Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 3
The Role of Computed Tomography in the Diagnosis of Acute and Chronic Pulmonary Embolism (CTPA) in Multi Centers at Riyadh Region
Fahad M Alotaibi1,2, Ali Hassan A. Ali3,4*, Omar O. Serhan1, Abdullah Aldossary5, Ahmed Yqindin5, Khalid Z Aljulaifi6, Abdullah A Alghamdi6 and Youssef M Alsomali62Radiology Department, King Fahd Medical City, Ministry of Health, KSA
3Anatomy Department, College of Medicine, Prince Sattam bin Abdulaziz University, Alkharj, KSA
4Anatomy Department, Faculty of Medicine, Al-Azhar University, Cairo, Egypt
5Radiology Department, College of medicine Alfaisal University, KSA
6College of Medicine, Prince Sattam bin Abdulaziz University, Alkharj, KSA
Ali Hassan A. Ali, Anatomy Department, College of Medicine, Prince Sattam bin Abdulaziz University, Alkharj, KSA, Email: alihassan3750@yahoo.com
Received: 23-Feb-2021 Accepted Date: Mar 23, 2021 ; Published: 30-Mar-2021
Abstract
Pulmonary Embolism (PE), of acute type, is considered a significant reason for mortality due to cardiovascular cause. PE incidence is estimated to be about 60 to 70/100,000. However, the exact incidence could be higher due to silent PE. The PE incidence is rising in contrast to Deep Vein Thrombosis (DVT) that is declining. Diagnosis of PE may be a difficult task since clinical presentations (signs and symptoms) are variable especially in presence of comorbidities and laboratory tests are not that specific. Imaging techniques are of significant importance as suspected PE diagnostic evaluation. Computed Tomography Pulmonary Angiography (CTPA) is a frequently used imaging technique in cases of clinical high probability PE and positive D-dimer test. This study aimed at studying the correlation between blood investigations and Computed Tomography (CT) for diagnosis of Pulmonary Embolism (PE), also to determine the characteristics and accuracy of CT in detecting PE and to evaluate the incidence of PE according to males and females and to determine the most common comorbidities before the PE event. In this study, about half of the studied cases (47.1%) have chronic PE, one-third of the sample have acute PE (33.1%), while, (19.8%) of the sample study have massive PE. The Wells scoring was applied for the evaluation of risk probability because of its accuracy in the prediction of PE in suspected cases. There is a statically strong positive relation between blood investigation and CT of PE in the studied cases. It is recommended that patients with a high-risk probability of PE are recommended to perform CTPA directly without D-dimer testing.
Keywords
Computed tomography, Pulmonary embolism, High risk, Pulmonary angiography
Introduction
Pulmonary Embolism (PE), of acute type, is considered a significant reason for mortality due to cardiovascular cause [1]. PE incidence is estimated to be about 60 to 70/100,000 and the European report of the annual incidence of venous thrombosis and PE is 0.5 to 1.0 per 1000 population, however, the exact incidence could be higher due to silent PE [2].
Occlusion of pulmonary vasculature by an embolus is usually originating from a thrombus occluding a vein (usually of lower extremities). Coagulation factors, acting in a cascade, result in thrombosis that can be stimulated by endothelial injury, hypercoagulability, blood flow alterations. Small emboli usually occlude peripheral arteries while large ones could lodge into the main bifurcation causing “saddle embolism”; which causes marked compromise on the hemodynamic level, collapse, and marked dyspnea. If the thrombi pass through into very small and end arteries, pulmonary infarction usually occurs [3].
The clinical presentation of acute PE is not specific. Usually, suspicion of PE occurs mostly when the patient has chest pain, dyspnea, palpitations, syncope, or hemoptysis. Leg swelling, pain, and redness are associated symptoms of DVT [3,4]. Sometimes, PE shows no symptoms or exhibits incidental discovery when performing workup for diagnosis of another disorder [5].
The outcome of this study will provide the correlation between blood investigations and Computed Tomography (CT) for diagnosis of Pulmonary Embolism (PE), besides, determining the characteristics and accuracy of CT in detecting PE and show sensitivity and specificity of CT in the diagnosis of PE. Also, we are aiming to evaluate the incidence of PE according to males and females and to determine the most common comorbidities before the PE event. Certainly, we are hoping that the data of this study will help to improve the level of diagnosis of acute and chronic PE in hospitals and hence reduce patient death.
Material and Methods
This is a retrospective cross-sectional descriptive hospital-based study of patients admitted in King Fahad Medical City and King Khalid hospitals in diagnostic Centers-Riyadh. Data collection took place from 1 January 2019 to 31 December 2019 of 121 patients who had clinical features suggestive of PE according to symptoms, blood test, and clinical diagnosis with the subsequent radiologic investigation (Computed Tomography Pulmonary Angiogram CTPA). The study was approved by the ethics approval committee of the concerned hospital (H-01-R-012) (2019- 66M).
The evaluation was done, clinical assessment, and lab investigations such as D-dimer test, that the classical triad pleuritic chest pain, hemoptysis, and signs of DVT were not frequently detected (Table 1 and Table 2).
| Criterion | Points |
|---|---|
| Suspected DVT | 3.0 |
| An alternate diagnosis is less likely than PE | 3.0 |
| Heart rate > 100 beats/min | 1.5 |
| Immobilization or surgery in the previous four weeks | 1.5 |
| Previous DVT/PE | 1.5 |
| Hemoptysis | 1 |
| Malignancy (on treatment, treated in past six months) | 1 |
Table 1: Wells score criteria for Pulmonary Embolism (original and simplified).
| Score range | Mean probability of PE | %with score | Interpretation of risk |
|---|---|---|---|
| 0–2 points | 3.6% | 40% | Low |
| 3–6 points | 20.5% | 53% | Moderate |
| >6 points | 66.7% | 7% | High |
Table 2:Wells score interpretation.
Wells score according to Committee, ACEP Clinical Policies, 2003 was used for determining if direct CTPA was to be done or D-dimer analysis was to be requested first.
D-dimer test normal cutoff was 500 microgram/L. Age-adjusted D-dimer cut off in age more than 50 years=age × 10 microgram/L. It is used in low/intermediate probability patients. Cases with negative results are ruled out of PE, however, this cannot be applied in certain groups such as; hospitalized patients, post-surgical and pregnant females who need CT (false positive).
Cases with positive D-dimer were submitted for CT if high probability patient and if venous thromboembolism cannot be ruled out and for confirmation in very sick people.
Starting with CTPA for evaluation in high probability patients and if negative, Doppler US was done for venous thromboembolism detection before discharge from hospital.
Multiple-CT scanner 64 slices. Siemens RS Sensation 16 Mobile 420 ms rotation time (370 ms optional) 700 slices in 20s breath-hold Max. 100 seconds spiral duration Down to 105 ms temporal resolution with Heart View (option) 30 lp/cm spatial resolution Contrast delectable Philips Brilliance ICT 128 Slice and 256 Slice and other slices. Ethical clearance was taken before the start of the study. Patients having only pain in the abdomen were excluded from this study.
The position of patients was supine, lower lung to inferior cervical vertebras was the scanning area, 5 mm was the volume of scanning, administration of non-ionic opaque agent by auto-injectors (Missouri brand) through antecubital vein vascular access. Moreover, based on the patient, automatic scanning was delayed for 12 to 20 seconds, when pulmonary artery density becomes 120 Hounsfield units. The opaque agent was administrated between two bolus serum solutions, to prevent artifact. CT findings and the relationship between these findings and D-dimer results were analyzed. All data were recorded and analyzed in SPSS 20.
Results
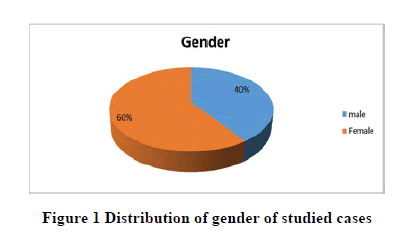
From Table 3 and Figure 1, we found that (59.5%) of the sample study are females and (40.5%) of the sample study are males.
| GENDER | Frequency | Percent |
|---|---|---|
| Male | 49 | 40.5 |
| Female | 72 | 59.5 |
| Total | 121 | 100.0 |
Table 3: Distribution of Gender of studied cases.
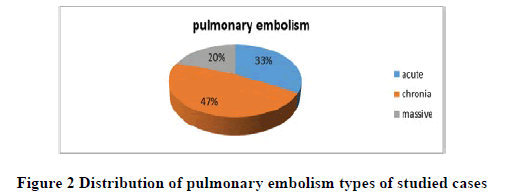
From Table 4 and Figure 2, we found that (47.1%) of the sample study have a chronic pulmonary embolism, (33.1%) of the sample study have an acute pulmonary embolism, and (19.8%) of the sample study have a massive pulmonary embolism.
| pulmonary embolism | Frequency | Percent |
|---|---|---|
| Acute | 40 | 33.1 |
| Chronic | 57 | 47.1 |
| Massive | 24 | 19.8 |
| Total | 121 | 100.0 |
Table 4: types of pulmonary embolism in studied cases.
To verify this incidence of acute and chronic pulmonary embolism according to males and females, we used independent samples t-Test and the results are shown in Table 5. We conclude that the significant value 0.902 which is more than 0.05 with t-value=0.123. This means that there is no statistical significance so we conclude that there is no difference between males and females in getting pulmonary embolism.
| GENDER | N | Mean | Std. Deviation | T | Sig |
|---|---|---|---|---|---|
| Male | 49 | 1.88 | .666 | .123 | .902 |
| Female | 72 | 1.86 | .756 |
Table 5: The incidence of acute and chronic pulmonary embolism according to males and females.
To verify this relation, we used (Person correlation test) and the results are shown in Table 6. We conclude that there is a statically strong positive relation between blood investigation and computed tomography of pulmonary embolism where significant value=0.004 less than 0.05 and correlation coefficient=0.863 positive value more than 0.5 which means that there is a statically strong positive relation between blood investigation and computed tomography of pulmonary embolism.
| pulmonary embolism | ||
|---|---|---|
| Blood investigation | Pearson Correlation | .863** |
| Sig. (2-tailed) | .004 | |
| N | 121 |
Table 6: The correlation between blood investigation and computed tomography of pulmonary embolism.
To determine the most common comorbidities before the PE event, we used one way Anova-Test and the results shown in Table 7.
| ANOVA | ||||||
|---|---|---|---|---|---|---|
| Sum of Squares | Df | Mean Square | F | Sig. | ||
| Cancer | Between Groups | .146 | 2 | .073 | .452 | .638 |
| Within Groups | 19.093 | 118 | .162 | |||
| Total | 19.240 | 120 | ||||
| Immobilization/surgery | Between Groups | .055 | 2 | .027 | .248 | .781 |
| Within Groups | 13.086 | 118 | .111 | |||
| Total | 13.140 | 120 | ||||
| Hypertension | Between Groups | 1.627 | 2 | .813 | 3.539 | .032 |
| Within Groups | 27.117 | 118 | .230 | |||
| Total | 28.744 | 120 | ||||
| Diabetes | Between Groups | 1.004 | 2 | .502 | 2.400 | .095 |
| Within Groups | 24.682 | 118 | .209 | |||
| Total | 25.686 | 120 | ||||
| Respiratory | Between Groups | .021 | 2 | .010 | .163 | .849 |
| Within Groups | 7.450 | 118 | .063 | |||
| Total | 7.471 | 120 | ||||
| Neuro | Between Groups | .183 | 2 | .091 | .786 | .458 |
| Within Groups | 13.702 | 118 | .116 | |||
| Total | 13.884 | 120 | ||||
| Kidney | Between Groups | .038 | 2 | .019 | .153 | .858 |
| Within Groups | 14.574 | 118 | .124 | |||
| Total | 14.612 | 120 | ||||
| Cardiac | Between Groups | .856 | 2 | .428 | 2.660 | .074 |
| Within Groups | 18.979 | 118 | .161 | |||
| Total | 19.835 | 120 | ||||
| D Dimer | Between Groups | .044 | .171 | .843 | ||
| Within Groups | 30.144 | 118 | .255 | |||
| Total | 30.231 | 120 | ||||
Table 7: Comorbidities prior to the PE event in studied cases.
We conclude that:
• There is no difference between affection with types of pulmonary embolism and the incidence of Cancer where significant value=0.638 more than 0.05
• There is no difference between affection with types of pulmonary embolism and the incidence of Immobilization/ surgery where significant value=0.781 more than 0.05
• There is no difference between affection with types of pulmonary embolism and the incidence of Diabetes where significant value=0.095 more than 0.05
• There is no difference between affection with types of pulmonary embolism and the incidence of Respiratory where significant value=0.849 more than 0.05
• There is no difference between affection with types of pulmonary embolism and the incidence of Neuro where significant value=0.458 more than 0.05
• There is no difference between affection with types of pulmonary embolism and the incidence of Kidney where significant value=0.858 more than 0.05
• There is no difference between affection with types of pulmonary embolism and the incidence of Cardiac where significant value=0.074 more than 0.05
• There is no difference between affection with types of pulmonary embolism and D Dimer where significant value=0.843 more than 0.05
• There is a difference between affection with types of pulmonary embolism and the incidence of Hypertension where significant value=0.032 less than 0.05 and to indicate this difference to any type we used the Kruskal- Wallis Test and the results shown as Table 8.
| PE | N | Mean Rank | Chi-Square | Df | Asymp. Sig. | |
|---|---|---|---|---|---|---|
| Hypertension | Acute | 40 | 58.79 | 6.791 | 2 | .034 |
| Chronic | 57 | 67.52 | ||||
| Massive | 24 | 49.21 | ||||
| Total | 121 |
Table 8: The incidence of hypertension in studied PE cases
From the above table, we conclude that there is a difference between types of pulmonary embolism and the incidence of hypertension and this difference was (chronic) with a mean (67.52).
Discussion
PE is considered a fatal disease of cardiovascular origin that can be commonly encountered. Diagnosis of such a condition requires clinical evidence. Most of the patients complain of one or more of these symptoms: chest pain, dyspnea, back pain, consciousness alteration, and syncope [6].
PE is not only an acute condition but it can be met within patients suffering from respiratory symptoms for a long time [7]. However, these are non-specific symptoms that could be seen in other conditions than PE [8].
Czech Society of Cardiology guidelines on PE utilize the typical classification into acute (massive, submassive, and small), subacute massive PE, and chronic thromboembolic pulmonary hypertension [9]. In this study about half of the studied cases (47.1%) have chronic PE, one-third of the sample have acute PE (33.1%), while, (19.8%) of the sample study have massive PE.
Another study performed on only 35 cases conducted by Davidsingh, et al. detected massive PE in 10 patients (28.5%), sub-massive PE in 21 patients (60%), and the rest of the cases (11.5%) had the mild disease of PE. This may be due to the difference in the number of cases included and the categorization according to the classification used.
In this study no statistical significance difference could be detected between males and females in getting PE, 59.5% of the sample studies were females and 40.5% of the sample study was males. The percentage of female and male patients in this work is comparable to a recent study performed by Mohamed, et al. on the accuracy of detection of pulmonary thromboembolism by CT where 54% were females and 46% were males [10].
Evaluation of suspected PE patients includes algorithms of clinical prediction criteria with/without D-dimer investigation. The Wells score integrated with D-dimer analysis (Wells/D-dimer), has given high prediction as a Negative Predictive Value (NPV) in previous studies. However, further evaluation using the radiological investigation is important particularly in patients with negative results and suspected clinical presentations and risk factors [8,11].
Pulmonary angiography has been considered as PE diagnosis standard method; however, its routine use cannot be applied since it is an invasive technique with reduced availability in health centers [12].
V/Q scanning can be utilized for PE risk determination before conducting CTPA and has been known as the most preferred noninvasive way for diagnosis besides chest X-ray. V/Q imaging is considered an indirect way of diagnosis by detection of secondary effects but pulmonary and mediastinal visualization cannot be achieved [8].
Recently, advances in device technology have reintroduced CTPA value in PE diagnosis with the availability of devices in variable health centers. Detailed cross-sections of vasculature can be obtained in the images of such devices. 3-dimension examination of anatomic structures could be supplied if required. Especially in CT scanning of thorax with venography, CTPA sensitivity has increased in PE from 83% to 93% [8,13].
In cases submitted for CTPA, some factors should be taken into consideration in patient selection such as radiation exposure, the renal toxicity risk of iodized injected opaque agents, prolonged stay in the emergency department, and elevated costs. Risk probability scoring e.g. Wells scale, with the use of clinical criteria rules has been proposed to not influence CTPA application rate for PE confirmed diagnosis or exclusion [8,14].
In this work, the Wells scoring was applied for the evaluation of risk probability because of its accuracy in the prediction of PE in suspected cases and the high prevalence of PE in such cases [15].
The D-dimer test is considered positive when greater than the cutoff point but this could be approved only in cases with low probability, however, positive cases are not confirmative of PE since the value can be elevated in many other disorders than PE [16,17].
In this work, we conclude that there is a statically strong positive relation between blood investigation and CT of PE where significant value=0.004 less than 0.05 and correlation coefficient=0.863 positive value more than 0.5 which means that there is a statistically strong positive relation between blood investigation and CT of PE.
This result goes hand in hand with the study of Gao, who performed an analysis on 32 cases of suspected PE performed CTPA, as they found that levels of D-dimer were significantly elevated in PE positive patients on CTPA than negative ones on CTPA [18].
Furthermore, another study on a larger number of cases performed CTPA (1,051), where 21% showed PE with corresponding analysis of D-dimer in 822 CTPAs. The 0.5 mg/L cut-offs achieved a sensitivity and negative predictive value of 99%. The age-adjusted cut-off achieved a sensitivity and NPV of 98%, and our suggested cut-off of 0.9 mg/L achieved a sensitivity and NPV of 97% [19].
All comorbidities before the PE event in sample cases were studied and there is no difference between affection with types of PE and the incidence of the conditions (cancer, surgery/immobilization, diabetes, kidney disease, cardiac disease, respiratory disease, and neural disease).
These results were different than the previous report of significant more frequent positive PE in cases of history of malignancy within 6 months [20].
Other studies reported that a history of immobilization or recent surgery has a relatively high frequency of positive PE and on the other hand also increased frequency for negative PE cases [20,21].
Furthermore, in this work, no significant difference could be detected with affection by PE and D-dimer which is supported by the findings of Dos Santos, et al. who detected no significant relationship between high D-dimer alone and the incidence of PE in high probability group [20]. Regarding recommendations, patient with high risk is recommended to perform CTPA directly without D-dimer testing [22,23].
There is a difference between affection with types of PE and the incidence of Hypertension where significant value=0.032 especially in relation with chronic cases this is supported by the incidence of CT criteria of thromboembolic pulmonary arterial hypertension in chronic cases of PE [24].
Conclusion and Recommendation
In this study, about half of the studied cases (47.1%) have chronic PE, one-third of the sample have acute PE (33.1%), while, (19.8%) of the sample study have massive PE. No statistically significant difference could be detected between male and female gender in PE affection. The Wells scoring was applied for the evaluation of risk probability because of its accuracy in the prediction of PE in suspected cases. There is a statically strong positive relation between blood investigation and CT of PE in the studied cases. All comorbidities before the PE event in sample cases were studied and there is no difference between affection with types of PE and the incidence of the conditions (cancer, surgery/ immobilization, diabetes, kidney disease, cardiac disease, respiratory disease, and neural disease). Furthermore, in this work, no significant difference could be detected with affection by PE and D-dimer. However, there is a difference between affection with types of PE and the incidence of Hypertension.
It is recommended that patients with a high-risk probability of PE are recommended to perform CTPA directly without D-dimer testing.
Declarations
Acknowledgment
This publication was supported by the Deanship of Scientific Research at Prince Sattam bin Abdulaziz University, Alkharj, Saudi Arabia.
Conflicts of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Wolberg, Alisa S., et al. "Venous thrombosis."Nature Reviews Disease Primers1.1 (2015): 1-17.
- Bĕlohlávek, Jan, Vladimír Dytrych, and Aleš Linhart. "Pulmonary embolism, part I: Epidemiology, risk factors and risk stratification, pathophysiology, clinical presentation, diagnosis and nonthrombotic pulmonary embolism."Experimental & Clinical Cardiology18.2 (2013): 129.
- Huisman, M., Barco, S., Cannegieter, S.et al.Pulmonary embolism.Nat Rev Dis Primers4,18028 (2018).
- Pollack, Charles V., et al. "Clinical characteristics, management, and outcomes of patients diagnosed with acute pulmonary embolism in the emergency department: initial report of EMPEROR (Multicenter Emergency Medicine Pulmonary Embolism in the Real World Registry)."Journal of the American College of Cardiology57.6 (2011): 700-706.
- Konstantinides, Stavros V., et al. "2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS) The Task Force for the diagnosis and management of acute pulmonary embolism of the European Society of Cardiology (ESC)."European heart journal41.4 (2020): 543-603.
- Stein, Paul D., et al. "Multidetector computed tomography for acute pulmonary embolism."New England Journal of Medicine354.22 (2006): 2317-2327.
- Bulbul, Yilmaz, et al. "Time delay between onset of symptoms and diagnosis in pulmonary thromboembolism."Respiration78.1 (2009): 36-41.
- Ozakin, Engin, et al. "An analysis of patients that underwent computed tomography pulmonary angiography with the prediagnosis of pulmonary embolism in the emergency department."The Scientific World Journal2014 (2014).
- Widimský, J., J. Malý, and P. Eliáš. "Doporučení pro diagnostiku a léčbu akutní plicní embolie."Vnitř. Lék54 (2008): 1S25-1S72.
- Yousef, Mohammed et al. “Evaluation of acute pulmonary embolism using spiral CT scan.” Indian Journal of Applied Research, Vol. 4, No. 4, 2011, pp. 397-400
- Kline, Jeffrey A., et al. "Prospective multicenter evaluation of the pulmonary embolism rule‐out criteria."Journal of Thrombosis and Haemostasis6.5 (2008): 772-780.
- Wells, Philip S., et al. "Use of a clinical model for safe management of patients with suspected pulmonary embolism."Annals of internal medicine129.12 (1998): 997-1005.
- Tresoldi, Silvia, et al. "MDCT of 220 consecutive patients with suspected acute pulmonary embolism: incidence of pulmonary embolism and of other acute or non-acute thoracic findings."La radiologia medica113.3 (2008): 373-384.
- Calder, Kirsten K., Mel Herbert, and Sean O. Henderson. "The mortality of untreated pulmonary embolism in emergency department patients."Annals of emergency medicine45.3 (2005): 302-310.
- Douma, Renée A., et al. "Performance of 4 clinical decision rules in the diagnostic management of acute pulmonary embolism: a prospective cohort study."Annals of internal medicine154.11 (2011): 709-718.
- Pieper, Carl F., et al. "Age, functional status, and racial differences in plasma D-dimer levels in community-dwelling elderly persons."The Journals of Gerontology Series A: Biological Sciences and Medical Sciences55.11 (2000): M649-M657.
- Fedullo, Peter F., and Victor F. Tapson. "The evaluation of suspected pulmonary embolism."New England Journal of Medicine349.13 (2003): 1247-1256.
- Gao, Hui, Hu Liu, and Yanjing Li. "Value of D‑dimer levels for the diagnosis of pulmonary embolism: An analysis of 32 cases with computed tomography pulmonary angiography."Experimental and therapeutic medicine16.2 (2018): 1554-1560.
- Kubak, Mateuzs Piotr, et al. "Elevated d-dimer cut-off values for computed tomography pulmonary angiography—d-dimer correlates with location of embolism."Annals of translational medicine4.11 (2016).
- Dos Santos, Bruno Sousa, et al. "Acute Pulmonary Thromboembolism Retrospective Auditory-The Benefits of Clinical Predictive Tools." (2019).
- Posadas-Martínez, María Lourdes, et al. "Performance of the Wells score in patients with suspected pulmonary embolism during hospitalization: a delayed-type cross sectional study in a community hospital."Thrombosis research133.2 (2014): 177-181.
- Authors/Task Force Members, et al. "2014 ESC Guidelines on the diagnosis and management of acute pulmonary embolism: The Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC) Endorsed by the European Respiratory Society (ERS)."European heart journal35.43 (2014): 3033-3080.
- Raja, Ali S., et al. "Evaluation of patients with suspected acute pulmonary embolism: best practice advice from the Clinical Guidelines Committee of the American College of Physicians."Annals of internal medicine163.9 (2015): 701-711.
- Doğan, Halil, et al. "The role of computed tomography in the diagnosis of acute and chronic pulmonary embolism."Diagnostic and Interventional Radiology21.4 (2015): 307.