Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 9
The Sperm Vitality Test with Eosin-Nigrosin can be used as an Indicator of Globospermia Type III
Zafer Gashi1, Shkelzen Elezaj2, Afrim Zeqiraj1*, Fitore Gashi3, Naser Kamberi1 and Arvesa Shala42Regional Hospital, Peje, Republic of Kosovo
3Faculty of Medicine, University of Pristina, Republic of Kosovo
4Biolab-Zafi-F Medical Laboratory, Peje, Republic of Kosovo
Afrim Zeqiraj, UBT College Pristina, Republic of Kosovo, Email: afrim.zeqiraj@ubt-uni.net
Received: 23-Aug-2021 Accepted Date: Sep 23, 2021 ; Published: 30-Sep-2021, DOI: O
Abstract
Introduction: Teratozoospermia is characterized by the presence of spermatozoa with abnormal morphology in sperm. Globozoospermia is a rare (incidence 0.1%) and severe form of teratozoospermia characterized by the presence in the ejaculate of a large majority of round spermatozoa without acrosome. Globozoospermia is most commonly caused by mutations in the DPY19L2 gene. Globozoospermic spermatozoa are thus unable to adhere and penetrate the zona pellucida, causing primary infertility. Results: Total teratozoospermia 100% (globozoospermia 89% and other forms of abnormal morphology 11%), necrozoospermia 69%, asthenozoospermia 99%. Conclusion: The case presented is the first to be published as a pathology of infertility in the Republic of Kosovo. Teratozoospermia in the form of globozoospermia was 89%, and we called it globozoospermia severe or Globospermia type III, based on the results of 100% atypical morphology (89% globozoospermia +11% other atypical forms) and necrozoospermia 69% as well as asthenozoospermia 99%.
Keywords
Spermatozoa, Teratozoospermia, Globozoospermia, Necrosospermia, Asthenozoospermia
Introduction
Infertility is defined as the inability of couples to have a baby after one year of regular unprotected intercourse, affecting 10-15 percent of couples [1-3]. Large-scale studies have shown that about half of all cases of infertility occur due to female factors, 20 to 30 percent male factors, and 20 to 30 percent due to common causes of both gender [4-6]. Recent meta-analysis studies by researchers show that male factors are present in 20-70 percent of infertility cases [7]. Among the factors leading to male infertility, alterations of spermatogenesis are the major cause including quantitative defects (azoo-or oligozoospermia) or qualitative defects (teratozoospermia or asthenozoospermia) [8,9]. Teratozoospermia is characterized by the presence of spermatozoa with abnormal morphology in sperm. The literature is limited to three forms of teratozoospermia. The first group consists of “polymorphic teratozoospermia”, where a majority of spermatozoa display more than one type of abnormality. The second group, named “globozoospermia”, is characterized by round spermatic heads, absence of acrosome, and disorganization of mid-piece and tail. The third group consists of “enlarged head teratozoospermia”, where almost all spermatozoa have an enlarged head, multiple tails, and abnormal acrosome [10]. Globozoospermia is a rare (incidence 0.1%) and severe form of teratozoospermia characterized by the presence in the ejaculate of a large majority of round spermatozoa without acrosome [11]. Analysis of the incidence of cases with globozoospermia demonstrated history of consanguinity and a familial occurrence. Familial cases of globozoospermia suggest that this pathology has genetic origins, but the mode of inheritance remains unexplained, probably showing X-linked, sex-restricted dominant, or autosomal recessive modes of inheritance [12]. Globozoospermia is most commonly caused by mutations in the DPY19L2 gene [13]. Mutations in other genes likely also cause globozoospermia [13-15]. Globozoospermic sperm are thus unable to adhere and penetrate the zona pellucida, causing primary infertility. It is important to differentiate total globozoospermia referring to patients with a homogeneous phenotype with ~100% round-headed sperm and partial globozoospermia with a variable percentage of spermatozoa of typical shape. A minimum threshold of 20%-50% of round-headed spermatozoa is commonly used in the literature to confirm the diagnosis of globozoospermia [11,16,17].
Case Presentation
History of Illness
22/06/2017, a male patient born in 1984 was reported to the Bioloab-Zafi-F Medical Laboratory from the city of Peja, to perform a spermiogram analysis, referred by a specialist urologist with an indication of primary infertility after 6.5 years of infertility. A diagnosis was made from a urologist’s report based on previous analyzes conducted in various clinics and laboratories in Kosovo; Asthenospermia and normal morphology.
Results
The urologist did not find anything significant after the physical and genital examination of the patient. Testicular ultrasound parameters were normal (right testicular volume 32 ml, left testicular volume 25 ml).
Hormone biochemical analyses were normal values (Table 1).
| Results | Normal value | |
|---|---|---|
| FSH (mIU/mL) | 3.62 | 0.60-12.00 |
| LH (mIU/mL) | 3.22 | 0.60-12.00 |
| Testosterone (ng/mL) | 6.77 | 2.40-8.70 |
From the gynecologist’s medical reports owned by the patient’s wife, it was seen that his wife had done ultrasonography several times, and in the last 6 months, hysterosalpingography and hormone analysis (FSH.LH, EII, P4, PROL, TSH) were normal. The patient delivered ejaculate on the third day of abstinence, and the ejaculate analysis was performed 2x based on the criteria for analysis of ejaculate by the World Health Organization [18].
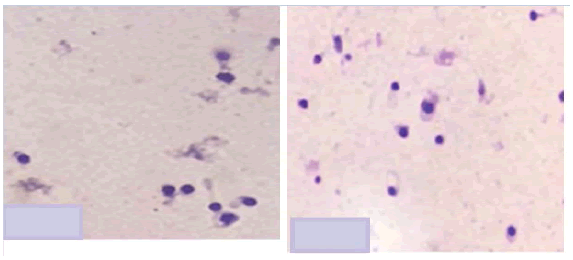
The main characteristics of sperm were as follows; volume=4.8 ml, pH 7.41, concentration=26.4 × 106 l, and total mobility=1% (grade c, mobility in place). However, sperm morphology revealed a diagnosis of 89% partial globozoospermia after staining by the May Grunewald-Giemsa method (MGG). An Eosin-Necrosis test, the viability in normal sperm samples, was also performed, and the result was 69% [18-20]. After detailed consultations with the couple, the man was found to be infertile for 6.5 years, and the ejaculate-spermiogram analysis was repeated two more times to confirm that it was a rare diagnosis of globosperm and first detected as pathology in an infertile man in the Republic of Kosovo (Figures 1-6).
The results are:
-total teratozoospermia 100% (globozoospermia 89% and other forms of abnormal morphology 11%)
-necrozoospermia 69%
-asthenozoospermia 99%
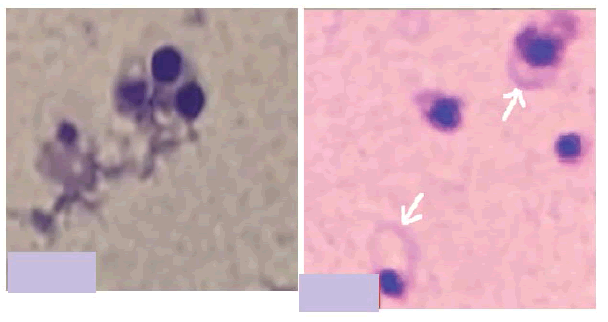
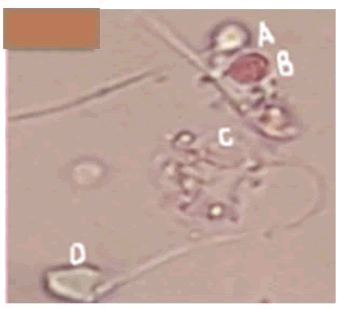
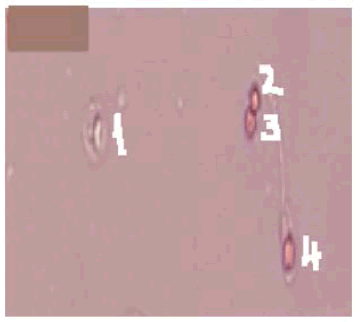
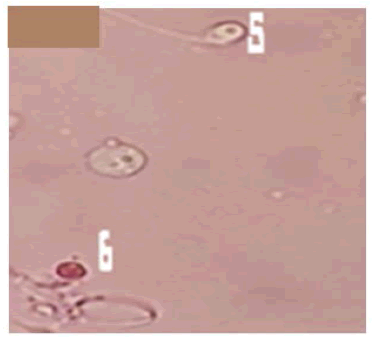
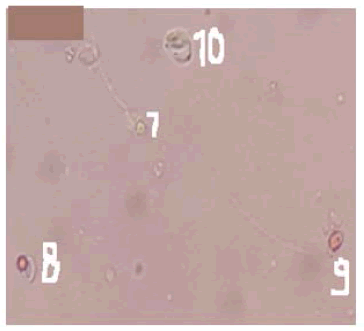
Figures 3-6 show the eosin-nigrosin staining technique for human sperm vitality assessment. Optical microscopic observations of sperm from a patient with partial globozoospermia
In our patient, the Eosin-Nigrosine vitality test was 31% live (unpainted heads of sperm) and 69% dead spermatozoa (red-head spermatozoa).
Normal range >58% vitality in normal sperm samples [18].
The presence of 89% globozoospermia is not teratozoospermia of the same percentage (globozoospermia 89% vs. necrozoospermia 69%). It is important to note that in the group of live sperm (31%) after the Eosin-Nigrosine test, 20% were globospermic and 11% live sperm with an atypical morphology of another non-globospermia (Figures 3-5).
Discussion
Globozoospermia is a rare incidence <0.1%, a genetic defect that causes male infertility [16]. It is characterized by multiple alterations such as spermatozoa with round heads, absence of acrosomes, and anomalies in chromatin condensation [11,21]. In this case presentation, we report our findings to spermatozoa with total teratozoospermia dominated by globozoospermic sperm as the first case detected in an infertile man in the Republic of Kosovo with total teratozoospermia and where globospermia dominates. In our case, the patient was with primary infertility and 89% are dominated by globozoospermic sperm which are characterized by the presence of round-headed sperm and total lack of acrosome (Figure 1 and Figure 2). The classification of globozoospermia based on morphological characteristics and the percentage of round-headed spermatozoa is not consensual. Singh classified globozoospermia into type I and type II [22]. Accordingly, in type I globozoospermia, also known as total or classic globozoospermia, or true roundhead only syndrome, 100% of the spermatozoa have a small, round, and acrosome-free head. Since round-headed spermatozoa are unable to penetrate the zona pellucida because of having no acrosome, this kind of disorder causes primary male infertility [22]. Contrary, men with type II globozoospermia have both normal and round-headed sperm cells with large which impair motility. In this type of globozoospermia, 20%-90% of spermatozoa have no acrosome; therefore, it is also known as partial globozoospermia [8,9,15,16].
We agree with the above-mentioned authors about this division of globozoospermia into two types but based on the case findings we present we have the dilemma that there are arguments that there must be type III globozoospermia, or severe globozoospermia as is the case of our patient. Our hypothesis that we can divide globosperm into three types is based on the percentage mentioned by the authors that type II globosperm counts from 20%-90% sperm with globosperm [8,9,16]. We thought it could not be concluded that it is globospermia type II result with 20% globospermic sperm. For example, the case presented by our group where globospermic sperm are 89% (Figure 1 and Figure 2) cannot be called globosperm type II. We did not find any positive encouraging results in achieving pregnancy in vivo when we had 20% or 50% of globospermic sperm. Therefore, we could not even think that there could be in vivo fertilization in cases with >50% or in our case 89% with atypical sperm, i.e. globozoospermia.
Dam concluded that partial globozoospermia is characterized by oval sperm cells with pronounced malformations on the sperm head matrix compared with normozoospermia, but normal sperm cells are also found [9]. We agree that type II partial globospermia has these characteristics; dominance of a higher percentage of globular spermatozoa and the presence of some spermatozoa of normal morphology. In our case, we have total teratozoospermia (100%), globospermic sperm 89%, and 11% non-glospermic spermatozoa, but with atypical morphology, as opposed to 69% necrosospermia. Necrosospermia was confirmed by the Eosin-Nigrosin test (Figures 3-6). The results show 31% of unstained head sperm i.e. live sperm. Within this percentage, 20% are globospermic live spermatozoa and 11% live morphologically atypical spermatozoa of other morphology than normal and not globospermic forms.
Based on our results we have hypothesized that we can talk about severe globozoospermia in the case of our patient and not with partial globozoospermia because we have more than 80% of sperm (89%) with globozoospermia associated with total teratozoospermia (100%) and the Eosin-Nigrosine vitality test has provided us with additional and reliable (easily verifiable) knowledge that we are dealing with another form of globozoospermia which we call “severe globozoospermia” when we have a high percentage of globozoospermia followed by 100% teratozoospermia. In cases with total globozoospermia as well as cases with severe globozoospermia as our case when we also have 99% asthenozoospermia, the sperm vitality test Eosin-Nigrosine gives us enough data that we can have live spermatozoa to use for the ICSI procedure after we have worked the HOS test.
The question is being raised, about in vitro conditions (IVF/ICSI). Now our hypothesis is “proud”. We agree with many authors that the only solution for cases with globozoospermia whether type I (total) or type II (partial) is the medically assisted fertilization procedure, the ICSI method.
For the ICSI method, the sperm with the best morphology is selected, the greatest mobility if there is movement and when it does not move (mobility 1%, movement in place) or 100% immobile and globospermic in percentage 89% as our case as we know that a globospermic sperm is also immobile, so which sperm will we use for ICSI. We have worked on the Eosin-Nigrosine test (Figures 3-6) to conclude that; our results have shown that globospermic and immobile sperm can be dead (heads are stained red) and alive (sperm heads are not stained). Such a finding could greatly contribute to IVF procedures to select live sperm to fertilize the oocyte with ICSI procedures. It is known that sperm cannot be used for fertilization with the ICSI method after the Eosin-Nigrosine test but it helps us a lot to trust the next Hypo-Osmotic Swelling (HOS) test-the test results from all the numerous articles have shown that the results of the HOS test and Eosin-Nigrosine are in fairly large consistency. It is known that sperm is immobile but with a positive HOS-test and can be used for oocyte fertilization with the ICSI method. We did not use Hypo-Osmotic Swelling (HOS) test or DNA fragmentation of sperm (for objective reasons), but we believe and expect that the author of other studies will confirm our hypothesis and come to a valid conclusion in cases with severe globozoospermia (80%-99%) type III must be checked Eosin-Nigrosine by a test in which percentage are globozoospermic sperm are necrozoospermic, to then do a HOS test on the day we need sperm for the ICSI procedure.
Conclusion
The case presented is the first to be published as a pathology of infertility in the Republic of Kosovo. Teratozosperm in the form of Globospermis was 89%, and we called it Globospermia severe or Globospermia type III, based on the results of 100% atypical morphology (89% globospermia+11% other atypical forms) and Necrosospermis 69% as well as asthenozoospermia 99%.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
References
- Turchi, Paolo. "Prevalence, definition, and classification of infertility." Clinical Management of Male Infertility. Springer, Cham, 2015, pp. 5-11.
- Vander Borght, Mélodie, and Christine Wyns. "Fertility and infertility: Definition and epidemiology." Clinical Biochemistry, Vol. 62, 2018, pp. 2-10.
- Zegers-Hochschild, Fernando, et al. "The international glossary on infertility and fertility care, 2017." Human Reproduction, Vol. 32, No. 9, 2017, pp. 1786-801.
- Kumar, Naina, and Amit Kant Singh. "Trends of male factor infertility, an important cause of infertility: A review of literature." Journal of Human Reproductive Sciences, Vol. 8, No. 4, 2015, pp. 191-96.
- Agarwal, Ashok, et al. "A unique view on male infertility around the globe." Reproductive Biology and Endocrinology, Vol. 13, No. 1, 2015, pp. 1-9.
- Masoumi, Seyedeh Zahra, et al. "An epidemiologic survey on the causes of infertility in patients referred to infertility center in Fatemieh Hospital in Hamadan." Iranian Journal of Reproductive Medicine, Vol. 13, No. 8, 2015, p. 513.
- Qi, Xiaokang, et al. "The role of testicular artery in laparoscopic varicocelectomy: A systematic review and meta-analysis." International Urology and Nephrology, Vol. 48, No. 6, 2016, pp. 955-65.
- Dam, Anika HDM, et al. "Homozygous mutation in SPATA16 is associated with male infertility in human globozoospermia." The American Journal of Human Genetics, Vol. 81, No. 4, 2007, pp. 813-20.
- Dam, Anika H., et al. "Morphology of partial globozoospermia." Journal of Andrology, Vol. 32, No. 2, 2011, pp. 199-206.
- Machev, N., P. Gosset, and S. Viville. "Chromosome abnormalities in sperm from infertile men with normal somatic karyotypes: Teratozoospermia." Cytogenetic and Genome Research, Vol. 111, No. 3-4, 2005, pp. 352-57.
- Modarres, Parastoo, et al. "An overview of the globozoospermia as a multigenic identified syndrome." International Journal of Fertility & Sterility, Vol. 12, No. 4, 2019, pp. 273-77.
- Stanislavov, R., and V. Ganev. "A clinico-genetic study of male infertility with globozoospermia." Obstetrics and Gynecology, Vol. 37, No. 4, 1998, pp. 20-22.
- Yassine, Sandra, et al. "Dpy19l2-deficient globozoospermic sperm display altered genome packaging and DNA damage that compromises the initiation of embryo development." Mhr: Basic Science of Reproductive Medicine, Vol. 21, No. 2, 2015, pp. 169-85.
- Coutton, Charles, et al. "MLPA and sequence analysis of DPY19L2 reveals point mutations causing globozoospermia." Human Reproduction, Vol. 27, No. 8, 2012, pp. 2549-58.
- Perrin, A., et al. "Molecular cytogenetic and genetic aspects of globozoospermia: A review." Andrologia, Vol. 45, No. 1, 2013, pp. 1-9.
- Dam, A. H. D. M., et al. "Globozoospermia revisited." Human Reproduction Update, Vol. 13, No. 1, 2007, pp. 63-75.
- Oud, M. S., et al. "Exome sequencing reveals novel causes as well as new candidate genes for human globozoospermia." Human Reproduction, Vol. 35, No. 1, 2020, pp. 240-52.
- World Health Organisation. "WHO laboratory manual for the examination of human semen and sperm-cervical mucus interaction." Cambridge University Press, 1999.
- Bjorndahl, L., I. Soderlund, and U. Kvist. "Evaluation of the one‐step eosin‐nigrosin staining technique for human sperm vitality assessment." Human Reproduction, Vol. 18, No. 4, 2003, pp. 813-16.
- Dougherty, Kathryn A., et al. "A comparison of subjective measurements of human sperm motility and viability with two live-dead staining techniques." Fertility and Sterility, Vol. 26, No. 7, 1975, pp. 700-03.
- Sen, CG Schirren, AF Holstein, and C. Schirren. "On the morphogenesis of round-headed human spermatozoa: On the cytomorphology of round-headed human spermatozoa/La morphogenèse des spermatozoides humains ayant tête ronde." Andrologia, Vol. 3, No. 3, 1971, pp. 117-25.
- Singh, G. "Ultrastructural features of round-headed human spermatozoa." International Journal of Fertility, Vol. 37, No. 2, 1992, pp. 99-102.