Research - International Journal of Medical Research & Health Sciences ( 2020) Volume 9, Issue 9
Unchanged Patient Attitude toward Spine Surgery despite about Two Decades of Practice at Tertiary Care Hospital
Waleed Awwad1, Rohail Mumtaz1*, Omar Alsultan1, Abdulaziz Aljurayyan1, Abeer Awwad2, Khalifah Aldawsari2, Abdulaziz Almaawi1 and Khalid Alsaleh12College of Medicine, King Saud University, Riyadh, Saudi Arabia
Rohail Mumtaz, King Saud University, Orthopaedic Surgery Department Riyadh, Saudi Arabia, Email: dr.rohael@gmail.com
Received: 04-Aug-2020 Accepted Date: Sep 21, 2020 ; Published: 28-Sep-2020
Abstract
Objective: Spine surgery carries a risk for the potential complications similar to any other surgical intervention. Our aim in this study to evaluate the patient attitude regarding spine surgeries and to understand the factors that could affect patient choice.
Methods: A cross sectional study of 164 patients who visited King Saud University Medical City (KSUMC) outpatient spine clinic between January to October 2019 and had a surgical pathology. Each patient and his family were counseled regarding the need of the spine surgery and the possible complications. A general demographic questionnaire was used to assess patient response toward surgery and to identify the factors which might influence his decision.
Results: A total of 164 patients were included in this study. Ninety-eight were females and sixty-six were males. Sixty-five (39.6%), agreed to surgery. The remaining ninety-nine (60.4%) didn’t opt surgery for different reasons. Conclusion: Despite that the spine surgery is as safe as any other surgical intervention patients tend to refuse it. We strongly believe that patient education is very important change this negative attitude. Patient’s understanding about the disease if left untreated or inappropriately treated may play a crucial role to make a better decision.
Keywords
Backache, Spine surgery, Patient attitude, Complications, Paralysis
Introduction
Backache is one of the commonest medical condition encountered in spine clinics. There are well established factors which are strongly associated with the backache. These factors can be enlisted as living style, obesity, work related, psychological and socio-economic characteristics [1]. Etiologies for back pain may vary from muscles spasm, sciatica, herniated or rupture disk, spinal stenosis, spinal deformities to cancer of the spine [2]. The overall lifetime prevalence of common (Non-specific) backache is about 60-70% in developed countries [3]. There is very limited research on the occurrence of low backache in Saudi Arabia. Al-Arfaj et al. have highlighted the factors and characteristics of the backache in Saudi population [4].
The management of low back pain universally starts with conservative measure if there are no red flags [5]. Conservative measures include physical therapy, general conditioning, back strengthening exercises, medications such as Nonsteroidal anti-inflammatory drugs (NSAIDs) and skeletal muscle relaxants. When conservative therapy fails, there comes the role of surgical intervention, which is usually required for a small number of patients. There are a variety of surgical procedures to deal with the low back problems, one procedure cannot be the solution for all the different problems. Most practiced surgical procedures are disc excision, decompressive laminectomy, fusion (instrumented or un-instrumented), or a combination of the above-mentioned procedures. It is very important to assess the expectations of patient and those must be given priority accordingly. Surgeon must set an achievable target which has to be very clear to both parties (Surgeon and patient). Like all other surgical procedures, spine surgery has possible complications. It has been observed widely that patients are much more concerned about the possible complications. As if any devastating complication happen such as loss of motor and sensory function can alter one’s life altogether [6].
It is utmost priority of the surgical team to take appropriate measures to avoid/reduce the incidence of such complications. Even in the literature, there’s a lot of variation about the complication associated to spine surgery. Possible explanation to this fact is that there are always differences in practice, experience of the surgeon and the patient samples among different studies. There is no much prospective work has been done to assess complications [3-6]. Community is still divided, and they do not have clear recommendations about potential risk factors which may cause complications in spine surgery [7-10].
The fear of complications keep patient deprived of optimal treatment in terms of surgical intervention and they may prefer living with disability even when they have a good chance to improve the quality of life [11]. The objective of this study is to assess the factors affecting patient’s decision making towards spine surgery.
Methods
From the practice of a single spine surgeon (WA), a total of 164 patients required spine surgery and attended the spine surgery outpatient, during January 2019 and October 2019. To be a surgical candidate, the patient must have clear and consistent symptoms. The clinical examination must correlate with the symptoms and radiological investigations must confirm the pathology. Furthermore, the patient must have tried nonsurgical options including physiotherapy, oral or local analgesia, and local steroid injection. Each patient underwent a structured interview by the treating surgeon. They must have a stable mental and psychosocial environment based on the absence of any mental or psychological problems in their past or present history. They must also be fit for general anesthesia. All the patients who needed surgery were sent to pre anesthesia clinic for assessment. American Society for Anesthesiologist (ASA) grading was used to assess fitness to surgery. All patients with grade I till III were considered fit while ASA classes IV and beyond were considered unfit. Lastly a questionnaire was given to the patients and labeled as surgical candidate with his clinical diagnosis and asked to submit it back prior to leave the clinic. The questionnaire had basic set of questions including demographic details (age, gender, level of educations, average monthly income) agree to surgery and refused, if refused state the cause of refusal. Statistical Package for the Social Science (SPSS) software, version 23 (SPSS Inc., Chicago, Illinois, USA) is used for data entry and analysis.
Results
A total of 164 patients were included in this study. Table 1 shows details about demographic data. Ninety-eight were females and sixty-six were males. Table 1 shows different variables which were included in questionnaire. Their median age was 52 years (range 28-76). Thirty eight percent of the patients had high degree of educations (Bachelor or above). Sixty two percent were married 38% were single (Unmarried, widowed and divorced). All 164 patients had a trial of conservative treatment. After that surgery was offered such as (discectomy, laminectomy, etc.).
| Variables | All Patients (N=164) | Accepted Surgery (N=65) | Rejected Surgery (N=99) |
|---|---|---|---|
| Average age (Years) | 52 | 50 | 54 |
| Male to female ratio | 98:66 | 42:23:00 | 56:43:00 |
| Average Education level | Undergraduate | Graduates or above | Higher secondary School |
| Married to unmarried ratio | 102:62 | 47:18:00 | 55:44:00 |
| Average monthly income in Saudi Riyals | <5K | 5-10K | <5K |
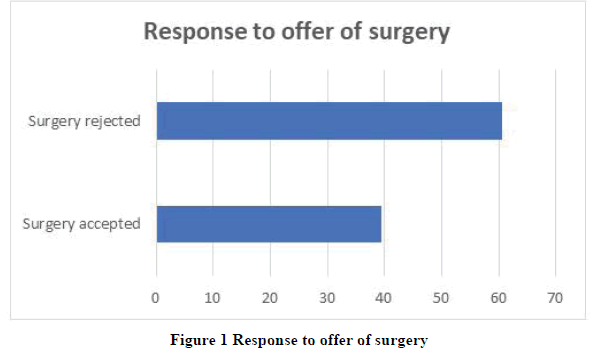
Among the group of 164 surgical patients, only 65 (39.5%) agreed to surgery. The remaining 99 (60.5%) preferred not to do surgery for various reasons. Figure 1 displays the response to surgical treatment.
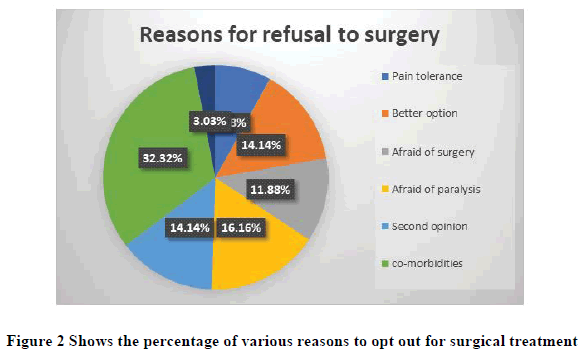
Figure 2 shows various reasons for refusal to surgery. These include living with the pain is fine in 8 (4.8%) patients, the thought that there is better option in 14 participants (8.5%), fear of surgery in 12 participants (7.3%), fear of complications such as paralysis in 16 (9.7%), looking for second opinion in 14 (8.5%). I have a lot of comorbidities in 32 (19.5%). I don’t believe in surgical interventions in 3 (1.8%).
Discussion
Low back pain and the resultant disability can be acute in some conditions such as acute disk prolapse, cauda equina syndrome, some infections and tumors. However, a large number of affected populations, especially who have degenerative problems, the onset and progression of symptoms is slow and may take years before really become disabling [12]. Most of the middle age to elderly population in Saudi community has a sedentary lifestyle. The prevalence of physical activity is different in various parts of the world, the highest activity level was noted among Scandinavian people, and the lowest in Brazil, Thailand and Kingdom of Saudi Arabia. Sporting activities and active pursuits are not very popular among them. In many instances, social and economic factors such as the availability of immediate help at home in the form of family members or hired domestic helper also play a significant role to potentiate the sedentary living. Above mentioned factors and the natural history of the chronic low back problems lead many patients to accept their symptoms and disability as part of the natural aging process.
Lack of proper knowledge, misunderstanding of the disease, the treatment options, misinformation about the spine surgery and possible related complications may in turn make them reluctant to undergo surgical treatment for their conditions even when they need it. A similar study by Behairy et al., back in 2003 showed the acceptance rate to spine surgery in Riyadh around 44% [12]. We were expecting better results as now people are more educated and even surgical safety has improved significantly with more and more qualified, trained and specialized staff. Despite the strongly accepted fact all across the professionals that with careful patient selection, spine surgery has proved better in terms of pain relief and improved quality of life when compared to more commonly used nonsurgical treatment options. Many researchers has proved that the modern spinal surgery is safe, effective and carries a risk rate either comparable to other surgical disciplines or even lower than them. Valen and Rolfsen followed 350 patients who underwent low back surgery for 2-16 years, they found that the complications rate was 9.7%, most complications were not serious, and there was no mortality related to the surgery [13].
According to the results of Global burden of disease study (GBD) 2010, low back pain was among top ten high burden problems. Its Disability-adjusted life years (DALY) was even higher than many other concerning problems such as road traffic accidents related injuries, infectious diseases like (HIV and tuberculosis), malignancies (lung cancer) and chronic medical conditions chronic obstructive pulmonary disease (COPD). Prevalence of back pain in many developed countries such as United States (US) is still very high and approaches from 8% till even as high as 57% [14]. It is estimated that about one third of the people may experience disabling backache at a certain stage of his or her life [15]. It is well known that the backache is one of the major causes for absence from work due to disability, it is reported as high as 23.6% in some studies [16]. It is very difficult to estimate the exact incidence of low back pain because large number of the individuals had experienced significant backache until they approach early adulthood and symptoms may return over time. Problem doesn’t always affect only the grown-up population or the one’s at higher risk such as heavy manual laborers. The occurrence of backache in childhood and young adults has been estimated up to 58% [17]. In some studies one year incidence (from 12.8-13.8 years) is found to be 18.4 % in girls and 16.9 in boys [18]. One year incidence of first ever back pain reaches up to 15.4 % with a recurrence rate between 24-80% [19,20].
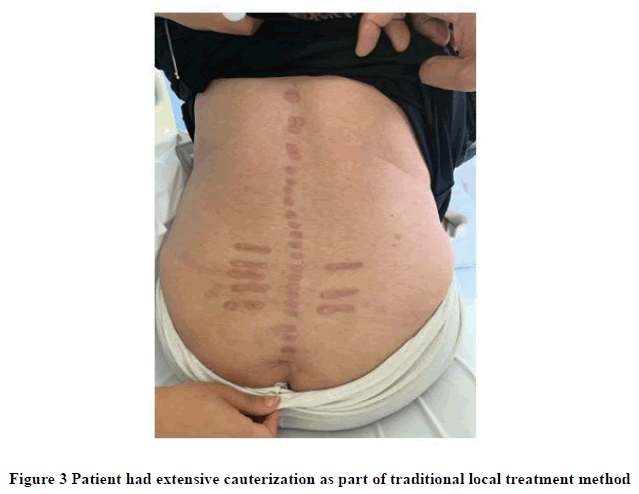
There is sufficient supporting data that those who have severe disabling symptoms they may be benefited the most from decompressive surgeries with or without fusion when compared with nonsurgical options [21,22]. But on many occasions, clinical trials are lacking technical aspects which are important to determine the safety of procedures and risks associated to them [23]. Many people would still opt for different conservative to invasive treatment options. Such as in alternative medicine forceful manipulation of the spine, cauterization and sometime venesection as well instead of surgery, even though all those poses significant risk of complication [24]. Figure 3 shows an example of extensive cauterization as a mode of local treatment for chronic painful conditions.
Despite the well-established view point that spinal surgery in comparison to other types of elective orthopedic surgery had an outstanding better ability to improve the operated subject’s health-related quality of life than other types of elective orthopedic surgery [25-27].
It is quite possible that other factors such as the specific institute and the specific surgeon might influence the patient’s decision to undergo low back surgery, our study still showed a high refusal rate (60.5%) for spine surgery among local patients. We were unable to determine any specific influencing factor.
Conclusion
Despite that the spine surgery is as safe as any other surgical intervention patients tend to refuse it. We strongly believe that patient education is very important change this negative attitude. Patient’s understanding about the disease if left untreated or inappropriately treated may play a crucial role to make a better decision.
Declarations
Ethics Approval and Consent to Participate
Study didn’t require IRB approval. All the patients were consented to participate in the study.
Consent for Publication
Written informed consent was obtained from all patients for publication. Copy of the written consent is available for review upon request.
Availability of Data and Materials
The datasets used and analyzed during the current study are available from the corresponding author upon request.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors’ Contributions
WA reviewed the final version of the manuscript. RM contributed to the study design and manuscript preparation and performed the literature review and statistical analysis. KA, OA and AJ contributed to the study design and manuscript preparation. AW and KA contributed to the study design and data collection. WA contributed to the manuscript preparation and data collection. RM contributed to the manuscript preparation and data collection. All authors read and approved the final manuscript.
Acknowledgements
The authors sincerely thank King Saud University, Vice Deanship of Research Chairs, and Research Chair of Orthopedic Surgery for their enthusiastic assistance.
Conflicts of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Allegri, Massimo, et al. "Mechanisms of low back pain: A guide for diagnosis and therapy." F1000 Research, Vol. 5, 2016, pp. 1-10.
- Wong, Arnold YL, Jaro Karppinen, and Dino Samartzis. "Low back pain in older adults: Risk factors, management options and future directions." Scoliosis and Spinal Disorders, Vol. 12, No. 1, 2017, p. 14.
- Bos, Ellen, et al. "Risk factors and musculoskeletal complaints in non-specialized nurses, IC nurses, operation room nurses, and X-ray technologists." International Archives of Occupational and Environmental Health, Vol. 80, No. 3, 2007, pp. 198-206.
- Al-Arfaj, Abdurhman S., et al. "Musculoskeletal pain in the community." Saudi Medical Journal, Vol. 24, No. 8, 2003, pp. 863-7.
- Alsaleh, Khalid A., et al. "Acute back pain: A survey of primary health care physicians’ awareness and knowledge of" Red Flag" Signs." Saudi Journal of Medicine and Medical Sciences, Vol. 4, No. 1, 2016, pp. 15-8.
- Hart, Robert A., et al. "Comparison of patient and surgeon perceptions of adverse events after adult spinal deformity surgery." Spine, Vol. 38, No. 9, 2013, pp. 732-6.
- Campbell, Peter G., et al. "Patient comorbidity score predicting the incidence of perioperative complications: Assessing the impact of comorbidities on complications in spine surgery." Journal of Neurosurgery: Spine, Vol. 16, No. 1, 2012, pp. 37-43.
- Campbell, Peter G., et al. "Comparison of ICD-9-based, retrospective, and prospective assessments of perioperative complications: Assessment of accuracy in reporting." Journal of Neurosurgery: Spine, Vol. 14, No. 1, 2011, pp. 16-22.
- Nasser, Rani, et al. "Complications in spine surgery: A review." Journal of Neurosurgery: Spine, Vol. 13, No. 2, 2010, pp. 144-57.
- Lee, Michael J., et al. "Risk factors for medical complication after spine surgery: A multivariate analysis of 1,591 patients." The Spine Journal, Vol. 12, No. 3, 2012, pp. 197-206.
- Atlas, Steven J., et al. "Surgical and nonsurgical management of lumbar spinal stenosis: Four-year outcomes from the maine lumbar spine study." Spine, Vol. 25, No. 5, 2000, pp. 556-62.
- Behairy, Yaser M., et al. "A survey of patient's attitude toward low back surgery in a major center in Saudi Arabia." Saudi Medical Journal, Vol. 24, No. 6, 2003, pp. 594-7.
- Valen, B., and L. C. Rolfsen. "Quality assurance of back surgery. A follow-up of 350 patients treated for sciatica by means of survival analysis." Tidsskrift for den Norske Laegeforening: Tidsskrift for Praktisk Medicin, ny Raekke, Vol. 118, No. 14, 1998, pp. 2136-9.
- Vos, Theo, et al. "Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: A systematic analysis for the Global Burden of Disease Study 2010." The Lancet, Vol. 380, No. 9859, 2012, pp. 2163-96.
- Manchikanti, Laxmaiah. "Epidemiology of low back pain." Pain Physician, Vol. 3, No. 2, 2000, pp. 167-92.
- Wynne-Jones, Gwenllian, et al. "Absence from work and return to work in people with back pain: A systematic review and meta-analysis." Occupational and Environmental Medicine, Vol. 71, No. 6, 2014, pp. 448-56.
- Kordi, Ramin, and Mohsen Rostami. "Low back pain in children and adolescents: An algorithmic clinical approach." Iranian Journal of Pediatrics, Vol. 21, No. 3, 2011, p. 259.
- Nissinen, Maunu, et al. "Anthropometric measurements and the incidence of low back pain in a cohort of pubertal children." Spine, Vol. 19, No. 12, 1994, pp. 1367-70.
- Balague, Federico, et al. "Non-specific low back pain." The Lancet, Vol. 379, No. 9814, 2012, pp. 482-91.
- Hoy, Damian, et al. "The epidemiology of low back pain." Best Practice and Research Clinical Rheumatology, Vol. 24, No. 6, 2010, pp. 769-81.
- Weinstein, James N., et al. "Surgical versus nonsurgical therapy for lumbar spinal stenosis." New England Journal of Medicine, Vol. 358, No. 8, 2008, pp. 794-810.
- Malmivaara, Antti, et al. "Surgical or nonoperative treatment for lumbar spinal stenosis: A randomized controlled trial." Spine, Vol. 32, No. 1, 2007, pp. 1-8.
- Chou, Roger, and Mark Helfand. "Challenges in systematic reviews that assess treatment harms." Annals of Internal Medicine, Vol. 142, No. 12, 2005, pp. 1090-9.
- Leung, Ping Chung. "The use of conservative and alternative therapy for low back pain." Medicines, Vol. 2, No. 3, 2015, pp. 287-97.
- Al-Hazzaa, Hazzaa M. "Physical inactivity in Saudi Arabia revisited: A systematic review of inactivity prevalence and perceived barriers to active living." International Journal of Health Sciences, Vol. 12, No. 6, 2018, p. 50.
- Al-Zalabani, Abdulmohsen H., Nasser A. Al-Hamdan, and Abdalla A. Saeed. "The prevalence of physical activity and its socioeconomic correlates in Kingdom of Saudi Arabia: A cross-sectional population-based national survey." Journal of Taibah University Medical Sciences, Vol. 10, No. 2, 2015, pp. 208-15.
- Hansson, Tommy, Elisabeth Hansson, and Henrik Malchau. "Utility of spine surgery: A comparison of common elective orthopaedic surgical procedures." Spine, Vol. 33, No. 25, 2008, pp. 2819-30.