Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 5
Visual Outcome of Anterior Uveitis in a Tertiary Hospital in South-East Nigeria
Apakama AI1*, Okosa MC1, Onwuegbuna AA1, Amobi MC1 and Onuorah KC22Queen Elizabeth the Queen Mother Hospital, Margate, Kent, England
Apakama AI, Guinness Eye Centre, Onitsha, Nigeria, Email: akunneapakama@yahoo.com
Received: 21-Apr-2021 Accepted Date: May 18, 2021 ; Published: 25-May-2021, DOI: O
Abstract
Objectives: To determine the visual outcome of anterior uveitis following treatment in a tertiary hospital in South- East Nigeria. Methods: A 5-year retrospective analysis of the visual outcome of anterior uveitis in patients treated for anterior uveitis at a tertiary eye center. A proforma was used in retrieving information on socio-demographics, presenting visual acuity, ocular examination findings, Intraocular Pressure (IOP), duration of follow-up, type of treatments given, routes of drug administration, and complications recorded in the patients on every visit. Data obtained was analyzed using the Statistical Package for Social Sciences (version 23) with statistical significance at p<0.05. Results: One hundred and seventy-three patients (191 eyes) comprising 99 (57.2%) males and 74 (42.8%) females were analyzed. Their ages range from 7 to 82 years, a mean of 39.1 ± 17.8 years. Thirteen (7.5%) were children ≤ 16 years. Unilateral involvement occurred in 155 (89.6%) patients. Ciliary flush 127 (66.5%), and unreactive pupil 48 (25.1%) were the commonest presenting eye signs. Cataract 33 (17.3%) and posterior synechiae 23 (12.0%) were the commonest recorded complications. The majority was treated with only topical steroids and cycloplegics 162 (84.8%). On presentation, 63 (33.0%) and 19 (9.9%) eyes had severe vision loss and moderate vision loss respectively; while at 12 weeks with 13.6% follow-up, 12 (6.3%) and 3 (1.6%) eyes had severe vision loss and moderate vision loss respectively. Conclusions: Anterior uveitis has a fairly good visual outcome following treatment. Tackling issues related to vision loss from anterior uveitis should be directed at factors influencing late presentation to the clinic and poor adherence to follow-up visits.
Keywords
Visual outcome, Anterior uveitis, Hospital, Nigeria
Introduction
Uveitis, a sight-threatening disease, is the inflammation of the uvea [1]. Based on the ocular structures involved, uveitis is anatomically classified into anterior, intermediate, posterior, and panuveitis by the International Uveitis Study Group (IUSG) [2]. Anterior uveitis is defined as inflammation of the uvea, predominantly involving the iris and ciliary body [2].
Studies across the continents have reported anterior uveitis to be the commonest form of uveitis [3-8]. Globally, the annual incidence of uveitis is approximately 17-52 cases per 100,000 [2]. However, in most developed and underdeveloped countries, over half of these uveitic cases are anterior uveitis [3-8]. In Ethiopia and Nigeria, anterior uveitis accounts for 74.5% and 63.7% of all cases of uveitis respectively [6,7]. Anterior uveitis is recorded as the commonest ophthalmic emergency in a tertiary eye center in Nigeria [9].
The treatment of anterior uveitis can be medical or surgical [10]. Corticosteroids, cycloplegics, Non-steroidal antiinflammatory drugs, and immunosuppressive agents are the mainstay drug therapies in the management of noninfectious anterior uveitis [10]. Antimicrobial agents are used in the treatment of infectious uveitis [11]. Surgical intervention is usually indicated in the management of structurally complicated cases of anterior uveitis [10].
Despite anterior uveitis is a potentially sight-threatening disease, the commonest type of uveitis in most studies, and the commonest ophthalmic emergency in Nigeria; there is an amazingly paucity of epidemiologic data focused specifically on the visual outcome of anterior uveitis [1,3-9]. Hence, this study is aimed at determining the visual outcome following treatment in patients with anterior uveitis.
Materials and Methods
This is a retrospective analysis of all patients with anterior uveitis managed from January 2012 to December 2016 in a tertiary eye center. Ethical approval was obtained from the Nnamdi Azikiwe University Teaching Hospital Medical and Health research ethics committee (IRB approval number NAUTH/CS/66/VOL. 13/VER. III/91/2020/065) and adherence to the tenets of the Declaration of Helsinki was strictly observed. Inclusion criteria were patients diagnosed with anterior uveitis and followed up during the study period, while patients with no-repeat clinic visits were excluded from the study. A proforma was used in collecting data as relevant to the study from the case notes of eligible patients.
Information on socio-demographic which included the age, sex, and occupation of the patients were obtained. Ocular examination findings included presenting Visual Acuity (VA) taken with the Snellen’s chart, detailed findings on pen torch and slit lamp biomicroscope, serial Intraocular Pressure (IOP) measurements, and complications at first and follow up visits were recorded. The type of treatment instituted, and route of administration was also documented. Patients were treated with corticosteroids given via different routes (topical, periocular, and oral); topical or oral Nonsteroidal anti-inflammatory drugs; and topical mydriatics or cycloplegics. In addition to the medications for anterior uveitis, patients with elevated intraocular pressure were also on ocular hypotensive medications. However, the choice of agent used in the treatment of the patients was based on the clinical verdict of the managing doctor. The duration of follow-up visits for each patient was taken in week(s).
Data obtained was analyzed using the Statistical Package for Social Sciences (SPSS version 23) with statistical significance at p˂0.05.
Operational Definitions
• Anterior uveitis: Inflammation of the uvea with its primary site in the anterior chamber [2,12]
• Acute anterior uveitis: Attacks of sudden onset and duration ≤ 3months [12]
• Chronic uveitis: Persistent uveitis with relapse in less than 3 months after discontinuation of treatment [12]
• Moderate vision loss: Visual acuity of ≤ 6/18 to 6/36
• Severe vision loss: Visual acuity of ≤ 6/60 [12]
• Combination therapy: Medications other than drugs used in the direct treatment of anterior uveitis. This includes periocular and systemic drugs. It also includes patients who were on ocular hypotensive for the treatment of elevated intraocular pressure from uveitis
Results
One hundred and seventy-three patients (191 eyes) met the inclusion criteria, and they were further analyzed. Their ages ranged from 7 to 82 years, a mean of 39.1 ± 17.8 years and a median age of 34 years. Ninety-nine (57.2%) patients were less than 40 years of age, of which 13 (7.5%) were children ≤ 16 years. Only 2 (1.2%) were 80 years and above. There were 99 (57.2%) males and 74 (42.8%) females. The male-to-female ratio was 1.3:1. There was a statistically significant difference in both sexes between persons less than 40 years and those ≥ 40 years of age, (p=0.004); and in persons ≤ 16 years and those above 16 years of age, (p=0.038). The age and sex distribution of these patients are shown in Table 1.
Table 1: Age and sex distribution of patients with anterior uveitis
| Age (Years) | Male (%) | Female (%) | Total (%) |
|---|---|---|---|
| ˂10 | 3 (1.7) | 2 (1.2) | 5 (2.9) |
| 10-19 | 11 (6.4) | 3 (1.7) | 14 (8.1) |
| 20-29 | 23 (13.3) | 17 (9.8) | 40 (23.1) |
| 30-39 | 29 (16.7) | 11 (6.4) | 40 (23.1) |
| 40-49 | 12 (6.95) | 12 (6.95) | 24 (13.9) |
| 50-59 | 5 (2.9) | 16 (9.2) | 21 (12.1) |
| 60-69 | 8 (4.6) | 9 (5.2) | 17 (9.8) |
| 70-79 | 7 (4.1) | 3 (1.7) | 10 (5.8) |
| ≥ 80 | 1 (0.6) | 1 (0.6) | 2 (1.2) |
| Total | 99 (57.2) | 74 (42.8) | 173 (100.0) |
Most of the patients were gainfully employed, 117 (67.6%). There was no significant statistical difference between patients who were gainfully employed in males and females (p=0.317). The majority, 139 (80.3%) lived within 20 km from the hospital, with most men likely to reside within 20 km from the hospital (p=0.035). The patients were followed up for a period of 1 week to 16 weeks, with a mean duration of follow-up of 3.91 ± 2.89 weeks. Unilateral involvement was the commonest mode of presentation, 155 (89.6%), with a slightly higher occurrence in the right eye, 79 (45.7%) than the left eye, 76 (43.9%). Bilateral involvement occurred more significantly in females, with unilateral involvement were more in males, (p˂0.001).
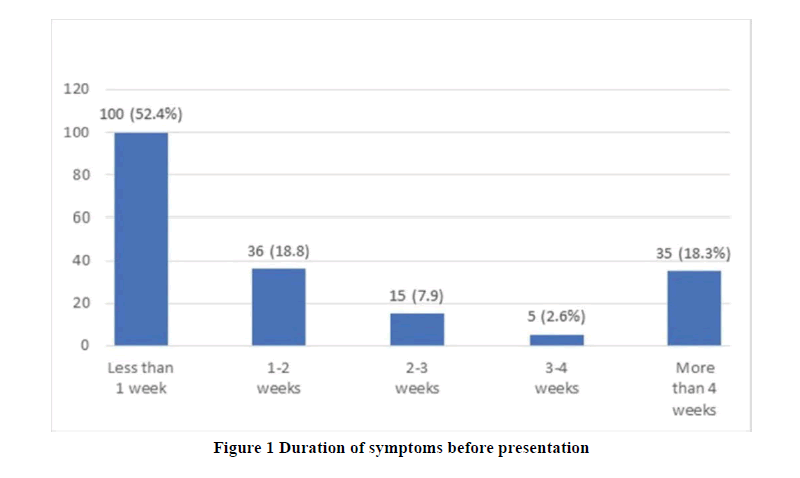
Figure 1 shows the duration of symptoms before presentation to the clinic. Presentation to the clinic within 2 weeks of the onset of symptoms is significantly higher in persons below 40 years of age, (p=0.007), but neither significant between adults and children (p=0.114), nor in both sexes (p=0.085).
The presenting signs seen in the eyes were ciliary flush 127 (66.5%), unreactive pupil 48 (25.1%), corneal haze 42 (22.0%), fresh KPs 32 (16.8%), lens opacity 23 (12.0%), irregular pupil 22 (11.5%), pigmented KPs 19 (9.9%), anterior chamber cells 18 (9.4%), anterior chamber flares 13 (7.5%), vitreous cells 4 (2.1%), and turbid aqueous 4 (2.1%).
On the clinical course, the majority of the eyes were acute 152 (79.6%), while recurrent and chronic clinical courses accounted for 17 (8.9%) and 22 (11.5%) of all eyes seen with anterior uveitis respectively. Chronic anterior uveitis is significantly higher in patients above 40 years (p=0.001), in those who reside more than 20 km from the hospital (p=0.036), those with severe vision loss (p˂0.001), and in those on combination therapy (p=0.001). The drug treatment and routes of administration are shown in Table 2.
Table 2: Drug treatment and routes of drug administration (eyes); NSAIDs: Non-Steroidal Anti-Inflammatory Drugs
| Routes of drug administration | No | Percentage (%) |
|---|---|---|
| Topical Therapy only | ||
| Steroids and cycloplegics | 120 | 74.1 |
| Steroids only | 42 | 25.9 |
| Total | 162 | 100.0 |
| Combination Therapy | ||
| Cycloplegics, topical steroids, and injectable steroids | 15 | 51.8 |
| Cycloplegics. topical steroids, and oral NSAIDs | 6 | 20.7 |
| Cycloplegics and oral NSAIDs | 3 | 10.3 |
| Cycloplegics, topical steroids, and oral steroids | 3 | 10.3 |
| Topical steroids and oral NSAIDS | 2 | 6.9 |
| Total | 29 | 100.0 |
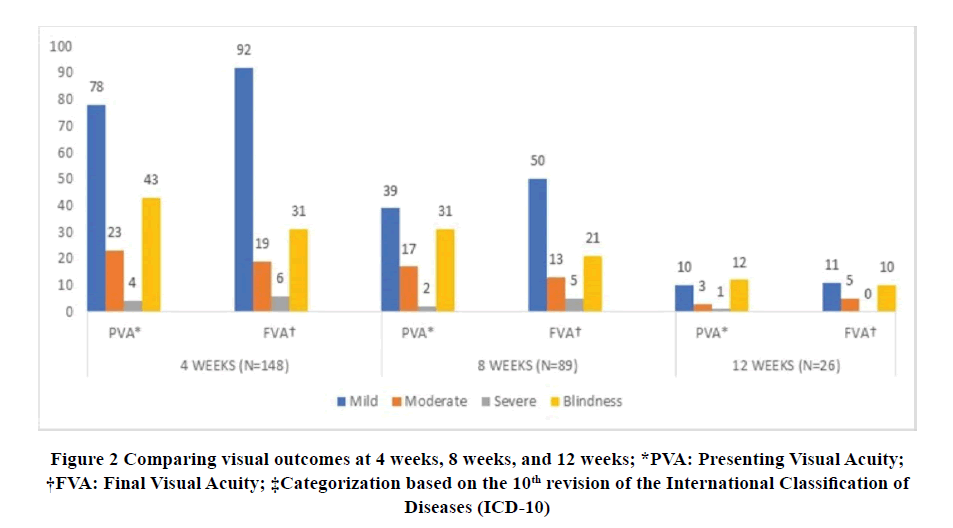
Comparison of the presenting visual acuity at the 4th week, 8th week, and 12th week in the eyes of patients that were followed up are presented in Figure 2.
Vision loss categorization according to the Standardization of Uveitis Nomenclature (SUN) working group is shown in Table 3.
Table 3: Comparing visual acuity (Vision loss)
| Visual Acuity (VA)* | Presenting visual acuity (eyes) | |||
|---|---|---|---|---|
| First visit | 4 weeks | 8 weeks | 12 weeks | |
| Moderate Visual Loss (˂6/18-6/36) | 19 (23.2) | 13 (23.2) | 9 (23.1) | 3 (20.0) |
| Severe Vision Loss (≤ 6/60) | 63 (76.8) | 43 (76.8) | 30 (76.9) | 12 (80.0) |
| Total | 82 (100.0) | 56 (100.0) | 39 (100.0) | 15 (100.0) |
*Categorization based on the Standardization of Uveitis Nomenclature (SUN) working group
There was a significant association between Severe Vision Loss (SVL) and age, a distance of abode from the hospital, duration of symptoms before presentation, and route of drug administration but not with sex, employment status. SVL was significantly associated with increasing age, being higher in patients above 40 years, (p˂0.001). There was a higher likelihood of SVL in patients living more than 20 km from the hospital, (p=0.001); in those with a duration of symptoms greater than 2 weeks before presentation, (p˂0.001) and in patients on combination therapy, (p=0.003). SVL was also significantly associated with complications such as posterior synechiae, (p=0.001); cataract, (p˂0.001); elevated intraocular pressure (p=0.044) and with optic atrophy (p=0.003). MVL was neither associated significantly with the demographics nor other factors. Presentation to the clinic within one week of onset of symptoms was significantly associated with mild or no visual impairment at 4 weeks (p=0.004), 8 weeks (p=0.008), and 12 weeks (p˂0.001) of follow-up visits.
Complications recorded during follow-up visits and their positive associations are shown in Table 4.
Table 4: Complications of anterior uveitis
| Complications | Frequency No. (%) | Associations | p-value |
|---|---|---|---|
| Cataract | 33 (17.3%) | Age of ˃40 years | p˂0.001 |
| Duration of more than 4 weeks before presentation | p=0.003 | ||
| Chronic uveitis | p˂0.001 | ||
| SVL | p˂0.001 | ||
| Combination therapy | p=0.012 | ||
| 12 weeks follow-up visit | p˂0.001 | ||
| Posterior synechiae | 23 (12.0%) | Living distance more than 20 km | p=0.012 |
| Duration of more than 4 weeks before presentation | p˂0.001 | ||
| Chronic uveitis | p=0.014 | ||
| SVL | p˂0.001 | ||
| 12 weeks follow-up visit | p=0.021 | ||
| Glaucoma | 14 (7.3%) | Chronic uveitis | p=0.007 |
| SVL | p=0.044 | ||
| Optic atrophy | 4 (2.1%) | Age of ˃40 years | p=0.033 |
| Living distance more than 20 km | p=0.032 | ||
| Duration of more than 4 weeks before presentation | p=0.020 | ||
| Chronic uveitis | p=0.002 | ||
| SVL | p=0.003 | ||
| Macula edema | 1 (0.5%) | ||
Discussion
Anterior uveitis is the leading cause of ophthalmic emergency seen in a tertiary hospital in Onitsha, South-East Nigeria; and the most common type of uveitis in Africa and most parts of the continents [3-9]. It is the commonest type of uveitis in all age groups [1]. Due to the paucity of literature focused on anterior uveitis alone, the different charts for visual acuity assessments, different cut-offs for age groups and visual impairments, and varying duration of follow-up visits in most patients; direct comparison of the present study with previous studies is difficult.
More than half of the patients treated for anterior uveitis within the period were below 40 years of age, with children less than 16 years of age accounting for less than 10%. This is similar to findings in Ekiti, south-western Nigeria where a person’s ≤ 16 years accounted for approximately 10% of all cases of anterior uveitis, with persons in their thirties being mostly affected [7]. Paivonsalo-Hietanen, et al. in Finland reported a 4.0% incidence of anterior uveitis per 100,000 populations per year in the age group less than 16 years old [13]. Also, Cunningham who reviewed several pieces of the literature concluded that children constitute about 5%-10% of all uveitis seen in tertiary facilities in most developing and developed countries [14]. However, a higher figure was recorded by BenEzra in Israel, where a third of the patients with uveitis occurred in person’s ≤ 18 years of age [15].
The follow-up of patients with anterior uveitis in most developed countries was for several years, which extended to a decade in some studies [16-19]. This could be due to increased systemic associations with anterior uveitis and the availability of diagnostic tools which is not widely available in this environment. In the present study, there was a progressive decline in the follow-up of patients from 77.5% at 4 weeks to 13.6% at 12 weeks. This is not surprising as Nwosu, et al. in the study area had recorded poor health-seeking behavior through the use of harmful practices in treating eye disease [20]. Iyiade, et al. in Ekiti, southwest Nigeria recorded a rapid decline in follow-up visits of patients with anterior uveitis over 12 weeks from their date of the first presentation to the clinic [7]. Also, Kizer-Akariwe reported a similar experience of poor adherence to follow-up visits of glaucoma patients in Enugu, a neighboring state to the study area in Nigeria [21]. The possible reason for non-compliance to follow-up visits was documented to be largely due to cost of utilization of the eye care services, distance from the hospital, and preference to receiving care in other facilities due to reasons like the discourteous attitude of hospital staff to patients [21]. This could also be due to the attitude and perception of eye diseases by people around this region [22].
The general aim of treatment of anterior uveitis is to control inflammation, reduce pain, prevent subsequent complications and most importantly restore good vision [10]. Despite the majority of the cases presenting to the hospital within 2 weeks of the onset of the disease and the acute type; however, in some patients, some attacks had previously occurred with complications being present even on their first visit to the clinic. Although studies have shown that anterior uveitis has a stable visual outcome; however, the unpredictability of the number of attacks, the course of the disease, and the possible long-term use of medications in the treatment of AU with their possible side effects could pose several challenges on the patient and the eventual visual outcome following treatment in this environment.
Approximately 30% and 40% of patients who were present for follow-up at 8 weeks and 12 weeks respectively had SVL. The older age groups, longer duration of symptoms before the commencement of treatment, place of abode farther to the hospital, were all associated with complications of anterior uveitis and severe vision loss in the present study. Patients who had SVL were mostly on combination therapy. Despite recording a significant number of patients with vision loss from anterior uveitis and its complications, however, this might not be permanent as further treatment of anterior uveitis and its complications have shown promising results in works of literature. Cataract which was the commonest complication recorded following treatment with anterior uveitis is strongly associated with severe vision loss in the present study. Okhravi, et al. in London demonstrated a significant improvement of the +4 Snellen line in visual acuity of eyes of patients with uveitis following cataract surgery [23].
Conclusion
Though presentation to the clinic within 2 weeks of the onset of symptoms seems early in our environment, it is pertinent to note that eyes that were treated within the first week of onset of symptom had a significantly better visual acuity of ≥ 6/18 at 4 weeks, 8weeks and 12 weeks of follow-up visits than those that presented after 1 week. Therefore, earlier presentation to the clinic is key in the management of this condition.
Declarations
Acknowledgment
Medical Record Staff of the Guinness Eye Centre, Onitsha.
Funding Sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of Interest
The authors declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
References
- de Smet, Marc D., et al. "Understanding uveitis: The impact of research on visual outcomes." Progress in Retinal and Eye Research, Vol. 30, No. 6, 2011, pp. 452-70.
- Gueudry, J., and M. Muraine. "Anterior uveitis." French Journal of Ophthalmology, Vol. 41, No. 1, 2018, pp. e11-21.
- Päivönsalo‐Hietanen, T., et al. "Uveitis survey at the University Eye Clinic in Turku." Acta Ophthalmologica, Vol. 72, No. 4, 1994, pp. 505-12.
- McCANNEL, Colin A., et al. "Causes of uveitis in the general practice of ophthalmology." American Journal of Ophthalmology, Vol. 121, No. 1, 1996, pp. 35-46.
- Wakefield, Denis, et al. "Uveitis: Aetiology and disease associations in an Australian population." Australian and New Zealand Journal of Ophthalmology, Vol. 14, No. 3, 1986, pp. 181-87.
- Tolesa, Kumale, et al. "Patterns of uveitis among patients attending Jimma University Department of Ophthalmology, Jimma, Ethiopia." Ocular Immunology and Inflammation, Vol. 28, No. 7, 2020, pp. 1109-15.
- Ajayi, I. A., O. J. Omotoye, and F. O. Adeleke. "Epidemiology of uveitis in a Nigerian Tertiary Eye Care Centre." Journal of Ophthalmic Research and Ocular Care, Vol. 3, No. 1, 2019, pp. 50-54.
- Borde, Prashant, et al. "Pattern of uveitis in a tertiary eye care centre of central India: Results of a prospective patient database over a period of two years." Indian Journal of Ophthalmology, Vol. 68, No. 3, 2020, pp. 476-81.
- Nwosu, Sebastian NN, et al. "Incidence and pattern of ophthalmic emergencies in Onitsha Nigeria." Nigerian Journal of Ophthalmology, Vol. 27, No. 1, 2019, pp. 29-32.
- Agrawal, Rupesh V., et al. "Current approach in diagnosis and management of anterior uveitis." Indian Journal of Ophthalmology, Vol. 58, No. 1, 2010, pp. 11-19.
- Lin, Phoebe. "Infectious uveitis." Current Ophthalmology Reports, Vol. 3, No. 3, 2015, pp. 170-83.
- Standardization of Uveitis Nomenclature (SUN) Working Group. "Standardization of uveitis nomenclature for reporting clinical data. Results of the First International Workshop." American Journal of Ophthalmology, Vol. 140, No. 3, 2005, pp. 509-16.
- Paivonsalo‐Hietanen, Taina, Juhani Tuominen, and K. Matti Saari. "Uveitis in children: Population‐based study in Finland." Acta Ophthalmologica Scandinavica, Vol. 78, No. 1, 2000, pp. 84-88.
- Cunningham, Jr, Emmett T. "Uveitis in children." Ocular Immunology and Inflammation, Vol. 8, No. 4, 2000, pp. 251-61.
- BenEzra, D., E. Cohen, and G. Maftzir. "Uveitis in children and adolescents." British Journal of Ophthalmology, Vol. 89, No. 4, 2005, pp. 444-48.
- Ozdal, Pinar C., Raul NG Vianna, and Jean Deschenes. "OAriginal article: Visual outcome of juvenile rheumatoid arthritis-associated uveitis in adults." Ocular Immunology and Inflammation, Vol. 13, No. 1, 2005, pp. 33-38.
- Tomkins-Netzer, Oren, et al. "Long-term clinical outcome and causes of vision loss in patients with uveitis." Ophthalmology, Vol. 121, No. 12, 2014, pp. 2387-92.
- Al-Ani, Haya H., et al. "Vision loss in anterior uveitis." British Journal of Ophthalmology, Vol. 104, No. 12, 2020, pp. 1652-57.
- Linssen, Annelise, and Christina Meenken. "Outcomes of HLA-B27-positive and HLA-B27-negative acute anterior uveitis." American Journal of Ophthalmology, Vol. 120, No. 3, 1995, pp. 351-61.
- Nwosu, S. N. N., and J. U. Obidiozor. "Incidence and risk factors for traditional eye medicine use among patients at a tertiary eye hospital in Nigeria." Nigerian Journal of Clinical Practice, Vol. 14, No. 4, 2011, pp. 405-07.
- Kizor-Akaraiwe, Nkiru N. "Follow-up and adherence to glaucoma care by newly diagnosed glaucoma patients in Enugu, Nigeria." Ophthalmic Epidemiology, Vol. 26, No. 2, 2019, pp. 140-46.
- Nwosu, S. N. N. "Beliefs and attitude to eye disease and blindness in rural Anambra State, Nigeria." Nigerian Journal of Ophthalmology, Vol. 10, No. 1, 2002, pp. 16-20.
- Okhravi, Narciss, Susan L. Lightman, and Hamish MA Towler. "Assessment of visual outcome after cataract surgery in patients with uveitis." Ophthalmology, Vol. 106, No. 4, 1999, pp. 710-22.