Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 2
The Use of Herbs to Induce Labor among Pregnant Women and Associated Factors: A Cross-Sectional Study
Norah A. Alshehri*Norah A. Alshehri, King Saud University, Department of Family and Community Medicine, College of Medicine, Riyadh, Saudi Arabia, Email: drnorah19@gmail.com
Received: 30-Dec-2020 Accepted Date: Feb 11, 2021 ; Published: 18-Feb-2021
Abstract
Background: Many women are using herbs during pregnancy. Moreover, the literature reports the practice of pregnant women using herbs to induce labor. Worryingly, the prevalence, sources, and reasons of the herbs being used in labor are not established in Saudi Arabia, ultimately creating uncertainty for both pregnant women and physicians. Objective: The study aimed to determine the prevalence of herbal use among pregnant women with inducing labor, their sources, and the motivations underlying these practices. Methods: Using a convenient random sampling technique, 340 postpartum women were interviewed in a cross-sectional study. The study, which was approved by the Institutional Review Board, occurred between April and July 2019 at King Saud University Medical City (KSUMC) in Riyadh, Saudi Arabia. Results: Of the women interviewed, 31.5% had used herbs to induce labor, with a statistically significant association among women with age between 25 and 35 years old (p=0.003). The participants reported using herbs during labor because of a belief that they might shorten and ease labor. Conclusion: The findings show an alarming rate of herbal use to induce labor among full-term pregnant women associated with non-evidence-based medicine practices.
Keywords
Herbs, Women health, Pregnancy, Labor Induction
Introduction
Complementary and Alternative Medicine (CAM) is a group of diverse medical and health-care practices which are not presently considered part of conventional modern medicine [1]. Despite this, the trend for such practices and related products is increasing; a study found that the prevalence of CAM use ranges from 0.3% to 86% during a person’s lifetime [2].
In a large population study, it was found that the uses of CAM differed and depended on gender and socio-demographic variables [3]. Interestingly, there was a statistically significant finding that women have a higher likelihood of CAM use than men (53.5% vs. 42.7%) [4]. This has also been reported in another local study that was carried out at health care centers in Riyadh. It was reported that 46% of the patients had used Alternative Medicine (AM). Similarly, it was also reported that AM use was more prevalent among women, homemakers, and illiterate [5].
In women’s health, it is apparent that CAM is seen to play an important role, especially in the medical treatment of the female reproductive system [6]. One study which included 7427 women found that CAM is being used to alleviate premenstrual symptoms [7].
Meanwhile, in pregnancy, the prevalence of CAM varies widely and ranges from 7% to 55% depending on socio-cultural and ethnic considerations [8]. Among those who use CAM, many implement it for pregnancy-related back and pelvic pain [9]. Among Arab women, studies have reported that 56.7% reported using at least one form of CAM modality during pregnancy, while only a few users disclosed their CAM usage to physicians [10]. Most women preferred to use herbs because they believe these are natural, safer alternatives to medication (82.5%). Furthermore, around (91.7%) considered these therapies to be beneficial, with the majority (99.2%) reporting no apparent side effects [11].
Regarding the factor of belief within the community and literature, women also report the use of herbs as a common aspect of CAM practices for labor induction during pregnancy to reduce the length of labor and to make this process easier. However, these practices are often not recommended by medical professionals who cite the risk of miscarriage and premature labor [12].
There are pharmacological methods to induce labor, such as PGE2 and oxytocin, and mechanical methods, such as membrane sweeping, amniotomy, and Foley catheter hydrostatic pressure [13-15]. In contrast, non-pharmacologic approaches for labor induction include but are not limited to herbal compounds [16]. The use of herbs is becoming increasingly widespread, and some women look to herbs during pregnancy and childbirth for use alongside conventional medical practices [17].
It is less known about the prevalence of the use of herbs for labor induction in Saudi Arabia and the associated factors. It is the intention of this study to estimate the prevalence of herbs used for labor induction among full-term pregnant women, to test for associations with maternal characteristics, and to explore women’s reasons for using herbs while investigating their sources.
Materials and Methods
Research Design and Setting
This cross-sectional study explored herbs to use for labor induction among full-term pregnant women. Three hundred and forty women were asked to join the study at King Saud University Medical City (KSUMC) in Riyadh, Saudi Arabia. The participants were approached during their stay at the hospital between April to July 2019.
Subject and Sampling Method
A convenient random sampling technique using a validated questionnaire was developed by the researcher and administered by trained data collectors who carried out face-to-face interviews. Participants in this research (n=340) were all full-term women who were admitted as inpatients, women who had given birth within two days and were in the postnatal ward, or women who were 36 weeks pregnant or more. The participants were excluded if they were admitted for elective cesarean section, had intellectual disabilities, or were non-Arabic speakers (as this could have affected the interview process).
Sample Size
Based on previous literature, the sample size was calculated by using the single-proportion formula. Based on the premise that 10% of participants would not respond and prevalence is 33.7%, a conservative choice (p=0.05) has been employed. To ensure that the estimation error would be at most alpha 0.05 with 95% confidence, the sample size of 340.
Research Instrument
The questionnaire was developed by the principal investigator based on the study objectives following a literature review of a similar study [12]. A panel of two obstetricians and one family physician, all of whom provide clinical care for pregnant women, and are familiar with the survey’s development, assessed the questionnaire for appropriateness, accuracy, and relevance.
A pilot study on a sample of 40 participants was conducted before initiating the process of data collection. This was done to assess the feasibility and validity of the scale used as well as to estimate the amount of time required for data collection. The results of the piloted questionnaires were not included in the analysis.
The questionnaire consisted of 11 items in total, divided into three sections. There were five items in section one. These were presented as demographic characteristics and covered the women’s age, nationality, education, occupation, and household income in Saudi Riyal. There were three questions in the second section which addressed the participants’ obstetric history. Finally, the last section had three items that addressed the use of herbs with response choices of “Yes” and “No”, and two subsequent questions that followed up on the reasons for this usage and their sources.
Data Analysis
To understand and describe the characteristics and patterns of traditional herbal usage, descriptive statistics were used. Categorical variables were presented in terms of frequency and percentage. Continuous variables were presented as mean and Standard Deviation (SD). To identify the relationship between socio-demographic factors and the use of herbs, Chi-square tests were used. A p-value of ≤ 0.05 and 95% confidence intervals was used to report the statistical significance and precision of the results. Statistical Package for the Social Sciences (SPSS), IBM version 22 (SPSS Inc., Chicago, IL, USA) software was used for data analysis and management.
Ethical Considerations
Before commencement, the study was approved by the institutional review board at King Saud University (no. E-17- 2384). Additionally, a signed informed consent form was obtained from each participant. These were worded and indicated the purpose of the study. Confidentiality was assured by assigning each participant to a code number for analysis. No financial aid or awards were offered, nor was there any conflict of interest involved. Each respondent was given the right to refuse their participation in the study. The fact that their medical care would not be affected was also stressed.
Results
Participants’ Characteristics
The data presented in Table 1 illustrates the demographic information of those women who used herbs for the induction of labor. The sample size of the study was 340 participants. Their mean (± SD) age is 29.9 ± 5.6 years. The majority of the participants were Saudi (84.4%), and over half of the participants held a bachelor’s degree (55.9%). Two-thirds of the participants were homemakers (67.6%), with monthly incomes between 5,000 and 10,000 Saudi Riyal (51.8%) (Table 1).
| Variable | Frequency | Percentage |
|---|---|---|
| Age | ||
| = 25 | 81 | 23.80% |
| 26-35 | 202 | 59.40% |
| = 36 | 57 | 16.80% |
| 340 | 100.00% | |
| Nationality | ||
| Saudi | 287 | 84.40% |
| Non-Saudi | 53 | 15.60% |
| 340 | 100.00% | |
| Education | ||
| Illiterate/High school or less | 126 | 37.10% |
| Bachelor’s degree | 190 | 55.90% |
| Postgraduate | 24 | 7.10% |
| 340 | 100.00% | |
| Occupation | ||
| Housewife | 230 | 67.60% |
| Teacher | 52 | 15.30% |
| Health care provider | 22 | 6.50% |
| Administrative | 36 | 10.60% |
| 340 | 100.00% | |
| Income (Saudi Riyal) | ||
| Less than 5,000 | 51 | 15.00% |
| 5,000 up to 10,000 | 176 | 51.80% |
| 10,000 up to 20,000 | 87 | 25.60% |
| More than 20,000 | 26 | 7.60% |
| 340 | 100.00% | |
| Gestational Age (Weeks) | ||
| 36 to 39 | 175 | 51.50% |
| 40 | 85 | 25.00% |
| 41 to 42 | 80 | 23.50% |
| 340 | 100.00% | |
| Parity | ||
| 1 | 84 | 31.70% |
| 2 | 66 | 24.90% |
| 3 | 50 | 18.90% |
| 4 | 26 | 9.80% |
| = 5 | 39 | 14.70% |
| 340 | 100% | |
Table 1: Distribution of participants by socio-demographic characteristics (n=340).
Just over half (51.5%) of the participants had a gestational period between 36 and 39 weeks, and for 31.7% of the participants, this was their first delivery. For most (92.9%) of the participants, the duration of labor was less than 24 h.
The Prevalence of Herbals Used to Induce Labour
The prevalence of herb use among pregnant women to induce labor after 36 weeks was 31.5% (107 participants). This number increased as the length of pregnancy continued, with (43.9%) using herbs to induce labor after a gestational period of 41 weeks (Table 2).
| Did you use herbs to induce labor in this pregnancy after 36 weeks? | Total | p-value | |||
|---|---|---|---|---|---|
| Yes | No | ||||
| 36 to 39 weeks | Count | 32 | 143 | 175 | 0.003 |
| % | 18.30% | 81.70% | 100.00% | ||
| 40 weeks | Count | 28 | 57 | 85 | |
| % | 32.90% | 67.10% | 100.00% | ||
| 41 to 42 weeks | Count | 47 | 33 | 80 | |
| % | 58.80% | 41.30% | 100.00% | ||
| Total | Count | 107 | 233 | 340 | |
| % | 31.50% | 68.50% | 100.00% | ||
Table 2 The prevalence of herb use among gestational age.
Association between Herb Use and Demographic Data
The results showed that herbal use for labor induction had a statistically significant association with the age of the women (p=0.003). Those participants who were aged between 26 and 35 years old had a higher propensity to use herbs to induce labor (65.4%).
There was also a high rate of the herb used to induce labor amongst women who were 41 weeks pregnant or more (43.9%). This statistical significance had a p-value of <0.001 (Table 3). The use of herbs was higher among Saudi women, those who held a bachelor’s degree, homemakers, and women who were para 2 or less. Unlike the length of pregnancy and age, however, these variables were not statistically significant.
| Variables | Herbal uses | Total | p-value | ||||
|---|---|---|---|---|---|---|---|
| Yes | No | ||||||
| Age | |||||||
| = 25 | 30 | 37.00% | 51 | 63.00% | 81 | 100.00% | 0.003 |
| 26-35 | 70 | 34.70% | 132 | 65.30% | 202 | 100.00% | |
| = 36 | 7 | 12.30% | 50 | 87.70% | 57 | 100.00% | |
| Total | 107 | 31.50% | 233 | 68.50% | 340 | 100.00% | |
| Nationality | |||||||
| Saudi | 90 | 31.40% | 197 | 68.60% | 287 | 100.00% | 0.918 |
| Non-Saudi | 17 | 32.10% | 36 | 67.90% | 53 | 100.00% | |
| Total | 107 | 31.50% | 233 | 68.50% | 340 | 100.00% | |
| Education | |||||||
| Illiterate/High school or less | 36 | 28.60% | 90 | 71.40% | 126 | 100.00% | 0.612 |
| Bachelor’s degree | 64 | 33.70% | 126 | 66.30% | 190 | 100.00% | |
| Postgraduate | 7 | 29.20% | 17 | 70.80% | 24 | 100.00% | |
| Total | 107 | 31.50% | 233 | 68.50% | 340 | 100.00% | |
| Occupation | |||||||
| Housewife | 78 | 33.90% | 152 | 66.10% | 230 | 100.00% | 0.492 |
| Teacher | 15 | 28.80% | 37 | 71.20% | 52 | 100.00% | |
| Health care provider | 6 | 27.30% | 16 | 72.70% | 22 | 100.00% | |
| Administrative | 8 | 22.20% | 28 | 77.80% | 36 | 100.00% | |
| Total | 107 | 31.50% | 233 | 68.50% | 340 | 100.00% | |
| Income (Saudi Riyal) | |||||||
| Less than 5,000 | 20 | 39.20% | 31 | 60.80% | 51 | 100.00% | 0.143 |
| 5,000 up to 10,000 | 46 | 26.10% | 130 | 73.90% | 176 | 100.00% | |
| 10,000 up to 20,000 | 33 | 37.90% | 54 | 62.10% | 87 | 100.00% | |
| More than 20,000 | 8 | 30.80% | 18 | 69.20% | 26 | 100.00% | |
| Total | 107 | 31.50% | 233 | 68.50% | 340 | 100.00% | |
| Gestational Age (Weeks) | |||||||
| 36 to 39 | 32 | 18.30% | 143 | 81.70% | 175 | 100.00% | = 0.001 |
| Up to 40 | 28 | 32.90% | 57 | 67.10% | 85 | 100.00% | |
| 41 to 42 | 47 | 58.80% | 33 | 41.30% | 80 | 100.00% | |
| Total | 107 | 31.50% | 233 | 68.50% | 340 | 100.00% | |
| Parity | |||||||
| 1 | 33 | 39.30% | 51 | 60.70% | 84 | 100.00% | 0.303 |
| 2 | 23 | 34.80% | 43 | 65.20% | 66 | 100.00% | |
| 3 | 13 | 26.00% | 37 | 74.00% | 50 | 100.00% | |
| 4 | 7 | 26.90% | 19 | 73.10% | 26 | 100.00% | |
| = 5 | 9 | 23.10% | 30 | 76.90% | 39 | 100.00% | |
| Total | 85 | 32.10% | 180 | 67.90% | 265 | 100.00% | |
Table 3 Association between herbal uses after 36 weeks of pregnancy with other variables.
Reasons to Use Herbs and Inducing Labour during Pregnancy after 36 Weeks
The most common reason for the use of herbs, which was cited by over half of the sample, was to make childbirth easier (57.5%) (Table 4). Advice from relatives or neighbors on the use of herbs to induce labor was the second most common reason (41.5%). Of the 370 respondents, only 26.4% used herbs to shorten the duration of labor. Almost 24.5% of the participants stated that they had previously used herbs for this purpose. Nearly a quarter of the participants (23.6%) used herbs due to their personal beliefs. Of those who were pregnant beyond 40 weeks, 21.7% had used herbs to induce labor.
| Did you use herbs to induce labor in this pregnancy after 36 weeks? | Total | ||
|---|---|---|---|
| Yes | |||
| previous experiences | Count | 26 | 26 |
| % | 24.50% | ||
| advice from relatives, family, or neighbor | Count | 44 | 44 |
| % | 41.50% | ||
| personal belief | Count | 25 | 25 |
| % | 23.60% | ||
| if you were postdated more than 40 weeks | Count | 23 | 23 |
| % | 21.70% | ||
| the membrane was ruptured | Count | 3 | 3 |
| % | 2.80% | ||
| to facilitate labor | Count | 61 | 61 |
| % | 57.50% | ||
| shorten the duration of labor | Count | 28 | 28 |
| % | 26.40% | ||
| safety and/or with no side effects | Count | 17 | 17 |
| % | 16.00% | ||
| its effectiveness | Count | 15 | 15 |
| % | 14.20% | ||
| easy to provide it | Count | 12 | 12 |
| % | 11.30% | ||
| tradition practices | Count | 18 | 18 |
| % | 17.00% | ||
| to avoid medical intervention | Count | 12 | 12 |
| % | 10.40% | ||
| Total | Count | 107 | 107 |
Table 4: Reasons for the use of herbs in the induction of labor during pregnancy after 36 weeks.
Moreover, the findings reveal that 17% of the participants stated that they use herbs as it is a traditional practice, and 16% considered it to be safe and without side effects. Among the respondents, 14.2% believed that it was an effective method by which to induce labor, and 11.3% believe herbs are easy to provide. A proportion of women (10.4%) had opted to use herbs to induce labor specifically to avoid medical intervention, and a further 2.8% had used herbs as their amniotic membrane was ruptured and they wanted to speed up the process of childbirth.
Sources for Herbs
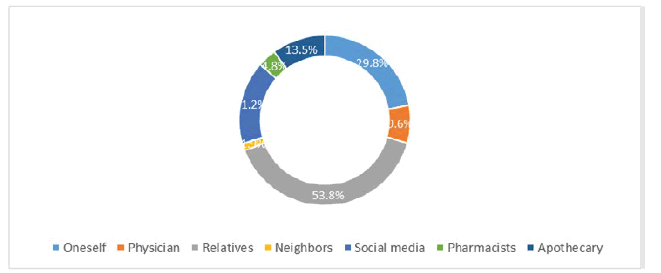
The data shows that the most common sources of herb supply were relatives for over half of the participants (53.8%). The second most common response was that the herbs were self-sourced (29.8%) (Figure 1). Some of the participants (21.2%) reported acquiring information regarding herbal medicines from social media, and 13.5% based their decision on advice from an apothecary. However, a smaller number (9.6%) of the participants asked their doctors and a smaller number still (3.8%) had approached a pharmacist to assist them in inducing labor.
Discussion
This study is attempted to understand the prevalence of pregnant women in Saudi Arabia who use herbs to induce labor. We found that 31.5% had used herbal approaches to accelerate labor. However, this percentage is low compared to findings reported by other studies. For instance, the use of herbal medicine by pregnant Malay women was significantly higher, at 73% [12]. Another study in Nigeria found that 67.5% of respondents had used some herbal medicine, be it in a crude form or as a pre-packaged, pharmaceutical dose [18]. As there is a pervading school of thought that herbs are safe and devoid of side effects, this might explain why there is such a high prevalence of herb use.
In a study by Glover, et al. 45.2% of women interviewed at rural outreach clinics and the Physician’s Office Centre of West Virginia University, Morgantown, had used at least one type of herbal medicine during pregnancy [19]. Pinn and Pallet provided questionnaires to women attending the antenatal clinic in an Australian district hospital, and 12% recorded that they had used herbal medicines [20]. One drawback of this study, however, is that the researchers had not specified how they defined the herbal medicine users.
It is common knowledge that traditional medicines and, in particular, herbal remedies are used more widely in developing countries. Conversely, however, several studies have found that the use of herbal medicine is also widespread in developed countries.
In this study, the use of herbal medicine to induce labor was higher in those aged between 26 and 35 years old (65.4%). The application of herbal remedies for inducing labor was associated with age (p=0.003). This is consistent with a similar result reported in a study of pregnant Malay women. Pregnant Malay women over the age of 30 used herbal remedies to a significantly greater extent (p=0.001) [12].
The use of herbal remedies to induce labor was higher among those who had been pregnant for longer. Women who were over 41 weeks pregnant showed higher levels of herb use (43.9%) (p<0.001). Another study has reported that during the third trimester of pregnancy, the majority of the respondents had used herbal medicines (79.6%) [21].
It was hypothesized that the level of education or income would inform the results, and a higher income and educational status would mean a diminished likelihood of traditional remedy use, although this was not the case. There were no significant associations in this study. However, the results from another study which occurred in an industrialized country showed a correlation between the use of herbal medicines and higher levels of income and education [22]. A further Malay study showed that the younger the female when pregnant, the more inclined they were to use herbal medicines (p=0.006). This study also indicates a statistically significant link between income and herb use [12].
Over half of the participants stated that they used herbal remedies to facilitate labor (57.5%). Another study explored a variety of reasons for the use of herbs in labor, but the most common is to ease the process of childbirth (89.2%) [12]. There was a belief amongst the majority of the respondents in this study that herbal remedies do effectively facilitate labor. This was supported by a study by Azriani, et al. in Tumpat, Kelantan, Malaysia. In this study, 108 of 210 mothers (51.4%) had used some herbal medicines during their pregnancy under the rationale that it facilitated labor (89.8%) [21].
This study showed that 30.2% of the respondents believed herbs to be an effective means by which to induce labor and that they are safe. This is lower than another study, which showed that 77.2% of women who took part perceived them to be safe and effective [12]. This is perhaps because herbs are ‘natural’ and do not contain seemingly dangerous chemicals. Also, these herbs have been used for generations. Consequently, they are considered safer for use during pregnancy than other more conventional medicines. However, there is a possibility of causing harm to the fetus due to potential interactions between alternative and conventional medicines.
The results of this study indicated that the most common source of supply of these alternative medicines was from relatives for over half of the participants (53.8%), and for 29.8% of respondents, the medicine was sourced by themselves. The most typical method by which to learn about herbal medicines was via social media (21.2%). Perhaps unsurprisingly, the women in the study were significantly influenced by social media. The information shared online is not whole evidence-based, and it is reliant on the sharing of previous experiences or traditional practices learned by elders, as is the case in many developing countries. These unsupervised and alarming practices are currently fashionable. Furthermore, these medicines are readily available and (to some extent) more economically affordable compared with modern medicine. These factors actively contribute to the widespread engagement in these practices.
The usage of herbal medicines is largely unsupervised, as demonstrated in another study, which showed that 81% of the respondents claim this to be the case. The same study also showed that the majority of women receive information on these remedies from their parents (60.7%) and purchase them directly from traditional midwives (32.2%) [12]. The most common advocates of these medicines were those of the older generation, such as parents (63.9%) [21]. Another qualitative study of Tswana mothers in South Africa has shown the considerable influence which is wielded by the older generation (such as grandmothers, mothers, and mothers-in-law) to take herbal medicines such as kgaba [14].
There are limitations for this study; the results cannot be extrapolated to create assumptions about other populations in the country. Besides, due to the nature of the study design, causal relationships could not be investigated.
Conclusion and Recommendations
This study shows that an alarming number of pregnant women are using the herbs to induce labor and, based on this finding, further investigation is recommended. The question of whether this practice is effective and safe needs to be investigated. Any future studies should focus on birth outcomes, as this will have a more significant impact on counseling and obstetric care. Another recommendation is for anyone who is taking herbs to discuss this decision with their physician.
Declarations
Acknowledgments
The author thanks the Deanship of Scientific Research and RSSU at King Saud University for their technical support.
This work was supported by the College of Medicine Research Center, Deanship of Scientific Research, King Saud University, Riyadh, Saudi Arabia.
Special thanks to Prof. Shaik Shafi Ahamed for his advice and for conducting the statistical analysis.
Funding
This research did not receive any specific grants from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Global Data. "National Center for Complementary and Alternative Medicine." In.: Thomson Reuters Embargoed Research Collection, 2014.
- Fischer, Felix H., et al. "High prevalence but limited evidence in complementary and alternative medicine: Guidelines for future research."BMC Complementary and Alternative Medicine,Vol. 14, No. 1, 2014, pp. 1-9.
- Kristoffersen, Agnete E., et al. "Gender differences in prevalence and associations for use of CAM in a large population study."BMC Complementary and Alternative Medicine,Vol. 14, No. 1, 2014, pp. 1-9.
- Alwhaibi, Monira, and Usha Sambamoorthi. "Sex differences in the use of complementary and alternative medicine among adults with multiple chronic conditions."Evidence-Based Complementary and Alternative Medicine,Vol. 2016, 2016.
- Al-Faris, Eiad A. "The pattern of alternative medicine use among patients attending health centres in a military community in Riyadh."Journal of Family and Community Medicine,Vol. 7, No. 2, 2000, pp. 17-25.
- Adnan, Muhammad, et al. "Ethnogynaecological assessment of medicinal plants in Pashtun’s Tribal Society."BioMed Research International,Vol. 2015, 2015.
- Fisher, Carole, et al. "The use of complementary and alternative medicine by 7427 Australian women with cyclic perimenstrual pain and discomfort: A cross-sectional study."BMC Complementary and Alternative Medicine,Vol. 16, No. 1, 2016, pp. 1-11.
- John, Lisha J., and Nisha Shantakumari. "Herbal medicines use during pregnancy: A review from the Middle East."Oman Medical Journal,Vol. 30, No. 4, 2015, pp. 229-36.
- Bergström, Cecilia, Margareta Persson, and Ingrid Mogren. "Sick leave and healthcare utilisation in women reporting pregnancy related low back pain and/or pelvic girdle pain at 14 months postpartum."Chiropractic and Manual Therapies,Vol. 24, No. 1, 2016, pp. 1-11.
- Hwang, Jung Hye, et al. "Use of complementary and alternative medicine in pregnancy: A cross-sectional survey on Iraqi women."BMC Complementary and Alternative Medicine,Vol. 16, No. 1, 2016, pp. 1-7.
- Jaradat, Nidal, and Deema Adawi. "Use of herbal medicines during pregnancy in a group of Palestinian women."Journal of Ethnopharmacology,Vol. 150, No. 1, 2013, pp. 79-84.
- Kim Sooi, Law, and Soon Lean Keng. "Herbal medicines: Malaysian women’s knowledge and practice."Evidence-Based Complementary and Alternative Medicine,Vol. 2013, 2013.
- Boulvain, Michel, et al. "Mechanical methods for induction of labour."Cochrane Database of Systematic Reviews,Vol. 4, 2001.
- Kelly, Anthony J., et al. "Vaginal prostaglandin (PGE2 and PGF2a) for induction of labour at term."Cochrane Database of Systematic Reviews,Vol. 4, 2009.
- Kelly, Anthony J., and Brenda P. Tan. "Intravenous oxytocin alone for cervical ripening and induction of labour."Cochrane Database of Systematic Reviews,Vol. 3, 2001.
- Tenore, Josie L. "Methods for cervical ripening and induction of labor."American Family Physician,Vol. 67, No. 10, 2003, pp. 2123-28.
- Smith, Caroline A., Caroline A. Crowther, and Suzanne J. Grant. "Acupuncture for induction of labour."Cochrane Database of Systematic Reviews,Vol. 8, 2013.
- Fakeye, Titilayo O., Rasaq Adisa, and Ismail E. Musa. "Attitude and use of herbal medicines among pregnant women in Nigeria."BMC Complementary and Alternative Medicine,Vol. 9, No. 1, 2009, pp. 1-7.
- Glover, Douglas D., et al. "Prescription, over-the-counter, and herbal medicine use in a rural, obstetric population."American Journal of Obstetrics and Gynecology,Vol. 188, No. 4, 2003, pp. 1039-45.
- Pinn, Graham, and Linda Pallett. "Herbal medicine in pregnancy."Complementary Therapies in Nursing and Midwifery,Vol. 8, No. 2, 2002, pp. 77-80.
- Rahman, Azriani Ab, et al. "Prevalence and pattern of use of herbal medicines during pregnancy in Tumpat district, Kelantan."The Malaysian Journal of Medical Sciences: MJMS,Vol. 15, No. 3, 2008, pp. 40-48.
- Barnes, Patricia M., Barbara Bloom, and Richard L. Nahin. "Complementary and alternative medicine use among adults and children; United States, 2007." National Health Statistics Reports, Vol. 12, 2008, pp. 1-24.