Research - International Journal of Medical Research & Health Sciences ( 2020) Volume 9, Issue 12
The pyrosphere prosthesis compared with epping-arthroplasty for Surgical treatment of thumb root arthritis: a clinical cohort study
Anas Abdulqader Fathuldeen1,2, Salem Fayez Alshaghdali2*, Renad Meshal Ashban Alharbi2, Walaa Sulyman Salem Alrasheed2, Afnan Awdah Masoud Alhazimi2 and Ziyad Alharbi1,32College of Medicine, University of Ha’il, Ha’il, Saudi Arabia
3Plastic and Reconstructive Surgery Division, Fakeeh College of Medicine, Jeddah, Saudi Arabia
Salem Fayez Alshaghdali, College of Medicine, University of Ha’il, Ha’il, Saudi Arabia, Tel: 966 16 535 8200, Email: Salem.Alshaghdali@outlook.com
Received: 20-Nov-2020 Accepted Date: Dec 21, 2020 ; Published: 28-Dec-2020
Abstract
Objective: Rhizarthrosis indicates osteoarthritis induced degenerative changes of the thumb root. Several surgical interventions have been previously described. Our question is whether the PyroSphere joint replacement shows superior results when compared to other operative techniques such as Epping-Plasty for the treatment of thumb root arthritis. Therefore, the purpose of this study was to compare the efficacy of both interventions. Methods: In this clinical cohort study we reviewed our medical database to identify patients who suffered from rhizarthrosis Grade II-III according to Eaton Littler, who were treated operatively between 2002 and 2018. After a mean follow-up of 13 years, 14 cases were evaluated. Evaluation by clinical examination includes range of motion of the thumb, Kapandji score, force measurement of the thumb and hand using JAMAR dynamometer for grip and pinch strength. Pain assessment was done; DASH-Score and DSG questionnaire were also performed. Results: 14 hands were included, The PyroSphere joint prosthetics were observed in 7 hands and the Epping-Plasty group included the other 7 hands. In all comparative tests, P values were not statistically significant (all p>0.05). Conclusion: This study concludes that PyroSphere prosthetics show no superior results when compared to Epping-arthroplasty for the treatment of thumb root arthritis.
Keywords
Rhizarthrosis, Trapeziometacarpal osteoarthritis, Pyrosphere, Pyrocarbon, Epping arthroplasty, Trapezium
Abbreviations
CMC1: First Carpometacarpal Joint (1st CMC), ROM: Range Of Motion, NSAIDs: Non-Steroidal Anti-Inflammatory Drugs, DSG questionnaire: Daumensattelgelenk (Thumb saddle joint), DASH-score: Disabilities of Arm, Shoulder, and Hand-score, VAS: Visual Analogue Scale, MCP: Metacarpophalangeal, CMC: Carpometacarpal
Introduction
Rhizarthrosis indicates osteoarthritis induced degenerative changes of the thumb root. Specifically affecting the trapeziometacarpal and, in more severe stages, scaphotrapezial joint [1,2]. The trapeziometacarpal joint, also known as the first Carpometacarpal joint (CMC1), is a saddle-shaped joint with a characteristic concavoconvexity of both articulating surfaces [3-6]. The stability of the CMC1 joint is maintained by many stabilizing and supporting ligaments. These ligaments provide the ability to tolerate high-pressure loads, particularly during pinch and grasp maneuvers [7]. Although the number of ligaments surrounding the CMC1 Joint varies in anatomical literature, most authors state that five of these ligaments are most important for stability. Of these ligaments, the deep anterior oblique ligament, also known as the palmar beak ligament, is considered to be the most important stabilizing ligament [7-11]. Laxity of this ligament in particular, and in addition to the other surrounding ligaments, is involved in the progression of rhizarthrosis [12]. Conservative treatment options for rhizarthrosis include NSAIDs, corticosteroids, and intra-articular hyaluronic acid injections [13]. They’re usually used as a temporary measure before surgery, in elderly patients who aren’t good candidates for surgery, or in those patients who don’t prefer to undergo an operation [14]. Surgical arthrodesis was used before advances in arthroplasty took place and it’s still in practice today. Nevertheless, it has the disadvantages of functional compromise to reach joint stability and pain relief [15-17]. The least complex form of arthroplasty involves the trapezial excision alone. In 1949, Gervis published the results of total trapeziectomy performed on fifteen patients. It generally showed favorable results with improvement of pain and function except in two patients who had polyarthritis. Although no wires were used for the stabilization of the thumb after trapeziectomy, no obvious deformities were reported [15,16,18,19]. Moreover, partial excision of the trapezium was also performed and described in the literature [20,21]. In 1972, Alfred Swanson described a novel method for rhizarthrosis that involved trapezium resection and silicone implant arthroplasty [22]. This method has significant adverse outcomes including implant instability, implant tear, silicone synovitis, and implant failure [23-25]. One study revealed that on an average follow-up period of 6.5 years, 90% of patients with silicone implants manifested radiologic changes consistent with silicone synovitis [26]. Implants made of degradable polyurethaneurea with biocompatible properties (Artelon) were also introduced. Conversely, they were associated with a significant complication rate and poor preliminary results in the short-term [27-29]. In 1979, de la Caffiniere and Aucouturier introduced arthroplasty with a total prosthesis. This prosthesis uses a ball and socket design and involves the implantation of a cup made of polyethylene in the trapezium, for articulation with cobalt-chromium alloy placed in the first metacarpal shaft [30,31]. The pyrolytic carbon implant has the advantage of being inert and biocompatible. Hence, it has been widely implicated in clinical practice in the last decade [32]. The short-term results of pyrocarbon implants seem promising with positive outcomes in pain relief and range of motion, although the long-term remains unclear [33]. In addition to implants, another main surgical approach is complete trapeziectomy with or without ligament construction. Trapeziectomy without ligament reconstruction commonly involves stabilization by a K-wire. On the other side, tendons of abductor pollicis longus and/or flexor carpi radialis are used for thumb fixation in ligament reconstruction modalities [16]. In Epping arthroplasty, the trapezium is excised and followed by ligament reconstruction using the distal end flexor carpi readialis tendon [34,35]. The question of whether the PyroSphere shows superior results when compared to other operative techniques for the treatment of CMC1 arthritis has not been answered yet. Therefore, the purpose of the present study is to compare the efficacy of PyroSphere prosthesis with that of Epping arthroplasty in the treatment of trapeziometacarpal osteoarthritis.
Materials and Methods
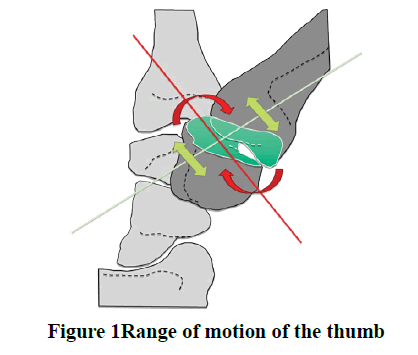
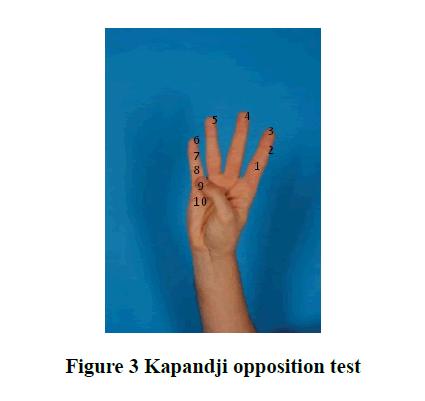
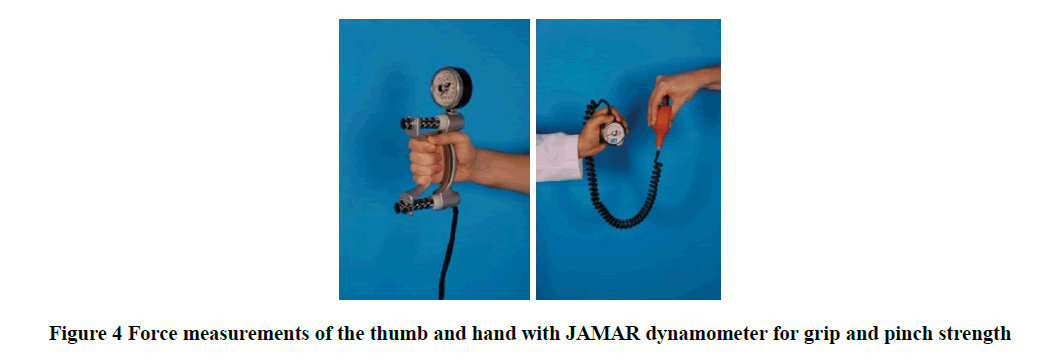
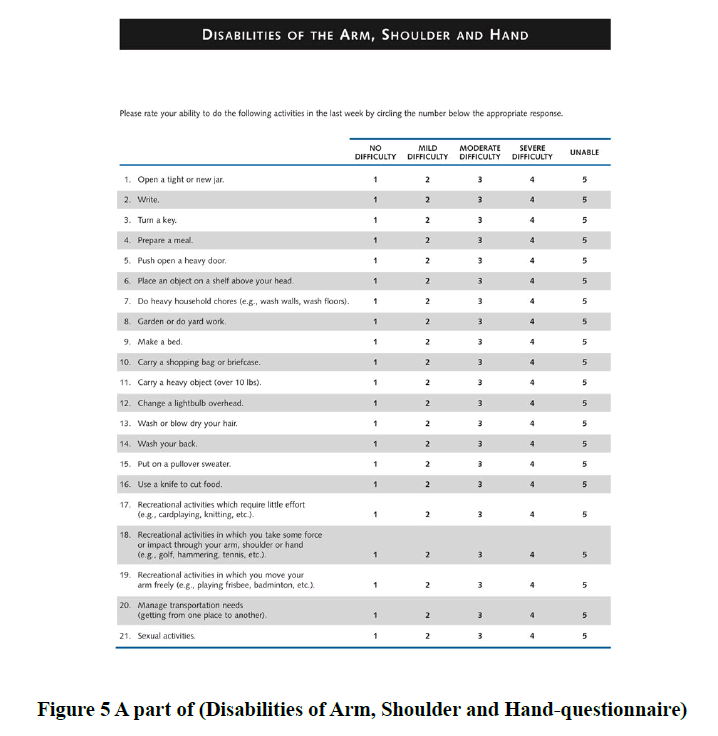
In this clinical cohort study we have reviewed the medical database at the Plastic Surgery Department of Aachen University, Germany to identify patients suffered from rhizarthrosis Grade II-III (according to Eaton Littler) who were treated operatively between 2002 and 2018, to evaluate and compare the postoperative outcome of two different surgical techniques, the PyroSphere prostheses and Epping-Plasty [36]. We excluded any patient less than 18 years, doubt inpatient therapy, pregnancy, contraindications for the implantation of pyrospecial prosthesis according to the manufacturer’s instructions and FDA approval, patient’s participation in interventional studies in the affected hand, contraindications against components of the therapy regimen, previous participation in a similar study, and rhizarthrosis grade IV. We identified and analyzed 21 patients (16 females and 5 males, mean age=66.7 years) who met our criteria. Of these, 6 females underwent a bilateral operation (3 underwent Pyrosphere, 2 underwent Epping-Plasty, 1 underwent both of these techniques). So, a total of 27 hands (11 right hands, 16 left hands), 14 hands treated with PyroSphere, and 13 hands treated with Epping-Plasty (Table 1). Follow-up examinations in the polyclinic after 1 week of wound control and after 3, 6, 12 months for functional evaluation. An e-mail invitation letter has been sent to each patient, and only 11 patients were presented for final clinical examination (8 females and 3 males, mean age=59.45 years). Of these, 3 females underwent a bilateral operation (2 underwent Pyrosphere, 1 underwent Epping-Plasty). So in total, we have 14 hands (7 right (1 male) and 7 left (2 male)). We have made an informed signed consent with each patient. We divided these patients-according to their surgical procedures- into two groups. Group A, we have 5 patients who underwent PyroSphere prostheses (4 females and 1 male, mean age=60.6 years) whereas two of them were treated bilaterally, a total of 7 hands, 3 right and 4 left (1 male). Group B, we have 6 patients who underwent Epping-Plasty (4 females and 2 males, mean age=59.6 years) whereas one of them was treated bilaterally, a total of 7 hands, 4 right (1 male) and 3 left (1 male) (Table 2). Preoperative symptoms were present for a mean of 2.5 years in Group A, while symptoms were present for 7.6 years in Group B. We have asked the patients to complete the DSG questionnaire, before performing the examinations. All patients were examined in terms of 3 months. It took 2 hours to perform the examinations and to fulfill DASH-Score per patient. The examinations were done by the same physician and included the following: Range of Motion of the thumb (Figure 1 and 2), Kapandji score (Figure 3), and force measurement of the thumb and hand using JAMAR dynamometer for grip and pinch strength (Figure 4) (Lafayette Instrument, Model J00105) [6, 37]. Pain assessment was done by Visual Analog Scale (VAS), either with load or without load. Also, all Patients were asked to complete the DASH-Score (Disabilities of Arm, Shoulder and Handquestionnaire) (Figure 5) [38].
| Total no. of patients | 21 |
| Total no. of hands | 27 |
| Sex (Female/Male) | 16/5 |
| Mean age in years | 66.7 |
| Side (Right/Left) | 11/16 |
| Procedure (PyroSphere/Epping) | 14/13 |
Table 1: General characteristic of the patients
| Group A | Group B | |
|---|---|---|
| Total no. of patients | 5 | 6 |
| Total no. of hands | 7 | 7 |
| Sex (Female/Male) | 4/1 | 4/2 |
| Mean age in years | 60.6 | 59.6 |
| Side (Right/Left) | 3/4 | 4/3 |
Table 2: General characteristics of the patients who presented for the final clinical examination (divided according to their surgical procedures) A: PyroSphere prostheses; B: Epping-Plasty
Statistical Analysis:
Significance was set at p<0.05. Microsoft Excel, GraphPad Prism were used t-test.
Results
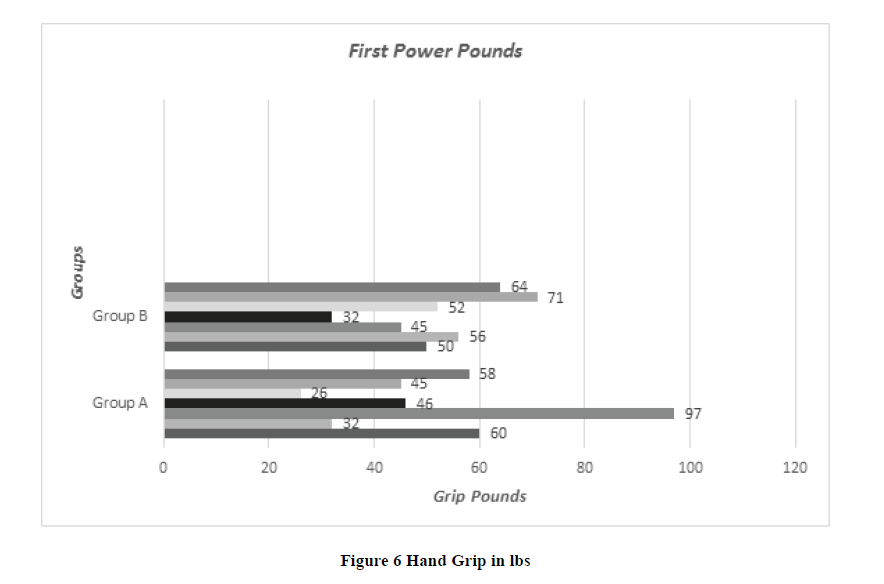
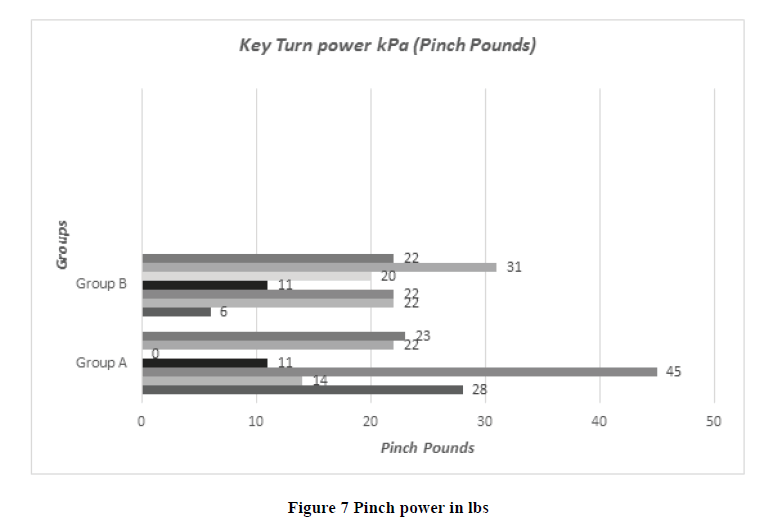
In our study twenty-one, patients were included, identified, and analyzed (17 females, 4 males, mean age=66.7 years) who were treated operatively with rhizarthrosis in the period between 2002 and 2018. Only 11 patients (14 Hands) were presented for final clinical examination. All patients suffered from rhizarthrosis Grade II-III according to Eaton Littler. 7 hands were treated with PyroSphere prostheses and 7 Hands with Epping-Plasty. The PyroSphere Group (Group A) included 7 hands (6 females, 1 male, mean age=68.4 years) and the Epping Plasty Group (Group B) contained 7 hands (5 females, 2 males, mean age=65.4 years). The majority of the patient followed up in a period of five days, 3 months, and 6 months. Most of the patients in both groups were working as a housewife (5 of 7 in group A and 5 of 7 in group B) in Group A, the right hand was affected 3 times, the left hand 4 times and in Group B the right hand was affected 4 times, the left hand 3 times. All patients from both groups are operated on as primary osteoarthritis. Regarding Pain scale (VAS) without load for the PyroSphere Group (Group A), one patient has a score of 1 out of 10, and the rest of the group have a score of 0 out of 10 (0=no pain, 10=Max pain) and for the Epping Plasty Group (Group B) one patient has score 3 out of 10 and rest of group have score 0 out of 10 (p-value=0.539). For the Pain scale (VAS) with load, one patient from Group A who treated by PyoSphere prostheses in both Right and Left hands have a pain scale of 7 out of 10 in his right hand and 10 out of 10 in his left hand and Group B three patient have score 9, 5, 1 out of 10 (p-value =0.893). Fist power pounds (Grip Pounds) were assessed equally for each group, the minimum value detected was 26 lbs and the maximum value was 97 lbs in Group A and the minimum value detected is 32 lbs and the maximum value is 71 lbs in Group B (p-value=0.993) (Figure 6). Key turn power kPa (Pinch Pound) were also assessed in both groups and the minimum value in Group A was 0 and the maximum was 45 and in Group B minimum value was 6 and the maximum value was 31 (p-value=0.893) (Figure 7). Patients were tested using Kapandji opposition test score also, all patients were asked to complete a DASH-Score and the result is summarized in Table 3. In all comparative tests, (DASH-Score p=0.842), (Grip Strength p=0.993) and (Kapandji Opposition test p=0.270) p-value were not statistically significant (all p>0.05).
| Gender (M/F) | Age (years) | Side (R/L) | Indication | Operation (Pyro vs. Epping) | Pain Scale (VAS) without Load 0=No pain 10=Max. Pain p=0.539 | Pain Scale (VAS) with Load 0=No pain 10=Max. Pain p=0.893 | Fist power pounds (Grip) Pounds p=0.993 | Key turn power kPa (Pinch) Pounds p=0.893 | Kapandji Opposition Test Score p=0.270 | DASH Questioner Score p=0.842 |
|---|---|---|---|---|---|---|---|---|---|---|
| Group A (Pyro-Carbon-prosthesis | ||||||||||
| F | 69 | L | Primary | Pyro | 0 | 0 | 60 | 28 | 10 | 3.3 |
| F | 71 | R | Primary | Pyro | 0 | 0 | 32 | 14 | 8 | 6.9 |
| M | 53 | L | Primary | Pyro | 0 | 0 | 97 | 45 | 10 | 0 |
| F | 49 | R | Primary | Pyro | 0 | 7 | 46 | 11 | 8 | 46.6 |
| F | 49 | L | Primary | Pyro | 1 | 10 | 26 | 0 | 4 | 89.7 |
| F | 71 | L | Primary | Pyro | 0 | 0 | 45 | 22 | 10 | 1.7 |
| F | 61 | R | Primary | Pyro | 0 | 0 | 58 | 23 | 9 | 0.8 |
| Group B (Epping-Arthoplasty) | ||||||||||
| M | 55 | R | Primary | Epping | 0 | 9 | 50 | 6 | 8 | 67.5 |
| F | 58 | L | Primary | Epping | 0 | 0 | 56 | 22 | 10 | 13.3 |
| F | 53 | R | Primary | Epping | 0 | 1 | 45 | 22 | 10 | 20.8 |
| M | 67 | L | Trauma | Epping | 0 | 0 | 32 | 11 | 9 | 28.3 |
| F | 53 | L | Primary | Epping | 3 | 5 | 52 | 20 | 10 | 40 |
| F | 64 | R | Primary | Epping | 0 | 0 | 71 | 31 | 10 | 0.8 |
| F | 54 | R | Primary | Epping | 0 | 0 | 64 | 22 | 9 | 0.8 |
Table 3: Shows comparison between Group A and B in scoring system
Discussion
Several studies were done to review and compare the outcomes of different surgical techniques that are available for the treatment of Rhizarthrosis [39,40]. Among these techniques, the pyrolytic carbon MCP joint arthroplasty, appears to be of a promising outcome. Pyrolytic carbon implants are available in many designs including the Pyrodisk and PyroSphere. They have the advantage of preserving the collateral ligaments, with a minimal bone resection [33]. The short-term results of pyrocarbon implants have been evaluated by Parker WL and have shown positive outcomes in pain relief and range of motion [33]. High patient satisfaction and excellent pain relief were also reported with the Pyrodisk arthroplasty [41]. However, the pyrosephere implants were reported to have a higher rate of complications [42].
Regarding the pain intensity assessed using the Visual Analogue Scale (VAS) without load and with load, our result found no significant difference between the two groups of patients treated with PyroSphere prosthesis with that of epping arthroplasty. This’s is in keeping with that of Claudia Santos, who compared the result of trapeziectomy with or without ligamentoplasty versus total prosthesis and found no significant difference concerning pain, mobility, strength, or activities of daily living [40].
In the view of Evaluation of Pinch grip which is fundamental to many of daily living activities, our result shows no significant difference between the two groups of patients, (p-value =0.893) [43]. This result is also in keeping with that of Claudia Santos [40]. Regarding the maintenance of grip strength, several studies suggest that total arthroplasty of the CMC joint is superior to other surgical procedures [44,45]. However other studies showed insignificant differences [40].
In a previous study, the overall outcome of the modified Epping procedure was found to be encouraging, despite a mean DASH score of 32.39. However, a relatively subjective loss of strength is the main complaint among these patients, whereas instability is less of concern [46].
The DASH score in a thumb-targeted module assessing basal joint-loading in the thumb was 63 points before and 21 points after surgery. In the patients with total joint replacement; total DASH score, 56 and 7 points; thumb module DASH score, 60 and 11 points [47]. Many contradictory results are observed in the literature in comparing the above two techniques. We think it is attributed to the different follow-up periods of patients among these studies.
Conclusion and Limitations
This study concludes that PyroSphere prosthesis shows no superior results when compared to Epping-arthroplasty for the treatment of thumb root arthritis. However, this study is limited by the small number of patients included. A larger sample comparative study is needed.
Declerations
Ethics approval and consent to participate:
Ethical approval has been taken and all surgical procedures took place in the Department of Plastic Surgery, Hand Surgery, and Burn Centre at RWTH University Hospital, Aachen, Germany. Each patient signed the consent form. All examinations were carried out in compliance with the Declaration of Helsinki in its current form.
Consent for publication:
Consent to publish was obtained from study participants. They provided written informed consent for their personal or clinical details.
Availability of data and materials:
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Authors’ contributions
AF drafted the manuscript and helped in operations of the patients as well as follows up of previously operated patients and participated in the analysis and interpretation of data. RA and HA conceived the design of the study. AA and SA helped in drafting the manuscript. ZA participated in the operations and follow up previously operated patients as well as revised and edited the manuscript. All authors read and approved the final manuscript.
Acknowledgments:
The authors gratefully acknowledge the efforts of Mr. Werner Kriegel for his remarkable contributions to this study.
Funding:
This study was supported by Aachen University Hospital. The funding body has no role in the design of the study, interpretation of data, and writing of the manuscript.
Conflict of Interests:
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Meireles, Sandra Mara, Anamaria Jones, and Jamil Natour. "Orthosis for rhizarthrosis: A systematic review and meta-analysis." Seminars in Arthritis and Rheumatism, Vol. 48, No. 5, 2019, pp. 778-90.
- Russo, Sergio, et al. "Treatment of the trapeziometacarpal osteoarthritis by arthroplasty with a pyrocarbon implant." International Orthopaedics, Vol. 40, No. 7, 2016, pp. 1465-71.
- Ladd, Amy L., Julia Lee, and Elisabet Hagert. "Macroscopic and microscopic analysis of the thumb carpometacarpal ligaments: a cadaveric study of ligament anatomy and histology." The Journal of Bone and Joint Surgery. American Volume, Vol. 94, No. 16, 2012, pp. 1468.
- Chug, Manish, et al. "Outcome of uncemented trapeziometacarpal prosthesis for treatment of thumb carpometacarpal joint arthritis." Indian Journal of Orthopaedics, Vol. 48, No. 4, 2014, pp. 394-8.
- Kuczynski, K. "Carpometacarpal joint of the human thumb." Journal of Anatomy, Vol. 118, No. 1, 1974, pp. 119.
- Levangie, P. K., and C. C. Norkin. "Joint Structure and Function: A Comprehensive Analysis. ad. 2005." Philadelphia: FA Davis Company, 2005.
- Bettinger, Paul C., et al. "An anatomic study of the stabilizing ligaments of the trapezium and trapeziometacarpal joint." The Journal of Hand Surgery, Vol. 24, No. 4, 1999, pp. 786-98.
- Bettinger, Paul C., and Richard A. Berger. "Functional ligamentous anatomy of the trapezium and trapeziometacarpal joint (gross and arthroscopic)." Hand Clinics, Vol. 17, No. 2, 2001, pp. 151-68.
- Pellegrini Jr, Vincent D., Christopher W. Olcott, and Gary Hollenberg. "Contact patterns in the trapeziometacarpal joint: the role of the palmar beak ligament." The Journal of Hand Surgery, Vol. 18, No. 2, 1993, pp. 238-44.
- Eaton, Richard G., et al. "Ligament reconstruction for the painful thumb carpometacarpal joint: a long-term assessment." The Journal of Hand Surgery, Vol. 9, No. 5, 1984, pp. 692-9.
- Eaton, Richard G., and J. William Littler. "Ligament reconstruction for the painful thumb carpometacarpal joint." Journal of Bone and Joint Surgery (JBJS), Vol. 55, No. 8, 1973, pp. 1655-66.
- Ghavami, Ashkan, and Scott N. Oishi. "Thumb trapeziometacarpal arthritis: treatment with ligament reconstruction tendon interposition arthroplasty." Plastic and Reconstructive Surgery, Vol. 117, No. 6, 2006, pp. 116e-28e.
- Frizziero, Antonio, et al. "Six-months pain relief and functional recovery after intra-articular injections with hyaluronic acid (mw 500–730 KDa) in trapeziometacarpal osteoarthritis." Muscles, Ligaments and Tendons Journal, Vol. 4, No. 2, 2014, pp. 256.
- Mandl, Lisa A., et al. "Injectable hyaluronan for the treatment of carpometacarpal osteoarthritis: open label pilot trial." Current Medical Research and Opinion, Vol. 25, No. 9, 2009, pp. 2103-8.
- Gervis, W. H. "Excision of the trapezium for osteo-arthritis of the trapezio-metacarpal joint." Postgraduate Medical Journal, Vol. 24, No. 271, 1948, pp. 262.
- Hentz, Vincent R. "Surgical treatment of trapeziometacarpal joint arthritis: a historical perspective." Clinical Orthopaedics and Related Research®, Vol. 472, No. 4, 2014, pp. 1184-9.
- Hattori, Yasunori, et al. "Arthrodesis for primary osteoarthritis of the trapeziometacarpal joint in elderly patients." The Journal of Hand Surgery, Vol. 41, No. 7, 2016, pp. 753-9.
- Gervis, W. H. "A review of excision of the trapezium for osteoarthritis of the trapezio-metacarpal joint after twenty-five years." The Journal of Bone and Joint Surgery. British Volume, Vol. 55, No. 1, 1973, pp. 56-7.
- Gervis, W. Harvey. "Excision of the trapezium for osteoarthritis of the trapezio-metacarpal joint." The Journal of Bone and Joint Surgery. British Volume, Vol. 31, No. 4, 1949, pp. 537-9.
- Menon, J. "Partial trapeziectomy and interpositional arthroplasty for trapeziometacarpal osteoarthritis of the thumb." Journal of Hand Surgery, Vol. 20, No. 5, 1995, pp. 700-6.
- Trumble, Thomas E., et al. "Thumb trapeziometacarpal joint arthritis: partial trapeziectomy with ligament reconstruction and interposition costochondral allograft." The Journal of Hand Surgery, Vol. 25, No. 1, 2000, pp. 61-76.
- Swanson, Alfred B. "Disabling arthritis at the base of the thumb: treatment by resection of the trapezium and flexible (silicone) implant arthroplasty." Journal of Bone and Joint Surgery (JBJS), Vol. 54, No. 3, 1972, pp. 456-71.
- Hofammann, Dabney Y., D. C. Ferlic, and M. L. Clayton. "Arthroplasty of the basal joint of the thumb using a silicone prosthesis. Long-term follow-up." The Journal of Bone and Joint Surgery. American Volume, Vol. 69, No. 7, 1987, pp. 993-7.
- Pellegrini, Vincent D., and Richard I. Burton. "Surgical management of basal joint arthritis of the thumb. Part I. Long-term results of silicone implant arthroplasty." Journal of Hand Surgery, Vol. 11, No. 3, 1986, pp. 309-24.
- Peimer, Clayton A. "Long-term complications of trapeziometacarpal silicone arthroplasty." Clinical Orthopaedics and Related Research®, Vol. 220, 1987, pp. 86-98.
- MacDermid, Joy C., et al. "Trapezial arthroplasty with silicone rubber implantation for advanced osteoarthritis of the trapeziometacarpal joint of the thumb." Canadian Journal of Surgery, Vol. 46, No. 2, 2003, pp 103.
- Nilsson, Anders, et al. "Results from a degradable TMC joint spacer (Artelon) compared with tendon arthroplasty." The Journal of Hand Surgery, Vol. 30, No. 2, 2005, pp. 380-9.
- Clarke, Sylvan, et al. "Complications with the use of Artelon in thumb CMC joint arthritis." Hand, Vol. 6, No. 3, 2011, pp. 282-6.
- Jörheim, Maria, et al. "Short-term outcomes of trapeziometacarpal artelon implant compared with tendon suspension interposition arthroplasty for osteoarthritis: a matched cohort study." The Journal of Hand Surgery, Vol. 34, No. 8, 2009, pp. 1381-7.
- De La Caffiniere, JY al, and P. Aucouturier. "Trapezio-metacarpal arthroplasty by total prosthesis." Hand, Vol. 11, No. 1, 1979, pp. 41-6.
- Nicholas, R. M., and J. W. Calderwood. "De la Caffiniere arthroplasty for basal thumb joint osteoarthritis." The Journal of Bone and Joint Surgery. British Volume, Vol. 74, No. 2, 1992, pp. 309-12.
- Woodward, Joseph F., Justin B. Heller, and Neil F. Jones. "PyroCarbon implant hemiarthroplasty for trapeziometacarpal arthritis." Techniques in Hand & Upper Extremity Surgery, Vol. 17, No. 1, 2013, pp. 7-12.
- Parker, Wendy L., et al. "Preliminary results of nonconstrained pyrolytic carbon arthroplasty for metacarpophalangeal joint arthritis." The Journal of Hand Surgery, Vol. 32, No. 10, 2007, pp. 1496-505.
- Wittemann, M., et al. "The Epping resection-suspension arthroplasty procedure. A standard procedure in the operative treatment of trapeziometacarpal osteoarthrosis?." Handchirurgie, Mikrochirurgie, plastische Chirurgie: Organ der Deutschsprachigen Arbeitsgemeinschaft fur Handchirurgie: Organ der Deutschsprachigen Arbeitsgemeinschaft fur Mikrochirurgie der Peripheren Nerven und Gefasse: Organ der V, Vol. 34, No. 1, 2002, pp. 49-58.
- Hart, R., et al. "Interposition suspension arthroplasty according to Epping versus arthrodesis for trapeziometacarpal osteoarthritis." European Surgery, Vol. 38, No. 6, 2006, pp. 433-8.
- Kennedy, Colin D., Mary Claire Manske, and Jerry I. Huang. "Classifications in brief: The Eaton-Littler classification of thumb carpometacarpal joint arthrosis." Clinical Orthopaedics and Related Research, Vol. 474, 2016, pp. 2729-33.
- Kapandji, A. "Clinical test of apposition and counter-apposition of the thumb." Annales de chirurgie de la main: organe officiel des societes de chirurgie de la main, Vol. 5, No. 1, 1986, pp. 67.
- Hudak, P L et al. "Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). " American Journal of Industrial Medicine, Vol. 29, No. 6, 1996, pp. 602-8.
- Vandenberghe, Lore, et al. "Long term outcome of trapeziectomy with ligament reconstruction/tendon interposition versus thumb basal joint prosthesis." Journal of Hand Surgery (European Volume), Vol. 38, No. 8, 2013, pp. 839-43.
- Santos, Claudia, et al. "Surgical treatment of rhizarthrosis: trapeziectomy with or without ligamentoplasty versus total prosthesis." Revista Brasileira de Ortopedia (English Edition), Vol. 46, No. 1, 2011, pp. 83-6.
- Mariconda, M., et al. "Partial trapeziectomy and pyrocarbon interpositional arthroplasty for trapeziometacarpal joint osteoarthritis: results after minimum 2 years of follow-up." Journal of Hand Surgery (European Volume), Vol. 39, No. 6, 2014, pp. 604-10.
- Lauwers, T. M. A. S., et al. "Early outcomes of Pyrocardan® implants for trapeziometacarpal osteoarthritis." Hand surgery and Rehabilitation, Vol. 35, No. 6, 2016, pp. 407-12.
- Degeorge, Benjamin, et al. "Do trapeziometacarpal prosthesis provide better metacarpophalangeal stability than trapeziectomy and ligamentoplasty?." Orthopaedics & Traumatology: Surgery & Research, Vol. 104, No. 7, 2018, pp. 1095-100.
- Kubát, P., and L. Trtík. "Maïa trapeziometacarpal implant for treatment of advanced osteoarthritis of the basal joint of the thumb." Acta chirurgiae orthopaedicae et traumatologiae Cechoslovaca, Vol. 79, No. 6, 2012, pp. 520-3.
- Ulrich-Vinther, M., H. Puggaard, and B. Lange. "Prospective 1-year follow-up study comparing joint prosthesis with tendon interposition arthroplasty in treatment of trapeziometacarpal osteoarthritis." The Journal of Hand Surgery, Vol. 33, No. 8, 2008, pp. 1369-77.
- Klein, Silvan M., et al. "Long-term results after modified Epping procedure for trapeziometacarpal osteoarthritis." Archives of Orthopaedic and Trauma Surgery, Vol. 135, No. 10, 2015, pp. 1475-84.
- Jurča, J., M. Nemejc, and V. Havlas. "Surgical treatment for advanced rhizarthrosis. Comparison of results of the Burton-Pellegrini technique and trapeziometacarpal joint arthroplasty." Acta Chirurgiae Orthopaedicae et Traumatologiae Cechoslovaca, Vol. 83, No. 1, 2016, pp. 27-31.