Research - International Journal of Medical Research & Health Sciences ( 2023) Volume 12, Issue 1
The Role of Diaphragmatic Shallow Breathing Index in Assessment of Diaphragmatic Dysfunction and Weaning from Mechanical Ventilation
Hatem Mowafy*, Kamel Abd el Aziz, Suzy Fawzy and Mohamed ShaabanHatem Mowafy, Department of Critical Care, Faculty of Medicine Cairo University, Egypt, Email: mowafy237@hotmail.com
Received: 13-Dec-2022, Manuscript No. ijmrhs-22-83365; Editor assigned: 15-Dec-2022, Pre QC No. ijmrhs-22-83365(PQ); Reviewed: 20-Dec-2022, QC No. ijmrhs-22-83365(Q); Revised: 26-Dec-2022, Manuscript No. ijmrhs-22-83365(R); Published: 30-Jan-2023
Abstract
Mechanical ventilation is one of the most common interventions in critical care. Weaning patients from mechanical ventilation is a cornerstone in the management of critically ill patients as unnecessary delay can lead to further complications 20% of the intubated patients show difficulty in extubation and weaning, despite established weaning criteria. The diaphragm is the principal respiratory muscle in humans, diaphragmatic ultrasound is a simple method useful to evaluate their thickness. This technique is highly feasible, simple, and non-invasive that can be used for the evaluation of diaphragmatic functions. This study aimed to compare the ability of the traditional RSBI and D-RSBI to predict successful weaning in ready-to-wean patients. A prospective observational study was conducted on 40 mechanically ventilated patients. In our study, DTF, DE, Rapid Shallow Breathing Index (RSBI), and Diaphragmatic Rapid Shallow Breathing Index (D-RSBI) were calculated for all those patients and correlated with the possibility of weaning. Weaned patients from mechanical ventilation were also followed up within the upcoming 48 hours for the risk of reintubation. The study population was subdivided into two groups; successful and failed weaning groups where 26 patients (65%) were weaned successfully from mechanical ventilation while 14 patients (35%) had failed the weaning trial. A statistically significant difference was found between each of DTF, Excursion, RBSI, and D-RBSI and weaning outcome (p=0.001, <0.001, 0.008, and <0.001) respectively in the study groups. DTF and Excursion were found higher in the successful weaning groups while RBSI and D-RBSI were found lower in the successful weaning groups. A Receiver Operating Characteristic (ROC) curve was calculated for DTF, DE, RSBI, and D-RSBI as indexes for successful weaning, and the cut-off point was ≥ 0.30, ≥ 19mm, ≤ 61 breaths/min/L, and ≤ 1.8 breaths/min/mm respectively. The D-RBSI was found as the most independent predictor of successful weaning by multivariate logistic regression with p-value=0.005.
Keywords
Mechanical ventilation, Diaphragmatic dysfunction, Weaning
Introduction
Mechanical ventilation is one of the most common interventions in critical care. Weaning patients from mechanical ventilation is a cornerstone in the management of critically ill patients as unnecessary delay can lead to further complications. 20% of the intubated patients show difficulty in extubation and weaning, despite established weaning criteria [1]. Timing is critical when deciding if a patient can be successfully extubated [2].
One of the major weaning failure determinants is the imbalance between the mechanical load imposed on the diaphragm and its ability to cope with it. accordingly, evaluating diaphragmatic function before any weaning attempt plays a fundamental role in ventilator dependency [3-6].
Mechanical ventilation, even after a short period, can also induce diaphragmatic dysfunction by reducing the force that generates the capacity of the diaphragm, with prevalence ranging from 33% to 95%, and accordingly remains the main cause of weaning difficulty or failure [7-9].
Diaphragmatic dysfunction (defined as DD <10 mm) is a predictor of weaning failure among patients in medical ICUs [10]. The Rapid Shallow Breathing Index (RSBI) (defined as the ratio of respiratory rate to tidal volume [RR/VT]) is one of the most widely used predictors of weaning outcome that has been reported as the most accurate weaning predictor [11]. But unfortunately, it has variable sensitivity and specificity [12-14]. Accordingly, substituting VT with DD in the RSBI, i.e., calculating diaphragmatic rapid shallow breathing index D-RSBI (DRSBI, RR/DD), can provide an accurate predictive index than the traditional RSBI [15].
• The relation between diaphragmatic ultrasound and weaning from mechanical ventilation.
• The assessment of the Diaphragmatic Rapid Shallow Breathing Index (D-RSBI), which is the ratio between Respiratory Rate (RR) and the ultrasonographic evaluation of Diaphragmatic Displacement (DD), is a new and promising tool to predict weaning outcomes.
• The relation between D-RSBI(diaphragmatic rapid shallow breathing), RSBI (Rapid Shallow Breathing Index), DTF (Diaphragmatic Thickening Fraction), and DD (Diaphragmatic Displacement ) as weaning tools from mechanical ventilation.
Methods
A prospective observational study on adult patients was conducted at the critical care department, of Cairo university hospital, the study was approved by the faculty of medicine, Cairo university medical ethics committee. Patients intubated and mechanically ventilated for more than 48 h planned for weaning were considered eligible for SBT if they met the following criteria:
• Clinical improvement of the underlying acute cause of respiratory failure.
• Adequate cough reflex.
• Absence of excessive and/or purulent tracheobronchial secretion.
• Stable cardiovascular status (i.e., heart rate <120 beats/min; mean arterial blood pressure, 60 mmHg-90 mmHg; and no vasopressor use).
• Stable metabolic status (i.e., electrolytes and glycemic index within normal range, body temperature <38°C, Hemoglobinemia ≥ 8 g/dL-10 g/dL).
• Adequate oxygenation (i.e., arterial oxygen saturation (SaO2) >92 % with inspiratory oxygen fraction (FiO2) ≤ 0.5 or arterial oxygen partial pressure to inspiratory oxygen fraction (PaO2/FiO2) ≥ 150 mmHg, both with Positive End-Expiratory Pressure (PEEP) ≤ 8 cmH2O).
• Adequate pulmonary function (i.e., RR ≤ 30 breaths/min with VT ≥ 5 mL/kg Ideal Body Weight (IBW) and no significant respiratory acidosis).
Exclusion Criteria
• Inability to obtain proper acoustic windows.
• Inability to obtain written informed consent.
• Patients under 18 years old.
• Hemodynamically unstable patient, on vasopressors.
• Presence of thoracotomy, pneumothorax, or pneumomediastinum.
• Neuromuscular disease or use of muscle-paralyzing agents within 48 h before the study.
• Advanced Peripheral neuropathy patients.
• Presence of flail chest or rib fractures.
• Advanced malignancy.
• Advanced heart failure.
Diaphragmatic Functions
Each diaphragm was evaluated by B-mode and M-mode Subcostal views used to rule out any abnormalities in muscle movement. All measurements were done by the ultrasound probe of Siemens Acuson X300 PE ultrasound machine (probe of 2 mH-4 mH frequency). We assessed the following parameters.
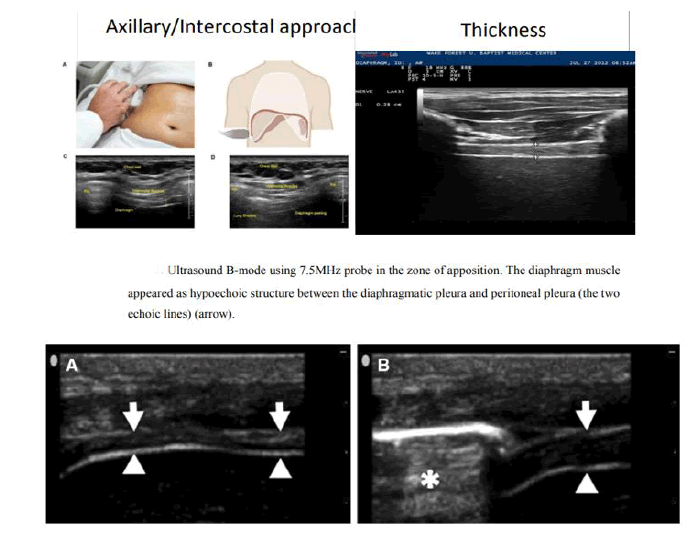
Diaphragmatic Thickens Fraction
The diaphragm was visualized by placing the probe perpendicular to the chest wall, in the eighth or ninth intercostal space, between the anterior axillary and the midaxillary lines, to observe the zone of apposition of the muscle 0.5cm to 2 cm below the costophrenic sinus. The diaphragm was imaged as a structure with three distinct layers, including two parallel echoic lines (the diaphragmatic pleura and the peritoneal membrane) and a hypoechoic structure between them (the muscle itself) [16]. The patient was then instructed to perform full inspiration to Total Lung Capacity (TLC) and then to exhale to Residual Volume (RV). Several images of the diaphragm were then captured and stored, including at least three at the point of maximum thickening at TLC and at least three at minimum thickening at RV. Images were obtained within the first 5 min of the SBT to identify the diaphragm and measure its thickness. It took three to five sessions; 10 min-15 min each.
On each frozen B-mode image; the diaphragm thickness was measured from the middle of the pleural line to the middle of the peritoneal line [16].
Then; DTF was calculated as a percentage from the following formula: Thickness at end inspiration-Thickness at end-expiration/Thickness at end-expiration (Figure 1) [17-23].
Diaphragmatic Excursion
• At the Anterior axillary line in the subcostal region, the Transducer is directed medially, cranially, and dorsally.
• B mode was used to assess excursion and M mode to measure the Normal range of motion from the resting expiratory position to full inspiration in adults 1.9 cm to 9 cm.
• Excursion >2.5 cm in adults as a cut-off was used for excluding severe diaphragm dysfunction [5].
Diaphragmatic Dysfunction
Diaphragmatic dysfunction was defined, during quiet breathing as Diaphragmatic excursion ≤ 11 mm or less and Diaphragm thickness less than 0.2 cm [5]. The Diaphragmatic Rapid Shallow Breathing Index (D-RSBI).
Statistical Analysis
Numerical variables were described as mean ± SD. Categorical variables were described as percentages. Comparisons were done using Student &‘‘t” and one-way ANOVA tests for numerical variables and the Chi-square test for categorical variables. Correlations were plotted and r values (correlation coefficients) were stated. ROC curves were plotted to determine cut-offs. P value was considered significant if ≤ 0.05.Statistics were calculated using SPSS 21 package [17].
Results
In our study, DTF (Diaphragmatic Thickening Fraction), DE (Diaphragmatic Excursion), RSBI (Rapid Shallow Breathing Index), and D-RSBI (Diaphragmatic Rapid Shallow Breathing Index) was calculated for all those patients and correlated with the possibility of weaning. Weaned patients from mechanical ventilation were also followed up within the upcoming 48 hours for the risk of reintubation.
The study population was subdivided into two groups; 26 patients (65%) were weaned successfully and 14 patients (35%) failed the weaning trial (Table 1 and 2).
|
Range | Mean ± SD | |
|---|---|---|---|
| Age | Failure | 56-91 | 71.2 ± 10.7 |
| Success | 22-75 | 4 ± 14.4 | |
| ICU stay (days) | Failure | 9-45 | 26.5 ± 10. |
| Success | 7-60 | 18.8 ± 12.9 | |
| Ventilation period | Failure | 3-14 | 6.85 ± 3.65 |
| Success | 1-16 | 5.46 ± 4.26 | |
| Ventilatory parameters | |||
| PaO2/FiO2 | Failure | 144-306 | 253.4 ± 50 |
| Success | 234-350 | 298.3 ± 26.7 | |
| RSBI(breaths/min/L) | Failure | 45-90 | 76.5 ± 15.8 |
| Success | 33-8- | 52 ± 12.9 | |
| C stat (ml/cmH2O) | Failure | 35-80 | 53.7 ± 11.4 |
| Success | 50-77 | 63.3 ± 6.8 | |
| Resistance( cmH2O/L/sec) | Failure | 3-15 | 6.9 ± 2.8 |
| Success | 14-19 | 11.3 ± 4.5 | |
| VT(ml) | Failure | 280-430 | 330.7 ± 36.2 |
| Success | 350-600 | 437.5 ± 57.6 | |
| P peak ( cmH2O) | Failure | 21-34 | 28.3 ± 3.5 |
| Success | 21-32 | 24.2 ± 2.9 | |
| P plateau (cmH2O) | Failure | 14-22 | 17.01 ± 2.8 |
| Success | 14-23 | 17.3 ± 1.78 | |
| Chest U/S parameters | |||
| DTF | Failure | 0.11-0.73 | 0.31 ± 0.21 |
| Success | 0.29-0.96 | 0.56 ± 0.22 | |
| Excursion(mm) | Failure | 7-16 | 12 ± 3 |
| Success | 16-32 | 21 ± 4 | |
| DRBSI ( breaths/min/mm) | Failure | 2.7 ± 0.9 | 1.4-4.2 |
| Success | 1.37 ± 0.46 | 0.8-2.6 | |
| Scores | |||
| SOFA | Failure | 6.7 ± 2.4 | 03-11 |
| Success | 3.6 ± 3.03 | 0-11 | |
| APACHE II | Failure | 17.2 ± 4.2 | 12-24 |
| Success | 9.8 ± 4.5 | 4-17 | |
| Expected Mortality | Failure | 24.2 ± 11. | 12-40 |
| Success | 9 9.8 ± 7.3 | 1-26 | |
| Demographic data | Weaning failure | Weaning success |
|---|---|---|
| Sex | ||
| Male | 10 (40%) | 15 (60%) |
| Female | 4 (26.6%) | 11 (74.4%) |
| Comorbidities | ||
| HTN | 3 (27%) | 8 (73%) |
| DM | 5 (45%) | 6 (55%) |
| Heart failure | 6 (33%) | 12 (67%) |
| Pneumonia | 13 (46%) | 15 (54%) |
| Renal impairment | 10 (62.5%) | 6 (37.5%) |
| Hypothyroidism | 4 (50%) | 4 (50%) |
| Neurological disorders | 6 (55%) | 5 (45%) |
| Fate | ||
| Survivor | 8 (57%) | 23 (88.5%) |
| Non-survivor | 6 (43%) | 3 (11.5%) |
Analytical Data
Shows the relation between age, gender, and weaning results where there was a strong statistical relationship between age and weaning failure with a p-value of 0.001 (Table 3).
| Weaning | p-value | ||
|---|---|---|---|
| Gender | Failure | Successful | 0.307 |
| Male | 4 (26.6%) | 11 (74.4%) | |
| female | 10 (40%) | 15 (60%) | |
| Age | Mean ± SD | 0.001 | |
| Failure | 71.2 ± 10.7 | ||
| Successful | 55.4 ± 14.4 | ||
Relation between different risk factors and comorbidities and weaning outcomes where pneumonia and renal impairment show a strong association with weaning failure with a p-value of 0.021 and 0.004 respectively (Table 4).
| Comorbidities | Weaning | p-value | |
|---|---|---|---|
| Failure | Successful | ||
| HTN | 3 (27%) | 8 (73%) | 0.404 |
| DM | 5 (45%) | 6 (55%) | 0.311 |
| Heart failure | 6 (33%) | 12 (67%) | 0.554 |
| Pneumonia | 13 (46%) | 15 (54%) | 0.021 |
| Renal impairment | 10 (62.5%) | 6 (37.5%) | 0.004 |
| Hypothyroidism | (50%) 4 | 4 (50%) | 0.276 |
| Neuro disorders | 6 (55%) | 5 (45%) | 0.111 |
The relation between risk factors and mortality where pneumonia shows a strong association with mortality with a pvalue of 0.016 (Table 5).
| Risk factors | Mortality | p-value | |
|---|---|---|---|
| survivor | Nonsurvivor | ||
| DM | 9 (81%) | 2 (19%) | 0.523 |
| Pneumonia | 5 (18%) | 21 (82%) | 0.016 |
| HTN | 9 (81%) | 2 (19%) | 0.523 |
| Heart failure | 15 (83.4%) | 3 (16.6%) | 0.341 |
| Neuro disorder | 8 (73%) | 3 (27%) | 0.477 |
| Hypothyroidism | 5 (62.5%) | 3 (37.5%) | 0.477 |
| Renal impairment | 10 (62.5%) | 6 (37.5%) | 0.042 |
The relation between ventilator parameters and weaning outcome where all mentioned parameters show a strong association with weaning outcome(Table 6).
| Mean ± SD | p-value | ||
|---|---|---|---|
| Ventilator measurements | |||
Weaning Failure |
Weaning Successful | ||
| PaO2/FiO2 | 253.4 ± 50 | 298.3 ± 26.7 | 0.006 |
| RSBI | 67.5 ± 15.8 | 52 ± 12.9 | 0.008 |
| Static compliance | 53.7 ± 11.4 | 63.3 ± 6.8 | 0.002 |
| Resistance | 11.3 ± 4.5 | 6.9 ± 2.8 | 0.004 |
The relation between LUS measurements and weaning outcome, where all measurements show a strong association with weaning outcome (Table 7).
| Mean ± SD | p-value | ||
|---|---|---|---|
| Weaning Failure | Weaning Successful | ||
| Thickness fraction | 0.31 ± 0.21 | 0.56 ± 0.22 | 0.001 |
| excursion | 1.24 ± 0.3 | 2.11 ± 0.4 | <0.001 |
| DRBSI | 2.7 ± 0.9 | 1.37 ± 0.46 | <0.001 |
This shows the relation between weaning outcomes sepsis, and mortality scores where both SOFA score and APACHE II score show a strong association with weaning outcome with p-value 0.021 and 0.032 respectively (Table 8).
| Scores | Mean ± SD | p-value | |
|---|---|---|---|
| Weaning Failure | Weaning Successful | ||
| SOFA | 6.7 ± 2.4 | 3.7 ± 3.0 | 0.021 |
| APACHE II | 17.2 ± 4.2 | 9.8 ± 4.5 | 0.032 |
Correlative Data
The Correlations of age, DTF, and DE with D-RSBI and RSBI where age and DE show strong statistical association with p-values 0.01 and <0.001 respectively, and r-values 0.353 and 0.729 respectively (Table 9).
| Variables | D-RSBI | RSBI | |
|---|---|---|---|
| Age | Pearson Correlation(r) | 0.353 | 0.463 |
| p-value | 0.025 | 0.002 | |
| DTF | Pearson Correlation(r) | 0.401 | 0.221 |
| p-value | 0.01 | 0.169 | |
| DE | Pearson Correlation(r) | 0.729 | 0.478 |
| p-value | <0.001 | 0.002 | |
Shows the Correlations of P/F ratio, RSBI and DTF with the length of ICU stay where statistical association showed p-value 0.004,0.016 and 0.013 respectively and r-value 0.437,0.377 and 0.389 respectively (Table 10).
| Variables | Length of ICU stay | |
|---|---|---|
| P\F ratio | Pearson Correlation (r) | 0.437 |
| p-value | 0.004 | |
| RSBI | Pearson Correlation (r) | 0.377 |
| p-value | 0.016 | |
| DTF | Pearson Correlation (r) | 0.389 |
| p-value | 0.013 | |
Comparative Data
Comparative statistical analysis between different outcomes including weaning results and mortality showed a significant statistical association with a p-value of 0.033 (Table 11).
| fate | Weaning | p-value | |
|---|---|---|---|
| Failure (14) | Successful (26) | ||
| survivors(31) | 8 (57%) | 23 (88.5%) | 0.033 |
| Non survivors(9) | 6 (43%) | 3 (11.5%) | |
Comparison between survivors and non-survivors as regards chest U/S where Thickness fraction, Excursion, and DRSBI showed a p-value of 0.004, 0.005, and 0.036 respectively (Table 12).
Receiver Operating Characteristic (ROC) Curve Analysis
| LUS measurements | Survivor | Non-survivor | p-value |
|---|---|---|---|
| Mean ± SD | |||
| Thickness fraction | 0.5 ± 0.3 | 0.3 ± 0.1 | 0.004 |
| Excursion | 1.9 ± 0.6 | 1.7 ± 0.5 | 0.005 |
| D-RSBI | 2.1 ± 2.2 | 1.0 ± 1.0 | 0.036 |
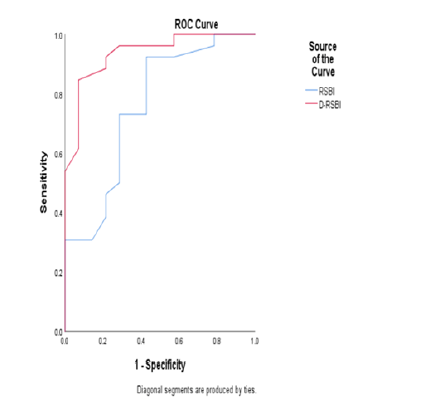
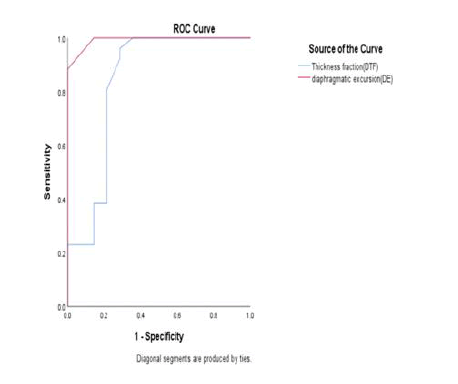
For prediction of successful weaning by the use of LUS parameters, RSBI, DSBI. At a cut of 30% of DTF, its sensitivity to predict successful weaning was 96% and its specificity was 71 % Area Under the ROC Curve (AUC=0.676). At a cut of 17 mm of diaphragmatic Excursion, its sensitivity to predict successful weaning was 88% and its specificity was 100% (AUC=0.973). At a cut of 61 breaths/min/L of RSBI, its sensitivity to predict successful weaning was 73% and its specificity was 71 % (AUC=0.755). At a cut of 1.8 breaths/min/mm of DRSBI, its sensitivity to predict successful weaning was 84% and its specificity was 92% (AUC=0.935) (Figure 2 and 3).
Discussion
The diaphragmatic Rapid Shallow Breathing Index (D-RSBI), the ratio between respiratory rate (RR) and the ultrasonographic Diaphragmatic Displacement (DD), is a new and promising tool to predict weaning outcomes [18]. Our results showed a statistically significant relationship between age and weaning results with a p-value (of 0.001). In contrast to our study, there was no statistically significant relationship between age and weaning results in with p-value (0.338, 0.508, and 0.976) respectively [19]. This can be explained by different age population groups, our study groups’ mean age was 55.4 and SD 14.4 for successful weaning groups, and the mean age was 71.2 and SD 10.7, the study groups’ mean age was 62 and SD 16 for successful weaning groups and mean age 66 and SD 11, relatively younger age groups.
There were no statistically significant differences between comorbidities and weaning outcomes in the two study groups except for pneumonia and renal impairment with p-values of 0.021 and 0.004 respectively. In the same context, did not show significant statistical relation between weaning outcome and comorbidities except for sepsis as a reason for initiating mechanical ventilation (p=0.035 and 0.008) respectively. This can be explained by different age groups, comorbidities, and types of patients as our study was conducted on medical and surgical ICU patients, the study was conducted on medical ICU patients only the study was conducted on COPD patients and severity of illness [15,20,21].
PaO2/FiO2 ratio was calculated before the start of SBT to indicate readiness for the weaning process, and then it was correlated with different variables. PaO2/FiO2 ratio was found to be significantly lower for patients who failed to wean than for those who were successfully weaned (p=0.006). The P/F ratio of the successful weaning groups ranged from 234 to 350 with a mean value and standard deviation (of 298.3 ± 26.7) while the failed weaning groups ranged from 144 to 306 with a mean value and standard deviation (of 253.4 ± 50). In concordance with our study, PaO2/FiO2 ratio was found to be significantly higher for patients who successfully weaned from MV (p ≤ 0.001) (p=0.002) respectively [22,23].
Regarding weaning from mechanical ventilation, our results showed that the cut-off point of DTF for successful weaning from mechanical ventilation was ≥ 30%. In the same context, the other cut-off points were in ≥ 30%, >36, ≥ 34.2%, >40% and >30% and all were associated with a successful SBT [24-27]. In our results, the DTF of the successful weaning groups ranged from 0.29 to 0.96 with a mean value of 0.56 while for the failed weaning groups it ranged from 0.11 to 0.73 with a mean value of 0.3. In the same context, in the DTF of the successful weaning groups ranged from 0.38 to 0.64 with a mean value of 0.56 while the failed weaning groups ranged from 0.22 to 0.30 with a mean value of 0.26. In our results, the DTF of the successful weaning groups was found to be significantly higher than the failed groups from MV (p=0.001). In concordance with our study, and the DTF of the successful weaning groups was found to be significantly higher than in the failed groups from MV (p ≤ 0.001)( p=0.001) (p<0.05) respectively [28]. Differences in DTF cut-off values can be explained by differences in methodology, the measurements were taken 12 hours to 36 hours before extubation, and done in controlled and spontaneous mode, variable inspiratory efforts, the patient population as in the study was carried on COPD patients, the severity of illness at ICU admission, metabolic conditions, and duration of MV were all patients on tracheostomy tube [25,28].
In our study, the cut-off point of DE that can predict successful weaning was ≥ 17 mm at end of inspiration. This was close to the cut-off point of which was >11 mm, >22 mm, >17.9 mm, ≥ 14 mm and 2018 >12 mm [15,18,29]. Our results showed that DE was significantly higher (21 mm (16 mm-32 mm) vs 12 mm (7 mm-16 mm) respectively in the successful extubation group compared to the failed one. In concordance with our study, stated that DE was significantly higher (16 mm (11.4 mm-18 mm) vs 9.8 mm (8.8 - mm-12 mm) respectively) in the successful extubation group compared to the failed one. In our results, the DE of the successful weaning groups was found to be significantly higher than the failed groups from MV (p ≤ 0.001). In the same context, in and Walaa and Lutfy, 2018, the DE of the successful weaning groups was found to be significantly higher than the failed groups from MV (p ≤ 0.001) (p ≤ 0.001) respectively. Different results of DE may be due to differences in posture, showing higher values when patients are supine versus seated, as well as when the abdominal and/or thoracic pressure is altered (eg. ascites, atelectasis) patient population ( Walaa and Lutfy, 2018 were carried on COPD patients, was carried on postoperative patients, in spontaneous ventilation through a T-tube was done with the FiO2 set at the same level used during mechanical ventilation, Also diaphragmatic ultrasound requires the use of high-frequency probes with precision to a few millimeters, meaning that slight variations in measurement between observers can substantially affect the result [30-33].
Our results showed that the cut-off point of RSBI for successful weaning from mechanical ventilation was ≤ 61 breaths/min/L showed 73% sensitivity and 71% specificity (AUC=0.755) was associated with a successful SBT. In the same context, the other cut-off points were ≥ 62 breaths/min/L showed 52% sensitivity and 97% specificity (AUC=0.720). , Walaa and Lutfy, 2018 (18) <70 breaths/min/L showed 69% sensitivity and 71% specificity (AUC=0.669), and <71 breaths/min/L showed 80% sensitivity and 70% specificity(AUC=0.815)., and Pirompanich and Romsaiyut, 2018 <105 breaths/min/L showed 78% sensitivity and 92% specificity and all were associated with a successful SBT. Our results showed that RSBI was significantly lower [52 breaths/min/L (33-80) vs 67 breaths/min/L (45-90) respectively] in the successful extubation group compared to the failed one [34]. In the same context stated that RSBI was significantly lower breaths/min/L (32-52) vs 63 breaths/min/L (37-90) respectively] in the successful extubation group compared to the failed one. In our results, the RSBI of the successful weaning groups was found to be significantly lower than the failed groups from MV (p=0.011). In concordance with our study in the RSBI of the successful weaning groups was found to be significantly lower than the failed groups from MV (p=0.012) while in concordance with our study, in Walaa and Lutfy, 2018, there was no statistically significant difference between failed and successful weaning groups (p=0.082) [18]. In concordance with our study, patients who failed the weaning attempt in this study had a lower RSBI (75.5 ± 11.4 breaths/min/L) than the cutoff value of 105 breaths/min/L to predict weaning failure originally described by Yang and Tobin [35]. Several other studies have documented a wide range of predictive values for RSBI, which could reflect Differences in methodology (the measurements were taken 12 hours-36 hours before extubation, Pirompanich and Romsaiyut, 2018 SBT was done for 1 hour and done on medical ICU patients), variable inspiratory efforts, patient population Walaa and Lutfy, 2018 was carried on COPD patients, the severity of illness at ICU admission [15,18,36].
Our results showed that the cut-off point of D-RSBI for successful weaning from mechanical ventilation was ≤ 1.8 breaths/min/mm showed 84% sensitivity and 92% specificity (AUC=0.935) was associated with a successful SBT. In the same context, the other cut-off points were < 1.3breaths/min/mm yielded 94.1 % sensitivity, 64.7% specificity (AUC=0.890), Walaa and Lutfy, 2018 <1.9 showed 82% sensitivity and 93% specificity (AUC=0.970) and (Mowafy and Abdelgalel, 2018) <1.6 breaths/min/mm showed 84% sensitivity and 100% specificity (AUC=0.979) and all were associated with a successful SBT [19]. Our results showed that D-RSBI was significantly lower (1.3 breaths/min/mm (0.8-2.6) vs 2.5 breaths/min/mm (1.4-4.2) respectively) in the successful extubation group compared to the failed one. In the same context stated that D-RSBI was significantly lower (1.2 breaths/min/mm (0.8-1.9) vs 2.7 breaths/min/mm (1.7-4.1) respectively) in the successful extubation group compared to the failed one. In our results, the D-RSBI of the successful weaning groups was found to be significantly lower than the failed groups from MV (p ≤ 0.001). In the same context, in Walaa and Lutfy, 2018, the D-RSBI of the successful weaning groups was found to be significantly lower than the failed groups from MV (p ≤ 0.001) (p ≤ 0.001) respectively. Different results of D-RSBI can be explained by differences in posture, showing lower values when patients are supine versus seated, as well as methodology, patient population( Walaa and Lutfy, 2018 were carried on COPD patients, spontaneous ventilation through a T-tube was done requiring more effort than SBT and (Mowafy and Abdelgalel, 2018) was done on surgical ICU patients). Also, diaphragmatic ultrasound variations in measurement between observers can affect the result. There is a strong positive correlation between D-RSBI and RSBI (r=0.678). Also, a statistically significant difference was found between DRSBI and RSBI (p ≤ 0.001), (p ≤ 0.001). A systematic review meta-analysis held a comparison between DTF and DE and found that DE is associated with inspiratory volume but does not correlate with other indexes of respiratory effort and data suggest a lower accuracy for DE compared to DTF in predicting weaning outcome [37]. Moreover, in patients undergoing MV, DTF reflects active diaphragm contraction, while DE comes from adding patients’ respiratory effort to the pressure generated by the ventilator, so its use is only meaningful in the absence of ventilatory support [37]. Despite being an observer-dependent technique, the available evidence suggests that both DTF and DE are reproducible measures and this can explain the difference in our results, especially in a diaphragmatic excursion to other studies. The D-RSBI was speculated to be more accurate than the RSBI because DD reflects more closely the diaphragmatic function as compared to VT. In the presence of diaphragmatic dysfunction, the diaphragm movement is depressed and the accessory muscles of inspiration assume a greater role in generating VT, but for a limited period as they are less efficient and easily fatigable [38,39]. In these situations, the VT is less linked to the function of the diaphragm than DD, which reflects the ability of the diaphragm to generate inspiratory volume [40]. However, while careful clinical observation remains the most important step in the decision to extubate, integrating it with the result of a relatively easy-to-obtain index like the D-RSBI could at least support the clinician in their decision [41-44].
Limitations
This study could be summarized in:
• A single physician performed the US.
• The nutritional status of the patients was not assessed which may affect muscle power.
• Being a single-center study
Conclusion
DD (defined as DD<10 mm), when combined with RR in an index that we named D-RSBI (RR/DD), is more accurate than the traditional RSBI (RR/VT) in predicting the weaning outcome, where, D-RSBI (RR/DD) cutoff of 1.8 is associated with the best sensitivity and specificity. We confirmed the importance of rapid and shallow breathing as a global index of weaning-induced patient distress
Declarations
Conflict of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Pinsky, Michael R., and Jean-Francois Dhainaut, eds. "Pathophysiologic foundations of critical care." Williams and Wilkins, 1993.
Google Scholar Crossref - Esteban, Andrés, et al. "Extubation outcome after spontaneous breathing trials with T-tube or pressure support ventilation." American journal of respiratory and critical care medicine, Vol. 156, No. 2, 1997, pp. 459-65.
Google Scholar Crossref - Vassilakopoulos, T., S. Zakynthinos, and C. H. Roussos. "Respiratory muscles and weaning failure." European Respiratory Journal, Vol. 9, No. 11, 1996, pp. 2383-2400.
Google Scholar Crossref - Heunks, Leo M., and Johannes G. Van Der Hoeven. "Clinical review: The ABC of weaning failure-a structured approach." Critical care, Vol. 14, No. 6, 2010, pp. 1-9.
Google Scholar Crossref - McCool, F. Dennis, and George E. Tzelepis. "Dysfunction of the diaphragm." New England Journal of Medicine, Vol, 366, No. 10, 2012, pp. 932-42.
Google Scholar Crossref - Jaber, Samir, et al. "Rapidly progressive diaphragmatic weakness and injury during mechanical ventilation in humans." American journal of respiratory and critical care medicine, Vol. 183, No. 3, 2011, pp. 364-71.
Google Scholar Crossref - Berek, K., et al. "Polyneuropathies in critically ill patients: a prospective evaluation." Intensive care medicine, Vol. 22, No. 9, 1996, pp. 849-55.
Google Scholar Crossref - Coakley, J. H., et al. "Preliminary observations on the neuromuscular abnormalities in patients with organ failure and sepsis." Intensive care medicine, Vol. 19, No. 6, 1993, pp. 323-28.
Google Scholar Crossref - Coakley, J. H., et al. "Preliminary observations on the neuromuscular abnormalities in patients with organ failure and sepsis." Intensive care medicine, Vol. 19, No. 6, 1993, pp. 323-28.
Google Scholar Crossref - Kim, W. Young, et al. "Diaphragm dysfunction assessed by ultrasonography: influence on weaning from mechanical ventilation." Critical care medicine, Vol. 39, No. 12, 2011, pp. 2627-30.
Google Scholar Crossref - Yang, Karl L., and Martin J. Tobin. "A prospective study of indexes predicting the outcome of trials of weaning from mechanical ventilation." New England Journal of Medicine, Vol. 324, No. 21, 1991, pp. 1445-50.
Google Scholar Crossref - Lee, Kang H., et al. "Rapid shallow breathing (frequency-tidal volume ratio) did not predict extubation outcome." Chest, Vol. 105, No. 2, 1994, pp. 540-43.
Google Scholar Crossref - Savi, Augusto, et al. "Weaning predictors do not predict extubation failure in simple-to-wean patients." Journal of critical care, Vol. 27, No. 2, 2012, pp. 221-e1.
Google Scholar Crossref - Huang, Chun-Ta, and Chong-Jen Yu. "Conventional weaning parameters do not predict extubation outcome in intubated subjects requiring prolonged mechanical ventilation." Respiratory care, Vol. 58, No. 8, 2013, pp. 1307-14.
Google Scholar Crossref - Spadaro, Savino, et al. "Can diaphragmatic ultrasonography performed during the T-tube trial predict weaning failure? The role of diaphragmatic rapid shallow breathing index." Critical Care, Vol. 20, No. 1, 2016, pp. 1-11.
Google Scholar Crossref - Wait, J. L., and R. L. Johnson. "Patterns of shortening and thickening of the human diaphragm." Journal of Applied Physiology, 1997.
Google Scholar Crossref - Statistics, I. S. "IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp." Google Search, 2013.
Google Scholar - Meghawri, Mohammed Walaa Saeed. "Role of diaphragmatic rapid shallow breathing index in predicting weaning outcome in patients with acute exacerbation of COPD". International Journal of COPD, 2018.
Google Scholar Crossref - Mowafy, Sherif MS, and Essam F. Abdelgalel. "Diaphragmatic rapid shallow breathing index for predicting weaning outcome from mechanical ventilation: Comparison with traditional rapid shallow breathing index." Egyptian Journal of Anaesthesia, 2018.
Google Scholar Crossref - DiNino, Ernest, et al. "Diaphragm ultrasound as a predictor of successful extubation from mechanical ventilation." Thorax, Vol. 69, No. 5, 2014, pp. 431-435.
Google Scholar Crossref - Ferrari, Giovanni, et al. "Diaphragm ultrasound as a new index of discontinuation from mechanical ventilation." Critical ultrasound journal, Vol. 6, No. 1, 2014, pp. 1-6.
Google Scholar Crossref - Moschietto, Sebastien, et al. "Transthoracic echocardiography with Doppler tissue imaging predicts weaning failure from mechanical ventilation: evolution of the left ventricle relaxation rate during a spontaneous breathing trial is the key factor in weaning outcome." Critical care, Vol. 16, No. 3, 2012, pp. 1-10.
Google Scholar Crossref - DiNino, Ernest, et al. "Diaphragm ultrasound as a predictor of successful extubation from mechanical ventilation." Thorax, Vol. 69, No. 5, 2014, pp. 431-35.
Google Scholar Crossref - Ferrari, Giovanni, et al. "Diaphragm ultrasound as a new index of discontinuation from mechanical ventilation." Critical ultrasound journal, Vol. 6, No. 1, 2014, pp. 1-6.
Google Scholar Crossref - Ferrari, Giovanni, et al. "Diaphragm ultrasound as a new index of discontinuation from mechanical ventilation." Critical ultrasound journal, Vol. 6, No. 1, 2014, pp. 1-6.
Google Scholar Crossref - Farghaly, Shereen, and Ali A. Hasan. "Diaphragm ultrasound as a new method to predict extubation outcome in mechanically ventilated patients." Australian Critical Care, Vol. 30, No. 1, 2017, pp. 37-43.
Google Scholar Crossref - Agmy, Gamal, Samiaa Hamdy, and Sherin Farghally. "Diaphragm ultrasound as a novel guide of weaning from invasive ventilation." 2015.
Google Scholar Crossref - Soliman, Soliman Belal, et al. "Chest ultrasound in predication of weaning failure." Open access Macedonian journal of medical sciences, Vol. 7, No. 7, 2019, p. 1143.
Google Scholar Crossref - Osman, Ahmed M., and Reham M. Hashim. "Diaphragmatic and lung ultrasound application as new predictive indices for the weaning process in ICU patients." The Egyptian Journal of Radiology and Nuclear Medicine, Vol. 48, No. 1, 2017, pp. 61-66.
Google Scholar Crossref - Ambrosino, Nicolino, and Luciano Gabbrielli. "The difficult-to-wean patient." Expert review of respiratory medicine, Vol. 4, No. 5, 2010, pp. 685-92.
Google Scholar Crossref - Matamis, Dimitrios, et al. "Sonographic evaluation of the diaphragm in critically ill patients. Technique and clinical applications." Intensive care medicine, Vol. 39, No. 5, 2013, pp. 801-10.
Google Scholar Crossref - Boussuges, Alain, Yoann Gole, and Philippe Blanc. "Diaphragmatic motion studied by m-mode ultrasonography: methods, reproducibility, and normal values." Chest, Vol. 135, No. 2, 2009, pp. 391-400.
Google Scholar Crossref - Wait, juliette L., et al. "Diaphragmatic thickness-lung volume relationship in vivo." Journal of Applied Physiology, Vol. 67, No. 4, 1989, pp. 1560-68.
Google Scholar Crossref - Pirompanich, Pattarin, and Sasithon Romsaiyut. "Use of diaphragm thickening fraction combined with rapid shallow breathing index for predicting success of weaning from mechanical ventilator in medical patients." Journal of intensive care, Vol. 6, No. 1, 2018, pp. 1-7.
Google Scholar Crossref - Yang, Karl L., and Martin J. Tobin. "A prospective study of indexes predicting the outcome of trials of weaning from mechanical ventilation." New England Journal of Medicine, Vol. 324, No. 21, 1991, pp. 1445-50.
Google Scholar Crossref - DiNino, Ernest, et al. "Diaphragm ultrasound as a predictor of successful extubation from mechanical ventilation." Thorax, Vol. 69, No. 5, 2014, pp. 431-35.
Google Scholar Crossref - Llamas-Alvarez, Ana M., Eva M. Tenza-Lozano, and Jaime Latour-Perez. "Diaphragm and lung ultrasound to predict weaning outcome: systematic review and meta-analysis." Chest, Vol. 152, No. 6, 2017, pp. 1140-50.
Google Scholar Crossref - Yan, S. H. E. N. G., et al. "Effect of diaphragmatic fatigue on control of respiratory muscles and ventilation during CO2 rebreathing." Journal of Applied Physiology, Vol. 75, No. 3, 1993, pp. 1364-70.
Google Scholar Crossref - Yan, S. H. E. N. G., et al. "Effect of global inspiratory muscle fatigue on ventilatory and respiratory muscle responses to CO2." Journal of Applied Physiology, Vol. 75, No. 3, 1993, pp. 1371-77.
Google Scholar Crossref - Umbrello, Michele, et al. "Diaphragm ultrasound as indicator of respiratory effort in critically ill patients undergoing assisted mechanical ventilation: a pilot clinical study." Critical Care, Vol. 19, No. 1, 2015, pp. 1-10.
Google Scholar Crossref - Esteban, Andrés, et al. "A comparison of four methods of weaning patients from mechanical ventilation." New England Journal of Medicine, Vol. 332, No. 6, 1995, pp. 345-50.
Google Scholar Crossref - Brochard, Laurent, et al. "Comparison of three methods of gradual withdrawal from ventilatory support during weaning from mechanical ventilation." American journal of respiratory and critical care medicine, Vol. 150, No. 4, 1994, pp. 896-03.
Google Scholar Crossref - Alvisi, R., et al. "Predictors of weaning outcome in chronic obstructive pulmonary disease patients." European Respiratory Journal, Vol. 15, No. 4, 2000, pp. 656-62.
Google Scholar Crossref - Farghaly, Shereen, and Ali A. Hasan. "Diaphragm ultrasound as a new method to predict extubation outcome in mechanically ventilated patients." Australian Critical Care, Vol. 30, No. 1, 2017, pp. 37-43.
Google Scholar Crossref