Hypothesis - International Journal of Medical Research & Health Sciences ( 2022) Volume 11, Issue 12
To estimate the prevalence rate of early initiation of breast feeding within 1 hour of delivery and evaluate the factors influencing - A prospective observational study at a tertiary care hospital
Archana Sinha1, Minakshi Sinha1*, Sushant Kumar Sharma2, Sanjay Kumar3, Varsha Singh3, Rizwan Ahmar4 and Neeru Goel12Department of Surgery, Sri Krishna Medical College and Hospital, Bihar, India
3Department of Community Medicine, Indira Gandhi Institute of Medical, Sciences, Bihar, India
4Department of Paediatrics, Indira Gandhi Institute of Medical, Sciences, Bihar, India
Minakshi Sinha, Department of Obstetrics and Gynaecology, Indira Gandhi Institute of Medical Sciences, Bihar, India, Email: minakshi1512sinha@gmail.com
Received: 24-Nov-2022, Manuscript No. ijmrhs-22-81000; Editor assigned: 28-Nov-2022, Pre QC No. ijmrhs-22-81000 (PQ); Reviewed: 08-Dec-2022, QC No. ijmrhs-22-81000 (Q); Revised: 10-Dec-2022, Manuscript No. ijmrhs-22-81000 (R); Published: 30-Dec-2022
Abstract
Objective: To estimate the prevalence of early initiation of breastfeeding, and evaluate the factors influencing it. Methods: A prospective observational study was conducted in the department of Obstetrics and Gynecology at IGIMS, Patna with 205 participants after ethical approval. The details of mothers, including their sociodemographic profile, time and date, and mode of delivery along with the time of initiation of breastfeeding were noted. Apgar score and birth weight of the newborn was noted as well along with causes of delay in early initiation of breastfeeding. Results: The mean age was 26.13 years ± 3.89 years. 137 (66.7%) of the participants had a vaginal delivery. 68 (33.3%) of the participants had a cesarean delivery. 55 (80.9%) participants had a reason for the delay; either the mother or neonate became unstable, so timely breastfeeding could not be done. 13 (19.1%) of the neonates had a delay due to a lack of motivation from hospital staff. Conclusion: Early initiation of breastfeeding is not an easy feat. Our study has shown that counseling the hospital staff regarding the significance of early initiation of breastfeeding is as important as counseling the mother. Also, cesarean sections had more delays than vaginal deliveries.
Keywords
Breastfeeding, Early initiation, Colostrum, Prospective study, Delay in breastfeeding, Counselling
Introduction
Early initiation of breastfeeding within one hour after delivery is being promoted by WHO since 1990 [1]. It reduces postpartum hemorrhage, promotes bonding between the mother and her newborn, and provides nourishment to the newborn immediately. However though institutional deliveries have increased to up to 80%, the initiation of breastfeeding within one hour of delivery is only 41% in India [2]. Many factors like the custom of pre-lacteal feeds in a certain community, the stigma associated with “Colostrum”, maternal ignorance regarding the advantages of early breastfeeding, or the lack of motivation of hospital staff, contribute to this delay. This delay is seen more after cesarean deliveries as compared to vaginal births [3]. The difference is so great that it ranges from 49% after vaginal delivery to 22% after cesarean delivery [4]. As early initiation of breastfeeding reduces long-term infant morbidity and mortality, it is essential to know the factors that lead to delay in early initiation of breastfeeding after both vaginal delivery and cesarean section.
Aims and Objectives
• To estimate the average timing of initiation of breastfeeding after vaginal & cesarean deliveries.
• To evaluate the factors, causing the delay, if any
Method
A prospective observational study was done in the Department of Obstetrics and Gynaecology, Indira Gandhi Institute of Medical Sciences, Bihar, India, after ethical approval.
Operational definition-Early Initiation of Breastfeeding (EIBF) within 1st hour of birth.
Study Design
Prospective Observational Study
Sample Size
205
(Using formula of the single population proportion, 95% CI, 5% margin of error, and 49% prevalence of EIBF in institutional deliveries n = Z2 p(1-p) / e2
Inclusion Criteria
• All recently vaginally delivered healthy mothers with healthy babies i.e Apgar score >7.
• Healthy Mothers who had cesarean birth under regional anesthesia.
• Period of gestation in Obstetrics and Gynecology (POG) >34 weeks.
• Babies >1.75 kg with other normal parameters.
Exclusion Criteria
• Mothers of babies admitted to Neonatal Intensive Care Unit (NICU) for any reason. Babies with anomalies needing surgical correction like Diaphragmatic Hernia, Tracheoesophageal Fistula.
• Mothers who had cesarean birth under general anesthesia or who need ICU care.
• Eclamptic mothers.
• Mothers on Chemotherapy or antipsychotics.
After taking informed consent, patients were enrolled. The details of mothers, including their sociodemographic profile were noted. Time and date and mode of delivery along with the time of initiation of breastfeeding were noted [5-7].
Apgar score, birth weight, sex, and maturity of the neonate were noted. Any congenital abnormality requiring immediate surgical intervention was looked for. If there was any delay in the initiation of breastfeeding for a neonate, the cause for delay was looked at retrospectively. Descriptive statistics were used for baseline characteristics. Association between variables was done by logistic regression analysis [8].
Result
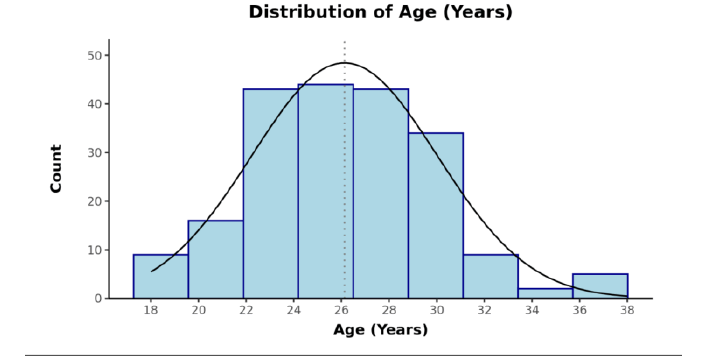
The mean age was 26.13 years ± 3.89 years (Figure 1).
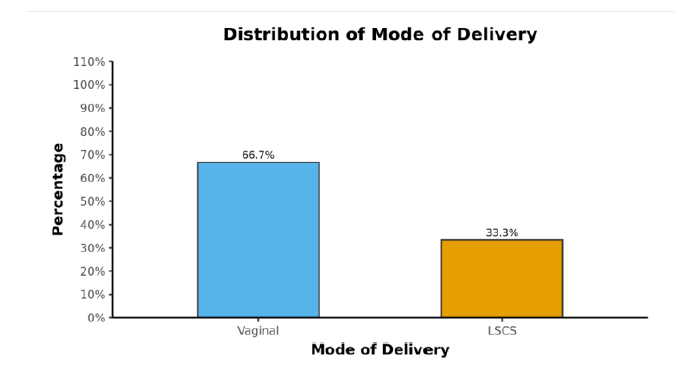
All of the participants had undergone Antenatal Care (ANC). 137 (66.7%) of the participants had a vaginal delivery. 68 (33.3%) of the participants had a cesarean delivery.
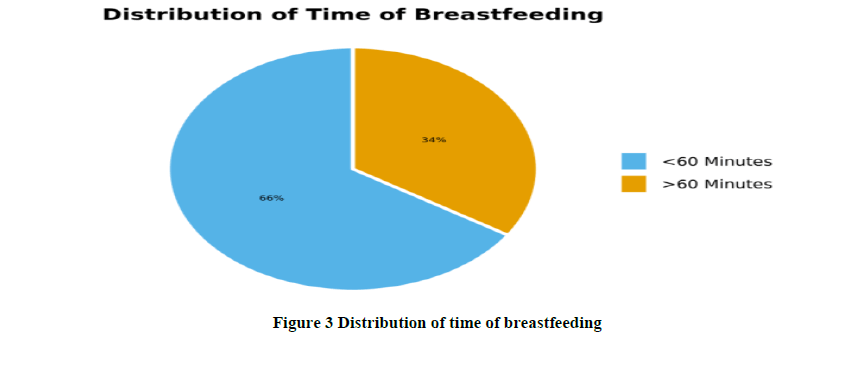
The mean Birth Weight was 2.83 ± 0.52. The mean Appearance, Pulse, Grimace, Activity, and Respiration (APGAR) (1 Minute) was 7.96 ± 1.13. The mean APGAR (5 Minutes) was 9.30 ± 0.83 (Figure 2). 135 (65.9%) of the participants breastfed their babies within one hour of birth.70 (34.1%) of the participants failed to do so (Figure 3).
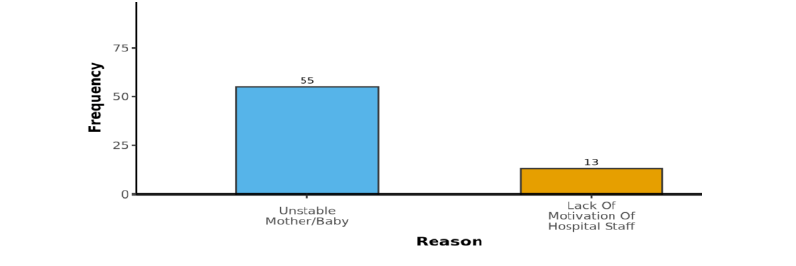
Cause of Delay
55 (80.9%) participants had a reason for the delay; either the mother or neonate became unstable, so timely breastfeeding could not be done. 13 (19.1%) of the neonates had a delay due to a lack of motivation from hospital staff (Figure 4).
1 (0.5%) of the neonate had a congenital anomaly. 30 (14.6%) of the neonates had NICU admission. The mean (SD) of APGAR (1 Minute) was 7.96 (1.13). The median Interquartile Range (IQR) of APGAR (1 Minute) was 8.00 (8-9). The APGAR (1 Minute) ranged from 3-10.
Discussion
The present study showed that the prevalence rate of EIBF was 66%. This is below the recommended 90% by WHO but much above the national average of 41.5% in the 2016 National Health Mission (NHM). In a study conducted by Bharani A. et al, only in 58% of deliveries, early initiation of breastfeeding could be practiced in their hospital. 75% of the participants knew about breastfeeding but only 60% knew the importance of Early Initiation of Breastfeeding (EIBF) [9].
Patel A showed that early initiation of breastfeeding was more in multiparous than primiparous women. They also showed that delay was more after cesarean deliveries [10].
Rajathi Sakthivel showed that exclusive breastfeeding was 39% in women >25 years while it was 14% in those <25 years of age [11].
Improvements in living standards and health infrastructure have increased institutional deliveries. However, still, early initiation of breastfeeding within one hour of delivery is not 100% even in institutional deliveries, like in the 35% delay in our study.
Lack of motivation of health professionals (19.1%) and new mothers were important factors in our study for the delay in EIBF. Delivery at night was the main deterrent for those with delays in this study.
According to a recent meta-analysis of five studies from four countries, including more than 130,000 breastfed newborns, those who began breastfeeding between 2 hours and 23 hours after birth had a 33% greater risk of dying compared with those who began breastfeeding within one hour after birth [12]. Among newborns who started breastfeeding 24 hours or more after birth, the risk was more than twice as high. The protective effect of early breastfeeding existed independently of whether or not the children were exclusively breastfed. Children who are not put to the breast within the first hour of life also face a higher risk of common infections. In a study of more than 4,000 children in Tanzania, the delayed initiation of breastfeeding was associated with an increased risk of cough and an almost 50% increased risk of breathing difficulties in the first six months of life, compared with newborns who began breastfeeding within the first hour of birth [13]
Conclusion
EIBF holds a key position in achieving the millennium development goals of reducing Under-5 mortality. Counseling of pregnant women during the antenatal period for EIBF will play an important role in this direction. Healthcare providers should also be trained and the labor room checklist should have a column for EIBF.
Initiating breastfeeding within the first hour of life is not easy. Mothers cannot be expected to do it alone. They require adequate support and guidance on positioning and feeding their newborns. The appropriate care of both newborn and mother in the moments after birth is critical to ensuring that breastfeeding not only begins but continues successfully. While a small proportion of women cannot breastfeed for medical reasons, most mothers simply need the right support at the right time to ensure that breastfeeding gets an early start.
Declarations
Strength
This was a prospective study. We could detect the cause of delay in EIBF in all patients. This will help us in making the necessary changes, to increase the rate of EIBF and prevent neonatal morbidity and mortality.
Conflict of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Limitations
It was a hospital-based study. The sample size was small, so the results may not reflect the general population. Still, the study helps in invoking a positive attitude in hospitals, so that a small change in the mindset of healthcare providers can prove beneficial to both the mothers and neonates.
Funding
This study was not funded.
Contribution of authors
All authors were involved equally since the inception of the protocol, data collection, analysis, and writing the final manuscript.
References
- Unicef, and WHO. "Capture the moment: early initiation of breastfeeding: the best start for every newborn." United Nations Children's Fund, 2018.
Google Scholar - Patel, Archana, et al. "Rates and determinants of early initiation of breastfeeding and exclusive breast feeding at 42 days postnatal in six low and middle-income countries: a prospective cohort study." Reproductive Health, Vol. 12, No. 2, 2015, pp. 1-11.
Google Scholar Crossref - Garcia, C. R., et al. "Breast-feeding initiation time and neonatal mortality risk among newborns in South India." Journal of Perinatology, Vol. 31, No. 6, 2011, pp. 397-03.
Google Scholar Crossref - Edmond, Karen M., et al. "Delayed breastfeeding initiation increases risk of neonatal mortality." Pediatrics, Vol. 117, No. 3, 2006, pp. e380-e86.
Google Scholar Crossref - Edmond, Karen M., et al. "Delayed breastfeeding initiation increases risk of neonatal mortality." Pediatrics, Vol. 117, No. 3, 2006, pp. e380-e86.
Google Scholar Crossref - Mullany, Luke C., et al. "Breast-feeding patterns, time to initiation, and mortality risk among newborns in southern Nepal." The Journal of nutrition, Vol. 138, No. 3, 2008, pp. 599-03.
Google Scholar Crossref - Debes, Amanda K., et al. "Time to initiation of breastfeeding and neonatal mortality and morbidity: a systematic review." BMC public health, Vol. 13, No. 3, 2013, pp. 1-14.
Google Scholar Crossref - Turfkruyer, Mathilde, and Valerie Verhasselt. "Breast milk and its impact on maturation of the neonatal immune system." Current opinion in infectious diseases, Vol. 28, No. 3, 2015, pp. 199-06.
Google Scholar Crossref - Wang, Haidong, et al. "Global, regional, national, and selected subnational levels of stillbirths, neonatal, infant, and under-5 mortality, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015." The Lancet, Vol. 388, No. 10053, 2016, pp. 1725-74.
Google Scholar Crossref - Neovita Study Group. "Timing of initiation, patterns of breastfeeding, and infant survival: prospective analysis of pooled data from three randomised trials." The Lancet Global Health, Vol. 4, No. 4, 2016, pp. e266-e75.
Google Scholar Crossref - Victora, Cesar G., et al. "Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect." The lancet, Vol. 387, No. 10017, 2016, pp. 475-90.
Google Scholar Crossref - Ogbo, Felix A., et al. "Infant feeding practices and diarrhoea in sub-Saharan African countries with high diarrhoea mortality." PloS one, Vol. 12, No. 2, 2017.
Google Scholar Crossref - Agho, Kingsley E., et al. "Trends and predictors of prelacteal feeding practices in Nigeria (2003–2013)." Nutrients, Vol. 8, No. 8, 2016, p. 462.
Google Scholar Crossref