Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 5
Unusual Presentation of Methemoglobinemia in Child with COVID-19: Case Report
Fadiah AlMotairi1, Mohammed AlShamrani1, Awatif AlMutairi1, Ahmed AlEidan1*, Moatasem AlOufi1, Mazen AlGhofaily1 and Ahmed AlKhalifah22Children’s Specialised Hospital, King Fahad Medical City, Riyadh, Saudi Arabia
Ahmed AlEidan, Children’s Specialised Hospital, King Fahad Medical City, Riyadh, Saudi Arabia, Tel: 505472300, Email: ahmedaleidan@gmail.com
Received: 21-Apr-2021 Accepted Date: May 18, 2021 ; Published: 25-May-2021
Abstract
Given the increasingly rising reports over a potential association between COVID-19 and Methemoglobinemia that deserves a clinical attention to address it, we elected to describe a local experience of evident methemoglobinemia in a 2 year old child, who tested positive for COVID-19 throughout the course of his illness with active hemolysis and unknown Glucose-6-Phosphate Dehydrogenase status.
Keywords
Methemoglobinemia, COVID-19, Pediatric, MIS-C, G6PD
Introduction
Methemoglobin is a form of hemoglobin that has been oxidized, changing its heme iron configuration from the ferrous (Fe2+) to the ferric (Fe3+) state. Unlike normal hemoglobin, methemoglobin does not bind oxygen and as a result, cannot deliver oxygen to the tissues [1].
Methemoglobinemia is a rare disorder of the blood. Clinically significant methemoglobinemia occurs when there is an imbalance between two processes, increased production of methemoglobin or decreased reduction. Acquired causes of methemoglobinemia are more common than congenital causes. In some cases, an underlying genetic predisposition to methemoglobin formation can greatly exacerbate methemoglobinemia after exposure to an oxidant, namely, secondary to exposure to drugs or chemicals that oxidize hemoglobin and occasionally from pathologic conditions, such as sepsis, Glucose-6-Phosphate-Dehydrogenase Deficiency, and sickle cell crisis [2].
Following the outbreak of a novel coronavirus (SARS-CoV-2) associated with pneumonia in 2019, there is a current remark connecting it to Methaemoglobin (MetHb) augmentation in the serum [2]. Hence, we describe evident methemoglobinemia in a 2-year-old child, who tested positive for COVID-19 throughout his illness.
Case Report
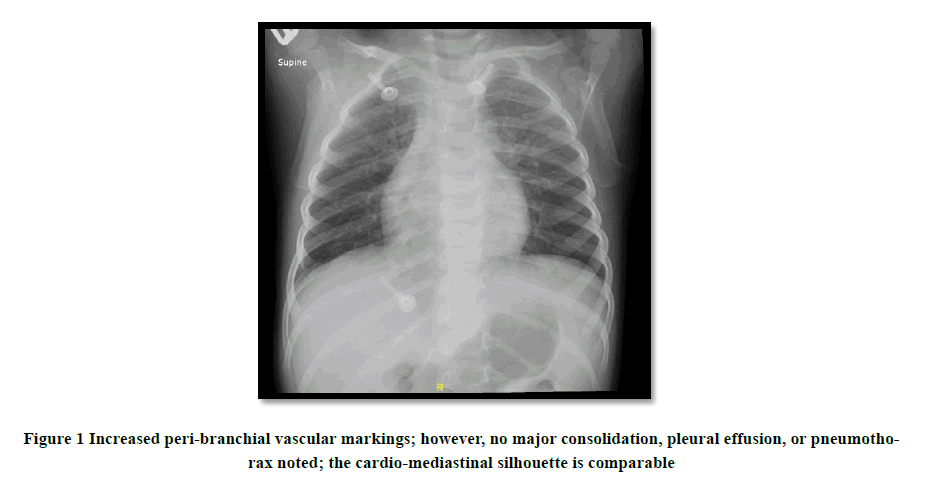
A 2-year-old male, who happened to be previously healthy tested positive for COVID-19 in the light of all family members being positive with very mild symptomatology. Four days later, he reported a 4-day-long constellation of fever, food content vomitus. Further, later on, he became hypoactive with a notable reduction in his oral intake. An observed paleness in conjunction with cola-colored urine appeared afterward. Upon presentation to the Emergency Department, he was found to have low Pulse Oximetry of 79% that did not respond to Low Flow Nasal cannula. Initial Capillary Blood Gases showed Methemoglobin of 7.6%, Hemoglobin of 4.4, Lactate of 3. Over a 48-hour Pediatric Intensive Care Unit stay, he was put on High Flow Nasal cannula of 15/L and received one Packed Red Blood Cells (PRBCs), following which, he improved significantly over one day with hydration only and antimicrobial therapy of Azithromycin to tackle his COVID infection. Of note, there is no family history of G6PD or hematological crisis with a similar presentation before. Notably, he was observed for a week with no suggestive signs of MultiSystem Inflammatory Syndrome in Children (MIS-C), yet evident hemolytic anemia that was not G6PD-explained. An expected repeat of G6PD testing after the resolution of the ongoing crises and residual effects of blood transfusion would be paramount in determining his disease status (Table 1 and Figure 1).
Table 1: Laboratory result
| Component Latest Ref Rng and Units | 23-03-2021 | 24-03-2021 | 24-03-2021 | 24-03-2021 | 25-03-2021 |
|---|---|---|---|---|---|
| Auto WBC >4.30 × 103/µL-<11.30 × 103/µL |
21.81 (H) | 23.20 (H) | 22.06 (H) | 25.67 (H) | 20.89 (H) |
| RBC >4.30 × 106/µL-<5.50 × 106/µL |
1.88 (L) | 3.01 (L) | 2.75 (L) | 3.39 (L) | 3.60 (L) |
| Hemoglobin 11.0 g/dL-15.0 g/dL |
5.1 (LL) | 8.4 (L) | 7.9 (L) | 9.9 (L) | 10.5 (L) |
| Hematocrit >35% -<45% |
16 (L) | 27 (L) | 24 (L) | 29 (L) | 32 (L) |
| MCV >75.0 fL-<95.0 fL |
85.6 | 88.4 | 86.5 | 86.7 | 87.8 |
| MCH >24.0 pg-<30.0 pg |
27.1 | 27.9 | 28.7 | 29.2 | 29.2 |
| MCHC >31 g/dL-<37 g/dL |
32 | 32 | 33 | 34 | 33 |
| RDW >11.0%-<15.0% |
17.0 (H) | 14 | 14.7 | 13.9 | 14.9 |
| MPV >6.3 fL-<11.2 fL |
9.3 | 9.7 | 10 | 9.9 | 11.3 (H) |
| Neutrophils Relative >30%-<70% |
53 | 31 | |||
| Lymphocytes Relative >25%-<75% |
25 (L) | 55 | |||
| Monocytes Relative >4%-<12% |
21 (H) | 13 (H) | |||
| Eosinophils Relative >1%-<12% |
1 (L) | 1 (L) | |||
| Neutrophils Absolute >1.35 × 103/µL-<7.50 × 103/µL |
10.55 (H) | 11.69 (H) | 7.97 (H) | 7.66 (H) | |
| Lymphocytes Absolute >1.90 × 103/µL-<4.90 × 103/µL |
5.44 (H) | 14.01 (H) | |||
| Monocytes Absolute >0.25 × 103/µL-<1.00 × 103/µL |
4.69 (H) | 3.29 (H) | |||
| Eosinophils Absolute >0.03 × 103/µL-<1.00 × 103/µL |
0.1 | 0.17 | |||
| Basophils Absolute >0.01 × 103/µL-<0.10 × 103/µL |
0.14 (H) | 0.23 (H) | |||
| Platelets 100 × 103/µL-450 × 103/µL |
297 | 262 | 259 | 254 | 94 (L) |
| nRBC% ≤0.00% |
6.80 (H) | 13.10 (H) | 19.90 (H) | 14.60 (H) | 11.90 (H) |
| ABSOLUTE NRBCS 109/L |
1.49 | 3.04 | 4.39 | 3.75 | 2.49 |
| Retic Ct Abs 103/µL |
119.4 | 143.6 | |||
| Immature reticulocyte fraction 103/µL |
43.2 | 41.2 | |||
| RETICS % >0.5%-<1.5% |
6.350 (HH) | 4.770 (HH) | |||
| LDH 125.00 U/L-220.00 U/L |
>1,995.00 (H) | ||||
| Ferritin 22.00 µg/l-275.00 µg/l |
>2,000.00 (H) | ||||
| POCT FMETHB,CAPILLARY 0.0%-1.5% |
7.6 (H) | 4.3 (H) | 2.2 (H) | 2.6 (H) | |
| COOMBS TEST, DIRECT, QUALITATIVE | Negative | ||||
| (DBS) GLUCOSE 6 PHOSPHATE DEHYDROGENASE ≥2.2 U/g Hp |
3.4 |
Discussion
The findings reported in the publications mirrored that MetHb can increase to dangerously high levels while contracting a severe COVID infection observed in some patients, particularly the critically ill ones. As dated to this moment, a total of seven publications (five case reports and two cross-sectional studies) were described in the literature linking methemoglobinemia to COVID-19 [3].
Kuipers, et al. reported a similar association in a 56-year-old man, who is known to have a clinical background of type II diabetes [4]. He was tested positive for COVID-19 in the light of presenting muscle pains and dry cough. Further, later on, he was required to be mechanically ventilated as he dropped his O2 saturation to 83% with a Computed Tomography (CT)-evident bilateral ground-glass opacities. Not to find later that his MetHB measured at 9.1% with hemolysis and a genetic deficiency of G6PD. He improved in 6 days following PRBCs and supportive care [3].
A local experience was mentioned by AlAamri, et al. describing a teenage girl with an age range of 10-to-15-year-old, who reported a clinical image about Kawasaki disease in the setting of COVID positivity 22 days before the reported presentation [5]. Unfortunately, she passed away on day 33 following aggressive management (Mechanical Ventilation “MV”, PRBCs, Antimicrobial therapy, and Tocilizumab and inotropes). Through which, she was found to have a MetHB level of (0.5%-1.9%) and G6PD-deficient [3].
Plamer, et al. reported a hypertensive and diabetic 62-year-old man, who presented with acute gastroenteritis and respiratory distress with febrile illness [6]. His COVID-19 screen returned positive. He was medicated with fluids, PRBCs, and antibiotics. His MetHB was 6.8% on the sixth day of the hospital course, and his suspected G6PD was confirmed as well [3].
Faisal, et al. published a report about a 74-year-old with prostate cancer, hypertension, and hyperlipidemia [7]. The old man tested positive for COVID-19 after presenting with a 7-day-long history of shortness of breath and fever. He was subjected to different lines of management as his course deteriorated from (Azithromycin and Hydroxychloroquine) to MV and inotropic support. On day 15, hypoxia was noted and his MetHB was high (6.3%), for which, the therapy of Methylene Blue was initiated and led to a significant drop from 15.9% to 2%. No known record of G6PD was mentioned [3].
Naymagon, et al. Alamdari, et al. wrote their reports in the literature as well [3,8,9].
In our perspective, the case we described is comparable in terms of initial presentation. However, the course is mild to what has been mentioned above. Nevertheless, we cannot ignore the similarities observed between ours and Kuipers. Of note, the status of G6PD in our patient is yet to be ascertained.
Conclusion
Although not fully understood, the association of Methemoglobenmia and COVID-19 infection is described across various reports. This genuine remark seemed proven after our own experience. An area of research is that where G6PD is the concealed condition underlying the abovementioned connection. Hence, we urge physicians, and Paediatricians, in particular, to recognize the relationship that existed in between and conduct further studies to comprehend the pathophysiological basis lying behind it.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Considerations
Written consent was obtained and signed by the legal guardians of the baby for full disclosure while maintaining strict confidentiality in respect to the patient medical information and images under the approval of the King Fahad Medical City (KFMC) research centre ethical committee.
References
- Prchal, JT. “Methemoglobinemia” UpToDate. https://www.uptodate.com/contents/methemoglobinemia?search=methemoglobinemia&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1
- Faisal, Hina, Alexi Bloom, and A. Osama Gaber. "Unexplained methemoglobinemia in coronavirus disease 2019: A case report." A&a Practice, Vol. 14, No. 9, 2020, p. e01287.
- Scholkmann, Felix, et al. "The role of methemoglobin and carboxyhemoglobin in COVID-19: A review." Journal of Clinical Medicine, Vol. 10, No. 1, 2021, p. 50.
- Kuipers, Maria T., et al. "G6PD deficiency‐associated hemolysis and methemoglobinemia in a COVID‐19 patient treated with chloroquine." American Journal of Hematology, 2020.
- Al-Aamri, Maryam Ali, et al. "A saudi G6PD deficient girl died with pediatric multisystem inflammatory syndrome-COVID-19." MedRxiv (2020).
- Palmer, Kieran, et al. "Methemoglobinemia in patient with G6PD deficiency and SARS-CoV-2 Infection." Emerging Infectious Diseases, Vol. 26, No. 9, 2020, pp. 2279-81.
- Faisal, Hina, Alexi Bloom, and A. Osama Gaber. "Unexplained methemoglobinemia in coronavirus disease 2019: A case report." A&a Practice, Vol. 14, No. 9, 2020, p. e01287.
- Naymagon, Leonard, et al. "The emergence of methemoglobinemia amidst the COVID‐19 pandemic." American Journal of Hematology, 2020.
- Alamdari, Daryoush Hamidi, et al. "Application of methylene blue-vitamin C-N-acetyl cysteine for treatment of critically ill COVID-19 patients, report of a phase-I clinical trial." European Journal of Pharmacology, Vol. 885, 2020, p. 173494.