Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 3
Under-Recognition of Radiologist Contributions in Case Reports of Jaw Lesions
Hanadi M. Khalifa1* and Haifa M Alharbi22General Dentist, KSA
Hanadi M. Khalifa, Oral and Maxillofacial Radiology Division, Department of Oral Diagnostic Sciences, Faculty of Dentistry, King Abdulaziz University, Jeddah, Saudi Arabia, Email: hmkhalifah@kau.edu.sa
Received: 10-Feb-2021 Accepted Date: Mar 24, 2021 ; Published: 31-Mar-2021
Abstract
Background: Diagnostic accuracy requires a correlative assessment of clinical, radiographic, and histologic findings. Jaw lesions with rare clinical features, imaging, laboratory, and/or histopathology findings are often communicated to the scientific community in the form of case reports. We have observed case reports of jaw lesions in which a radiographic interpretation frames an important part of the scientific article but radiologists were not identified or recognized as co-authors. Aim: The purpose of this study was to evaluate radiologists’ recognition in case reports involving jaw lesions. Methods and Materials: The PubMed database was searched for jaw pathology case reports. Inclusion criteria included case reports of jaw lesions containing radiographic images. Exclusion criteria include case reports in which all authors were radiologists; case reports where authors’ affiliation(s) could not be identified, and case reports with a focus on the surgical management of jaw pathology. Results: Of the 250 articles examined, radiologists were listed as co-authors or acknowledged in 18.8% and 0.8% of case reports, respectively. Advanced images were included in 82.2% of the case reports. Oral and maxillofacial surgeons and pathologists were authors in 71% and 58% of the case reports, respectively. Conclusion: Radiologists are extremely under-recognized in published case reports of jaw lesions. A fair and honest collaboration between clinicians, radiologists, pathologists, and dental specialists is crucial to serving the scientific community better and enriching the learning experience.
Keywords
Radiologists, Collaboration, Authorship, Case reports
Introduction
Human jaws can be affected by heterogeneous groups of clinically, radiographically, and histopathologically diverse lesions, ranging from normal variants to malignant neoplasms [1,2]. Obtaining an accurate diagnosis is an essential step in ensuring the most effective management; however, reaching this diagnosis requires a correlative assessment using clinical, radiographic, and histopathologic findings. In most cases, the histopathologic diagnosis is the foundation on which the decision regarding disease management and prognosis are based. However, the importance of radiographic interpretations and correlation with the histopathologic diagnosis cannot be underestimated [3].
Diagnostic imaging is a crucial tool for the correct clinical management of most pathology. Advanced imaging modalities such as Multi-Detector Computed Tomography (MDCT), Cone Beam Computed Tomography (CBCT), Magnetic Resonance Imaging (MRI), and nuclear imaging are useful in precisely delineating the extent of a lesion [2,4-6]. Some imaging features are indicative of a particular condition, and in those cases the diagnosis can be made entirely based on imaging [7]. Imaging features of certain lesions, however, are non-specific. In these cases, advanced imaging may allow the clinician to differentiate between different disease categories, such as benign versus malignant neoplasms, through a set of specific imaging features. Furthermore, advanced imaging is vital for staging, assessing the response to therapy, and providing ongoing tumor surveillance in cases of malignant neoplasms. MRI is particularly useful in demonstrating the perineural spread of malignant neoplasms as well as lymph node involvement. MDCT and MRI imaging may also be required when soft tissue characterization is necessary [2,8]. If a biopsy is indicated, diagnostic imaging may be useful in determining the best biopsy site. In some instances where the imaging features are not typical for histopathologic diagnosis, an additional biopsy may be recommended based on imaging.
Jaw lesions with rare clinical features, imaging, laboratory, and/or histopathology findings are often communicated to the scientific community in the form of case reports. Case reports need to show a close multidisciplinary approach to provide the best possible interpretation for these challenging cases. They can explain crucial scientific findings that may be overlooked or not observed in other forms of studies, and thus provide unique medical perspectives to extend the knowledge base of the scientific community [9-12].
In medical literature, several studies have investigated the issue of the under-recognition of radiologists and pathologists in published case reports [13-15]. A study by Manojlovic, et al. found that pathologists and radiologists were not acknowledged or attributed as co-authors in 46.2% and 83.5% of the examined studies, respectively [13]. Furthermore, Luyckx, et al. investigated how often a radiologist is recognized as a co-author in case reports containing radiological images and found that only 21% of the case reports included a radiologist as a co-author and 3% in the acknowledgments [14]. Similarly, Franko, et al. showed that radiologists were not attributed as authors or acknowledged in 72% of the case reports reviewed [15].
We have observed case reports concerning jaw lesions in which a radiographic interpretation, including published diagnostic imaging with detailed figure legends, frames an important part of the scientific paper, but radiologists were not acknowledged or recognized as co-authors. In these cases, it is not clear who ensured the integrity of the radiographic content. Therefore, the purpose of this study was to investigate the recognition of radiologists as authors in case reports involving jaw lesions.
Materials and Methods
The PubMed database was searched for case reports describing jaw lesions. The MeSH term used for the search was “jaw lesions,” and the search was restricted to human studies published in English over ten years from 1 January 2010 to 31 December 2019. This study included case reports regarding jaw pathology that also contained radiographic images. The following were excluded: case reports in which all authors were radiologists, case reports where authors’ affiliation(s) could not be identified, and case reports with a focus on the surgical management of jaw pathology. The following data were collected: the year of publication, the origin of the case reports, the specialty of the authors, the total number of authors, the presence of radiologists as co-authors, any mention of radiologists in the acknowledgments, the number and types of radiographic images, and lesion and/or disease categories. The medical or dental specialty of the authors was identified through screening the first or last page of the studies. Further online searching was conducted for some studies where the authors’ specialty could not be determined.
Data were statistically analyzed using IBM SPSS for Windows version 23.0 (IBM Corp, Armonk, NY). Simple descriptive statistics were used to describe the study variable’s characteristics in terms of counts, percentages, means, and standard deviations. The Z-test was used to assess differences between the recognized and omitted radiologists and a probability value of <0.05 was considered statistically significant.
Results
Characteristics of the Included Case Reports
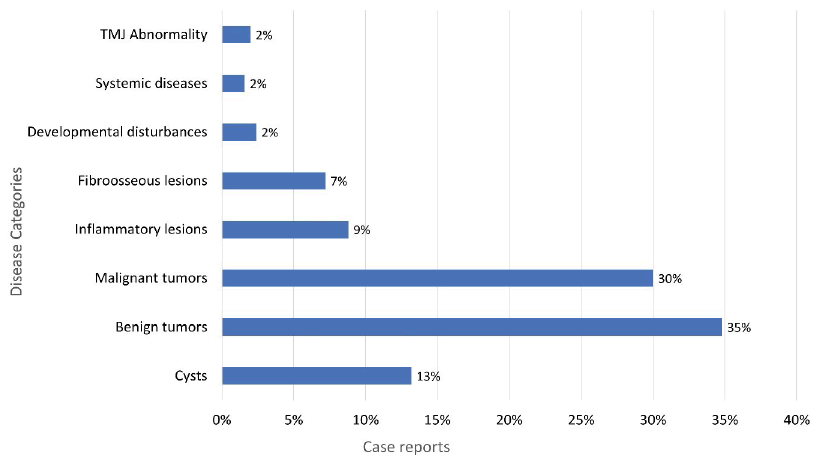
The initial PubMed search yielded 931 articles. The first 250 case reports that fulfilled the inclusion criteria were selected. One-fifth of the selected case reports were published in 2017 (20.5%), and the majority of the case reports were from Asia (38%), followed by Europe (22%). The characteristics of the case reports which were selected are shown in Table 1. The studies included reported various jaw lesions, most of which were benign (n=87) and malignant tumors (n=75). The percentage of the different disease categories reported in the included case reports is demonstrated in Figure 1.
| Case Reports (n=250) | n (%) | |
|---|---|---|
| Origin | Africa | 5 (2) |
| Asia | 94 (38) | |
| Australia | 8 (3) | |
| Europe | 56 (22) | |
| Middle east | 43 (43) | |
| North America | 30 (14) | |
| South America | 14 (6) | |
| Year | 2010 | 14 (5.6) |
| 2011 | 31 (12.4) | |
| 2012 | 17(6.8) | |
| 2013 | 26 (10.4) | |
| 2014 | 13 (5.2) | |
| 2015 | 10 (4) | |
| 2016 | 19 (7.6) | |
| 2017 | 51 (20.5) | |
| 2018 | 38 (15.2) | |
| 2019 | 31 (12.4) | |
Radiologist Contribution in Authorship
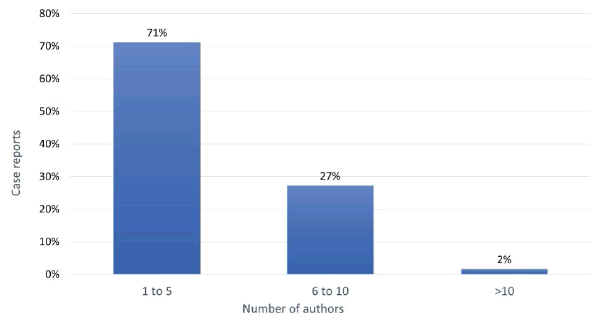
The number of authors per study ranged from to 2-13 (mean ± standard deviation was 4.6 ± 1.8 authors). Five or fewer authors were listed in 71% of the case reports examined, and the percentage of case reports for each number of authors is shown in Figure 2.
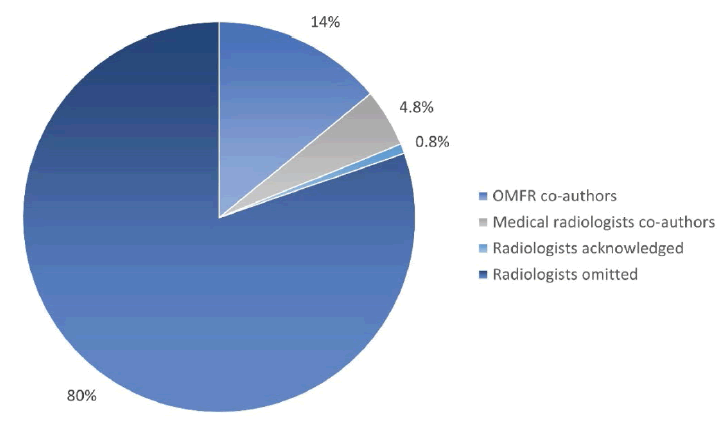
Radiologists were listed as authors in 47 (18.8%) of the examined case reports; among them, 35 (14%) were Oral and Maxillofacial Radiologists (OMFR) and 12 (4.8%) were medical radiologists. Radiologists were mentioned in the acknowledgments section in less than 1% of the studies (n=2) and were not listed as authors or recognized in the acknowledgments in 201 (80.4%) of the examined case reports. There were significantly fewer case reports in which radiologists were listed as co-authors or acknowledged compared to more case reports in which radiologists were omitted (Z= -13.595; p<0.001). Figure 3 demonstrates the percentage of radiologists’ authorship in the included case reports.
OMFRs was listed as the first author in 14 cases (40%), and a total of 28.5% of the case reports with OMFRs were published in radiology journals (Table 2). The authors for most of the examined case reports were either oral and maxillofacial surgeons (71%) or pathologists (58%). Figure 4 shows the dental and medical specialties of the authors for the included case reports.
| Author | Number | A study published in the radiology journal | Radiologist listed as the first author |
|---|---|---|---|
| OMFR | 35 | 10 | 14 |
| Medical radiologists | 12 | 1 | 3 |
| Total | 47 | 11 | 17 |
Diagnostic Images
There were a total of 972 diagnostic images in the selected studies. The maximum number of diagnostic images for a single study was 16 (mean ± standard deviation was 3.8 ± 2.7 images per case report). The majority of the images were conventional dental radiographs, which were published in 171 studies (68.4%), while ultrasounds appeared the least (n=4). Table 3 shows the proportion of various diagnostic imaging modalities published in the studies. Conventional dental radiographs were the only included radiographic images in 43 case reports (17.2%), while advanced imaging was included in 207 (82.2%).
| Type of radiographs | Number | Frequency |
|---|---|---|
| Conventional dental radiograph | 171 | 68.40% |
| MDCT | 138 | 55.20% |
| MRI | 43 | 17.20% |
| CBCT | 37 | 14.80% |
| Nuclear Imaging | 18 | 7.20% |
| Ultrasound | 4 | 1.60% |
| Other radiographs | 16 | 6.40% |
Discussion
Case reports provide novel and intellectually challenging cases to the scientific community and also serve as effective case-based educational tools that foster learning. Case reports are also an excellent opportunity for collaboration between healthcare providers [12]. Most jaw lesions require multidisciplinary collaboration to ensure accurate diagnosis and treatment decisions. Almazrooa, et al. demonstrated that oral and maxillofacial pathologists consulted oral and maxillofacial radiologists to reach a diagnosis in 16% of their cases [3]. It is anticipated that a multidisciplinary collaborative approach to inpatient management is reflected in publishing case reports to make them more fruitful and useful. However, the results of our study found that there is a lack of collaboration between radiologists and clinicians in publishing these reports. Radiologists were included as co-authors in less than 20% of the case reports we examined and were acknowledged in less than 1% of these cases, even though all case reports contained diagnostic images and corresponding expert descriptions and interpretations. The results of our study are similar to those of both Manojlovic, et al., and Franko, et al. who found that radiologists were not listed as co-authors in 81.1% and 72% of the case reports reviewed, respectively [13,15].
The lack of collaboration with radiologists under-represents the vital role that this diagnostic specialty plays in the process of patient management. Moreover, when radiologists are omitted, who is then accountable for the accuracy and integrity of the radiology content [16]. Manojlovic, et al. mentioned that neglecting pathologists and radiologists in manuscripts as co-authors, while using diagnostic images and the subsequent interpretations made by them, presents a failure to confer credit and responsibility for the content to the right individuals [13]. The publication credits have therefore been attributed to the clinicians who were the first to publish the findings, rather than the physicians (pathologists or radiologists) who played a critical role in the diagnostic process [13].
The International Committee of Medical Journal Editors (ICMJE) recommends that eligibility for authorship is dependent on the fulfillment of four criteria: substantial contributions to the conception or design of the work, or the acquisition, analysis, or interpretation of data; drafting the work or revising it critically for important intellectual content; final approval of the version to be published; and agreement to be accountable for all aspects of the work. Those who meet all four criteria should be acknowledged as an author, and in reality, not all authors meet all four criteria [17-19]. It has been found that 35% of listed authors meet only one or two criteria [20]. Bavdekar mentioned that the ICMJE criteria have an inherent limitation of being “voluntary” in nature, and therefore are highly dependent on the ethics and values of the reporting individuals [21]. In our opinion, when diagnostic imaging with corresponding descriptions and interpretations constitutes a major component of a manuscript, the radiologist has contributed to the acquisition, analysis, and interpretation of the data, as well as having written part of the manuscript. However, radiologists were not even acknowledged in 99.2% of the case reports we examined.
It has been speculated that the lack of collaboration with radiologists in publishing is most likely because diagnostic images and imaging reports are usually available in patients’ medical records. Therefore, radiologists are not required to simply retrieve the data [13,15]. Also, the conventionally written radiology report is the primary method by which radiologists interpret the results of diagnostic imaging and communicate with the referral clinicians. This reporting method has greatly limited the number of face-to-face encounters radiologists have with clinicians [22,23].
We found that oral and maxillofacial surgeons (71%) and pathologists (58%) contributed as authors in most of the examined case reports. Training in the radiographic interpretation of jaw pathology is an integral component of most oral and maxillofacial surgery and oral and maxillofacial pathology training programs. Therefore, most surgeons and pathologists self-interpret diagnostic images and do not seek further consultation with radiologists. Nevertheless, advanced imaging goes beyond the basic radiology training of most clinicians, and is therefore only interpreted by radiologists. In this study, 82.2% of the studies contained advanced imaging, including MDCT (55.2%), MRI (17.2%), CBCT (14.8%), nuclear medicine (7.2%), and ultrasound (1.6%). Radiologists deal with imaging modalities of different complexities as well as a wide range of diseases. Many studies have investigated the influence of expertise in radiologic interpretation, and have found that there is a clear association between diagnostic accuracy and experience [24,25]. Radiologists, more than any other specialists, can provide detailed descriptions of imaging procedures and findings. Moreover, many quality issues were observed in the case reports, such as panoramic positioning errors; suboptimal image density and contrast; low image resolution; errors in image identification and view names; and even errors in image orientation. Luyckx, et al. found that image quality scores were significantly better in studies having a radiologist as a co-author [14].
Under-recognition of radiologists may also be due to the proliferating unethical practices of honorary, gifted or mutual admiration authorship [13]. Honorary authorship occurs when an individual is granted authorship despite their lack of contribution to a study, such as department heads or other senior members, believing that their association with the manuscript will increase the chances of it being accepted [26,27]. The prevalence of honorary authorship has been reported to range from 11% to 60% and is more likely to occur in articles with more than five authors. In our study, more than five authors were listed in the by-line in 29% of the examined case reports [21]. Moreover, authorship can be gifted to individuals who performed various non-author activities, or to colleagues for academic promotion. Mutual admiration authorship is another unethical practice of authorship in which two or more authors agree to list each other’s names on a manuscript despite the others having minimal or no contribution [26]. The omission of radiologists in published papers containing radiology-related intellectual content is considered ghost authorship, and should therefore be discouraged. Clinicians should collaborate with radiologists and other specialists who are involved in patient management, for the drafting and critical evaluation of a manuscript when deciding to document a unique case.
In this study, 17.2% of the examined case reports contained only conventional radiographs. Among these, 8% were case reports of benign tumors, 2.4% were malignant tumors, and 0.8% were Benign Fibro-Osseous Lesions (BFOL). Conventional radiography is usually not adequate for the diagnosis of most jaw lesions and may result in misdiagnosis or mismanagement. Three-dimensional imaging is crucial for improving diagnostic accuracy and planning correct patient management. Advanced imaging provides information regarding the precise extent, features, and behavior of the lesion. Furthermore, advanced imaging is of paramount importance in the differential diagnosis of lesions that show similar histopathologic features, such as BFOL. For instance, the histopathologic diagnosis of fibrous dysplasia is known to be challenging because of its similarity to other forms of BFOL, osteomyelitis, and in some instances, welldifferentiated osteogenic sarcoma. Therefore, radiographic and histopathologic correlation is essential to differentiate between lesions that are extremely different in their treatment approach [28].
This study is not without limitations. Studies in which the first author listed was a radiologist and studies published in radiologic journals were not excluded, therefore, the rate of clinician and radiologist collaboration could be lower with stricter inclusion criteria. Also, the case reports we examined were heterogeneous about disease category and complexity. Many general clinicians are capable of describing the radiographic findings of uncomplicated cases, and some have received training to interpret CBCT imaging. Also, this study did not assess the effect of the radiologists’ contributions on the quality of the publication. The quality of the diagnostic images and figure legends as well as the integrity of the radiographic descriptions and interpretations were not evaluated. Finally, no attempt was made to assess the collaboration with pathologists and to compare the contribution of the two diagnostic specialties. These are areas for future research. More authorship recognition studies and ethics of publication are warranted to help influence under-recognition practices in scientific publications.
Conclusion
Although there is evidence of their contribution to the scientific manuscripts, radiologists are extremely underrecognized as co-authors of case reports regarding jaws lesions. Concerning research and publishing, a fair and honest collaboration between clinicians, pathologists, radiologists, and other specialists is crucial to better serve the scientific community and enrich the learning experience. We urge the editorial boards of scientific journals to develop and implement a contribution policy that mandates the involvement of a radiologist whenever radiology-related intellectual content is part of a published paper.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- MacDonald, David. "The most frequent and/or important lesions that affect the face and the jaws." Oral Radiology, Vol. 36, No. 1, 2020, pp. 1-17.
- White, Stuart C., and Michael J. Pharoah. "White and Pharoah's Oral Radiology E-Book: Principles and Interpretation." Elsevier Health Sciences, 2018.
- Almazrooa, Soulafa, et al. "The agreement rate between radiographic interpretation and histopathologic diagnosis of jaw lesions." Radiology Research and Practice, Vol. 2019, 2019.
- Meyer, Kathleen A., et al. "Imaging characteristics of benign, malignant, and infectious jaw lesions: A pictorial review." American Journal of Roentgenology, Vol. 197, No. 3, 2011, pp. W412-21.
- Fazaeli, Yousef, et al. "In vivo SPECT imaging of tumors by 198,199 Au-labeled graphene oxide nanostructures." Materials Science and Engineering: C, Vol. 45, 2014, pp. 196-204.
- Moradi, S., et al. "Magnetite/dextran-functionalized graphene oxide nanosheets for in vivo positive contrast magnetic resonance imaging." RSC Advances, Vol. 5, No. 59, 2015, pp. 47529-37.
- Omami, Galal. "Twenty classic signs in oral and maxillofacial radiology." Oral Radiology, Vol. 35, No. 1, 2019, pp. 3-10.
- Benson, Byron W., et al. "Advances in diagnostic imaging for pathologic conditions of the jaws." Head and Neck Pathology, Vol. 8, No. 4, 2014, pp. 383-91.
- Murad, M. Hassan, et al. "New evidence pyramid." BMJ Evidence-Based Medicine, Vol. 21, No. 4, 2016, pp. 125-27.
- Nissen, Trygve, and Rolf Wynn. "The clinical case report: A review of its merits and limitations." BMC Research Notes, Vol. 7, No. 1, 2014, pp. 1-7.
- Rison, Richard A. "A guide to writing case reports for the Journal of Medical Case Reports and BioMed Central Research Notes." Journal of Medical Case Reports, Vol. 7, 2013, pp. 1-9.
- Cromwell, Julia C., and Theodore A. Stern. "Publishing case reports: Educational strategies and content recommendations." Psychosomatics, Vol. 60, No. 4, 2019, pp. 361-64.
- Manojlovic-Gacic, Emilija, et al. "Bridging the gap with clinicians: The issue of underrecognition of pathologists and radiologists as scientific authors in contemporary medical literature." Science and Engineering Ethics, Vol. 26, No. 2, 2020, pp. 783-92.
- Luyckx, Elisa, et al. "Radiologists as co-authors in case reports containing radiological images: Does their presence influence quality?" Journal of the American College of Radiology, Vol. 16, No. 4, 2019, pp. 526-27.
- Franko, Angela D., James R. Wright Jr, and Martin J. Trotter. "Underrecognition of pathologist contributions to articles published in a major multidisciplinary medical journal." American Journal of Clinical Pathology, Vol. 138, No. 4, 2012, pp. 495-97.
- Hoey, John. "Who wrote this paper anyway?: The new Vancouver Group statement refines the definition of authorship." CMAJ, Vol. 163, No. 6, 2000, pp. 716-17.
- International Committee of Medical Journal Editors. "Defining the role of authors and contributors." 2018.
- Goodman, Neville W. "Survey of fulfilment of criteria for authorship in published medical research." BMJ, Vol. 309, No. 6967, 1994, p. 1482.
- Hwang, Seong Su, et al. "Researcher contributions and fulfillment of ICMJE authorship criteria: analysis of author contribution lists in research articles with multiple authors published in Radiology." Radiology, Vol. 226, No. 1, 2003, pp. 16-23.
- Slone, Richard M. "Coauthors' contributions to major papers published in the AJR: Frequency of undeserved coauthorship." AJR. American Journal of Roentgenology, Vol. 167, No. 3, 1996, pp. 571-79.
- Bavdekar, Sandeep B. "Authorship issues." Lung India: Official Organ of Indian Chest Society, Vol. 29, No. 1, 2012, p. 76.
- Gunn, Andrew J., et al. "Rethinking the role of the radiologist: Enhancing visibility through both traditional and non-traditional reporting practices." Radiographics, Vol. 35, No. 2, 2015, pp. 416-23.
- Glazer, Gary M., and Julie A. Ruiz-Wibbelsmann. "The invisible radiologist." Radiology, Vol. 258, No. 1, 2011, pp. 18-22.
- Waite, Stephen, et al. "Analysis of perceptual expertise in radiology-Current knowledge and a new perspective." Frontiers in Human Neuroscience, Vol. 13, 2019, p. 213.
- Gunderman, Richard, et al. "Expertise: Implications for radiological education." Academic Radiology, Vol. 8, No. 12, 2001, pp. 1252-56.
- Claxton, Larry D. "Scientific authorship: Part 2. History, recurring issues, practices, and guidelines." Mutation Research/Reviews in Mutation Research, Vol. 589, No. 1, 2005, pp. 31-45.
- Grobbee, Diederick E., and Rosemary Allpress. "On scientific authorship: Proliferation, problems and prospects." European Journal of Preventive Cardiology, Vol. 23, No. 8, 2016, pp. 790-91.
- Petrikowski, C. Grace, et al. "Radiographic differentiation of osteogenic sarcoma, osteomyelitis, and fibrous dysplasia of the jaws." Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology, Vol. 80, No. 6, 1995, pp. 744-50.