Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 0, Issue 0
The Level of Knowledge of Anesthesiologist Residents About Difficult Airway Management
Luiz Eduardo Imbelloni1*, Bárbara Tayná Paes Ferreira1, Nuha Alabduljabbar1, Eduardo Piccinini Viana1, Jaime Weslei Sakamoto1, André Augusto de Araujo2 and Geraldo Borges de Morais Filho22Master in Labour Economics, Universidade Federal Da Paraíba, Paraíba, Brazil
Co-responsible for CET-SBA, Anesthesiolo. Luiz Eduardo Imbelloni, Department of Anesthesiology & Hospital Clínicas Municipal de São Bernardo do Camp, Brazil, Email: dr.imbelloni@hotmail.com
Received: 05-Jul-2021 Accepted Date: Jul 12, 2021 ; Published: 26-Jul-2021
Abstract
Background: Airway management continues to be one of the main challenges for anesthesiologists, so it is essential that these professionals know about the anatomy and functioning of the airways since the beginning of their residency, not only for the safe application of anesthesia, but also for avoid unwanted complications with risk of permanent sequelae and even death. The aim of this study was to assess the degree of knowledge of anesthesiology residents in handling difficult airways.
Methods: The prospective comparative study was carried out at the Hospital de Clínicas Municipal of São Bernardo do Campo, belonging to the Brazilian Health System (SUS) recently accredited by the Canadian company Qmentum, of among students of three years of medical residency in anesthesiology of both sexes, with the application of a printed multiple-choice questionnaire on difficult airway management, carried out in January 2021. For statistical analysis it was using Microsoft Excel spreadsheet and R Commander from software R version 4.1.0. We used the literature standard p-value as significance to be 0.05.
Results: Fifteen residents were interviewed (6 R1, 5 R2 and 4 R3) with an average age of 31 years. An increase in the learning of residents after three years was noticed in the following aspects: anatomy of the difficult airway management, Mallampati and Cormack classification, supraglottic devices, difficult airway management case equipment and difficult airway anagement algorithm. On the other hand, the predictors of difficult airway management and difficult ventilation under mask obtained a lower-than-expected result. In general, there was a better performance and confidence in those who have already participated in some difficult airway training.
Conclusion: This study allowed us to assess that at the end of the residency, students' learning increased significantly, as well as their confidence, especially in those who had already done some training in difficult airway management, such data point to the importance of investing in training on the topic.
Keywords
Airway management, Difficult airway, Intubation, Training
Introduction
Airway management remains one of the main challenges for anesthesiologists. Although advances in the development of new airway devices and well-defined algorithms that guide the conduct of emergencies have reduced the complications of a difficult airway, it is essential that these professionals know about the anatomy and functioning of the airways since the beginning of residency, not only for safe application of anesthesia, but above all to avoid undesirable complications with the risk of permanent sequelae and even death [1].
The difficult airway is defined as the clinical situation in which the conventionally trained physician has difficulty ventilating with a mask, difficulty with orotracheal intubation or both [2]. It is a complex interaction between factors of the patient, the clinical picture, the skill and experience of the doctor.
Difficult ventilation is the inability of an anesthesiologist to maintain patient saturation above 90%, using a face mask as a means of ventilation and 100% inspired oxygen, with oxygen saturation within normal values prior to ventilation [3]. Difficult intubation is defined as the need for three or more attempts at intubation, or a total duration of the procedure that exceeds 10 minutes [3]. However, difficult ventilation with a face mask is a situation that is often associated with difficult intubation. An adequate physical examination of the airway in search of predictors for a difficult airway is essential in preanesthetic evaluation.
In order to help in clinical practice in relation to intubation, guidelines with basic recommendations have been published that have become pillars of training programs in anesthesia and clinical practice [4-7]. These guides and algorithms play a key role in preserving patient safety, recommending specific plans and strategies for dealing with difficult expected or unexpected airways. Its effectiveness depends on the proficiency of its users, and training in various airway management techniques is mandatory. Despite this, not all users in training, or even experienced physicians, have complete competence in current difficult airway algorithms or techniques [8].
In order to help in clinical practice in relation to intubation, guidelines with basic recommendations have been published that have become pillars of training programs in anesthesia and clinical practice [4-7]. These guides and algorithms play a key role in preserving patient safety, recommending specific plans and strategies for dealing with difficult expected or unexpected airways. Its effectiveness depends on the proficiency of its users, and training in various airway management techniques is mandatory. Despite this, not all users in training, or even experienced physicians, have complete competence in current difficult airway algorithms or techniques [8].
Methods
This study was carried out in accordance with the Research Norms involving Human Beings (Rs. CNS 196/96) of the National Health Council, after being registered at Plataforma Brasil (CAAE: 36294520.4.0000.5625) and approved by the Research Ethics Committee (opinion 4,393,649), and signing the Free and Informed Consent Form.
This is a prospective comparative study, based on the application of a questionnaire on the management of difficult airways (APPENDIX A). The study was carried out at the Hospital de Clínicas Municipal of São Bernardo do Campo, belonging to the Brazilian Health System (SUS) recently accredited by the Canadian company Qmentum, with the anesthesiology residents of both sexes of the hospital. The residency in Anesthesiology (MEC/SBA) consists of a total of 18 doctors, six from the first year (R1), six from the second year (R2) and six from the third year (R3). The exclusion criterion was the refusal to answer the questionnaire and and the researcher (3rd year resident) for ethical reasons to research.
The variables included in the analysis were: demographic data; current year of residence; general questions about airway knowledge regarding anatomy, predictors of difficult airway, difficult ventilation, supraglottic devices and Difficult Airway Management (DAM); bronchoscope and videolaryngoscope management; number of DAM cases seen in the last six months; presence or absence of planning and equipment for handling the case; feeling of security to handle the case and participation in difficult airway training.
The questionnaires were stored in a sealed urn, and the data obtained were organized in a database in the form of a spreadsheet and subsequently subjected to descriptive analysis. Microsoft Office Excel 2019 softwares were used for data analysis and making tables and figures.
Statistical Methods
To analyze the data we use graphs ans descriptive measures to summarize the information. Association between categorical variables can be viewed through the mosaic plot. A mosaic plot (also known as a Marimekko diagram) is a graphical method for visualizing data from two or more qualitative variables. It is the multidimensional extension of spineplots, which graphically display the same information for only one variable. Associations between categorical variables are measured using the chisquare independence test with Yates correction. The outputs were generated using a Microsoft Excel spreadsheet and R Commander from software R version 4.1.0. We used the literature standard p-value as significance to be 0.05.
Results
Of the 18 residents, 15 responded to the questionnaire, six of whom were first- year residents, five of the second year, and four of the third year, eight women and seven men. The average age was 31.27 ± 3.55 years, ranging from 26 to 37 years. The excluded were one for refusing to complete the questionnaire, another for being away due to Covid and the researcher of the study.
The Table 1 presents percentages about direct questions with Yes or No answers when applied. There was no difference in the assessment of predictors of difficult airways among residents (Question 3rd). All residents knew that there was a variety of equipment available for DAM (Question 4th). Over the years there has been a significant increase in planning before surgery in case of DAM (Question 5th). Regarding the handling of the bronchofibroscope, there was a significant increase with years of residence (Question 6th). Even over the years, residents do not feel able to handle the bronchofibroscope (Question 10th). There was no difference between residents R1, R2 and R3 regarding the use of all materials in the DAM case (Question 13th).
| Questions | R1 | R2 | R3 | p-value | |||
|---|---|---|---|---|---|---|---|
| Yes | No | Yes | No | Yes | No | ||
| 3rd | 4 | 2 | 4 | 1 | 3 | 1 | 0.88 |
| 4th | 6 | 0 | 5 | 0 | 4 | 0 | - |
| 5th | 3 | 3 | 5 | 0 | 4 | 0 | 0.06* |
| 6th | 2 | 6 | 3 | 2 | 3 | 1 | 0.03* |
| 7th | 2 | 4 | 3 | 2 | 3 | 1 | 0.40 |
| 10th | 0 | 6 | 5 | 0 | 4 | 0 | 0.00* |
| 13th | 1 | 5 | 2 | 3 | 3 | 1 | 0.18 |
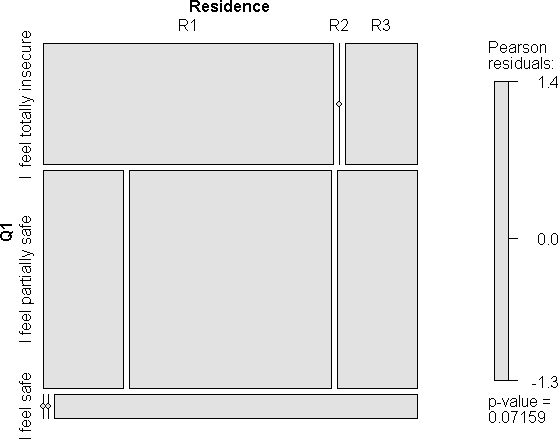
Over the years, residents feel significantly safer in approaching patients with difficult airways. There is no significant difference between the different degrees of residence (p=0.07) (Figure 1).
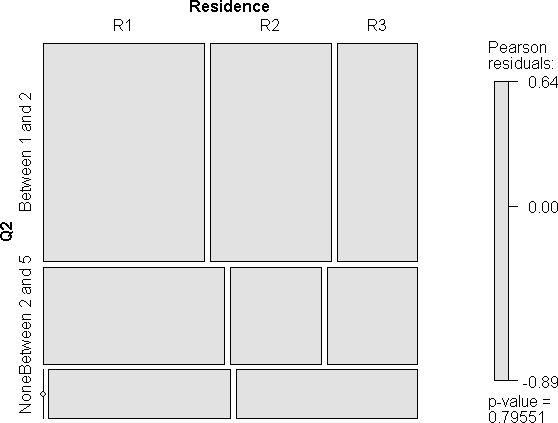
Regarding the number of cases of DMA, residents experienced in the last six months, all residents (R1, R2, R3) witnessed some case. Using the Pearson test there is no difference between residents of different years. (Figure 2).
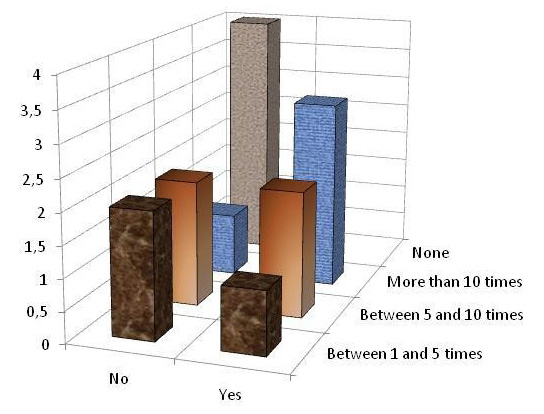
Regarding the handling of bronchofibroscope and videolaryngoscope, most of the 1st year residents stated that they were not able and had little contact with this equipment, whereas 75% of the 3rd residents said they knew how to handle and had greater contact. Using the Pearson test, there is no significant difference between 1st, 2nd and 3rd year residents (Figure 3).
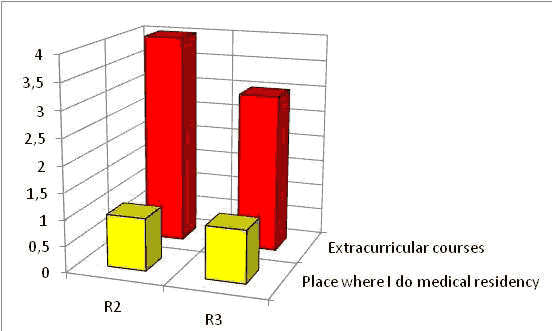
Regarding some training on DAM. All second and third years residents reported that they had already taken at least one training course on the topic, with 80% of 2nd year residents and 75% of 3rd year residents in extracurricular courses, with no significant difference. Regarding 1st year residents, none participated in any training course. Among the reasons for this result, 50% reported that the residency had not offered these courses, another 50% reported that they did not have the financial resources to do so (Figure 4).
About the residents' knowledge about difficult airways, with respect to the anatomy of the airways, where an increase was noticed over the years (R1=33%; R2=80%; R3=100%). Regarding the predictors of DAM, the study revealed correct answers of 16% among R1, 40% among R2 and 50% among R3. Regarding predictors of difficult ventilation under a mask, there was a decrease in correct answers over the first and last year (R1=33%; R2=20% and R3=25%). Regarding the knowledge of supraglottic devices, the highest percentage of correct answers was borne by first-year residents with 83%. Regarding the knowledge of the equipment available in the DAM case, only 16% of the R1 said they did, while in the following years the responses were 40% and 75%, between the R2 and R3, respectively. In none of these items was there a significant difference between residents of the various years.
Regarding the last algorithm launched in 2013 by the American Society of Anesthesiology, there was a significant increase in learning over the years of residency, with R1 with 66%, R2 with 80% and R3 with 100%. Regarding the Mallampati and Cormack-Lehane classifications, it was noticed that the Mallampati scale is best known among all the interviewed residents.
Regarding the safety of residents in relation to handling difficult airways, 66% of 1st year residents reported being totally insecure and 100% of 2nd year residents said they were partially safe. Among 3rd year residents, there was variation between responses: 25% felt totally insecure, 50% partially safe and 25% safe.
Discussion
Difficult airway management is a critical aspect of anesthesiology training and practice. Anesthesiology residency education in Brazil corresponds to three years, focusing on acquiring knowledge and skills during this training period. Our study, through a questionnaire, demonstrated that training in airways occurs a considerable increase in knowledge after each year of residency. An increase in the learning of residents after three years was noticed in the following aspects: anatomy of the airways, Mallampati and Cormack classification, supraglottic devices, equipment of the difficult airway bag and guidelines and algorithm for intubation.
One of the biggest concerns when performing an anesthetic procedure is undoubtedly related to the airway and its proper maintenance. The presence of a difficult, unanticipated airway is always a major challenge that can often lead to catastrophe [2,3]. Airway management in critically ill patients differs significantly from tracheal intubation carried out for a routine surgical procedure. In the operating room, most intubations are done under elective, controlled conditions by skilled physicians formally trained in airway management; the complication rate is low.
The “can’t intubate can’t situation ventilate” occurs in fewer than 1 in 5,000 routine general anesthetics and may be responsible for and requires an emergency to 25% of anesthesia-related deaths [9]. In this study, there was an alarming result in relation to the knowledge of predictors of difficult airway by anesthesiology residents, as it was found that only 50% of 3rd year residents were successful in this regard. It was expected that at the end of the three years this knowledge would already be rooted in the residents' daily lives. On the other hand, when questioned about the anatomical knowledge of the airways, it was noticed that this increased over the years in the residence (R3>R2> R1).
The hospital where this study was conducted belongs to the Brazilian Health System (SUS) recently accredited by the Canadian company Qmentum. Accreditation systems have emphasized the importance at all stages of patient care.
The assessment of competence in education in anesthesiology has been relatively easy due to the large volume of care provided by residents under direct observation of the teaching staff in the operating room. The distinction between evaluation and assessment is a move towards the use of reliable quantitative tools with a measurable level of objectivity [10]. Airway management training fits into these concepts.
It is important to note that knowing the anatomy and knowing how to perform an adequate physical examination of the airways in search of predictors that can alert you to a possible difficult airway is very useful in pre-anesthetic evaluation [1]. This study showed that there was an increase in knowledge to assess predictors of difficult airways, showing that the residence fulfilled its objective.
Education and training in advanced airway management as part of an anesthesiology residency program is necessary to help residents attain the status of expert in difficult airway management. This study with a small number of residents (18 in total) showed that the three years of residency in Brazil in an Anesthesiology Service of a tertiary hospital is not sufficient to learn all the new intubation techniques in patients with previously difficult airways, as only 50% consider themselves fit for safety in this procedure. Education and training in advanced airway management as part of an anesthesiology residency program is necessary to help residents attain the status of expert in difficult airway management. Otherwise, there is a need for extracurricular courses to improve this procedure.
Laryngoscopy and tracheal intubation are one of the pillars in airway management during general anesthesia and it is usually done without complications. A study carried out in an Intensive Care Unit (ICU) showed that orotracheal intubation method used for the first attempt in patients with a difficult or unremarkable airway was Macintosh laryngoscopy alone in 83.3% of attempts; a stylet or bougie with Macintosh laryngoscopy in 8.9% and 3.3% of attempts, respectively; a videolaryngoscope in 3.3% of attempts; and a videolaryngoscope with a stylet in 1.1% of attempts. When intubation proved difficult despite good visualization of the glottis, a bougie was used in 85.6%, a videolaryngoscope in 14/180 (7.8%) ICUs, and a stylet in 6.6% of attempts [11]. A similar study in the operating room was not found in the consulted literature.
Accreditation in any hospital emphasizes that anesthesiology residents must obtain significant experience with a broad spectrum of airways management techniques. However, there is no specific number required as a minimum clinical experience that should be obtained in order to ensure competency. This was observed in this study showing that at the end of the residency with a requirement of 400 procedures per year in Brazil, they are not enough to prepare an anesthesiologist for difficult airways.
In 2011, a program for training in advanced airway techniques was developed, complemented with a practical workshop on difficult airways [12]. This same training program exists in Brazil, showing that these extracurricular courses are important for the safety of handling patients' airways. Simulation training for difficult airway management offers learning opportunities.
A French group researched whether a three- hour simulation training would improve learning six months after training, demonstrated that there improved the frequency of use of devices by residents [13].
In this study, when asked to the residents about the knowledge of the devices present in the hospital's difficult airway bag, 16% of the first year residents, 40% of the second year and 75% of the third year reported knowing about it. It is noteworthy that this knowledge must be mandatory for all physicians who manipulate the airway, as it is essential to perform intubation in case of difficult airway. It is known that most of the devices indicated for the maintenance of airway functions are destined to its upper portion, called extra-glottic, periglottic or supra-glottic devices. In this study, when asked to residents about the knowledge of these devices, there was a decrease in correct answers (R1=83%; R2=80%; R3=75%), with no significant difference. This fact is extremely worrying, as these devices are extremely important to maintain the patient's urgent oxygenation in case of failure to intubate in a DAM situation [14]. This knowledge was expected to increase over the course of the residency because they are such essential devices in clinical practice [15,16].
Conclusion
Intubation training is one of the most important subjects in the curriculum of anesthesiology residents. The teaching of intubation skills to 1st year anesthesiology residents through workshops on mannequins showed a significant improvement in knowledge but was not confirmed in a control study. Mallampati and Comarck- Lehane classifications when used together they have a greater chance of predicting the difficult airway. Management of the difficult airway is an essential skill that should be taught during na anesthesiology residency. However, only a minority of anesthesiology residency programs have formal rotations in advanced airway management. In our hospital there are all the modern devices for handling difficult airways, and each year the residents train the different methods.
References
- Andrade, R. G. A. C., et al. "Dificuldade na laringoscopia e na intubação orotraqueal: Estudo observacional." Rev Bras Anestesiol 68.2 (2018):168-173.
- Figueiredo, L. F. P., and Ferez, D. "Diretrizes para o manejo da via aérea difícil."Rev Assoc Med Bras 49.2 (2003): 129-130.
- Reed, M. J., Dunn, M. J. G., and McKeon, D. W. "Can an airway assessment score predict difficulty at intubation in the emergency department?" Emerg Med J 22.2 (2005): 99- 102.
- Henderson, J. J, Popat, M. T, Latto, I. P, and Pearce, A. C. "Difficult airway society guidelines for management of the unanticipated difficult intubation." Anaesthesia 59 (2004): 675- 694.
- Frerk, C., et al. "Difficult airway society 2015 guidelines for management of unanticipated difficult intubation in adults." Br J Anaesth 115.6 (2015): 827-848.
- Frova, G., and Sorbello, M. "Algorithms for difficult airway management: A review." Minerva Anesthesiol 75 (2009): 201-209.
- Gómez-Ríos, A., et al. "Guías y algoritmos para el manejo de la vía aérea difícil. Formación Continuada." Rev Esp Anestesiol Reanim 65.1 (2018):41- 48.
- Tanaka, P. P., Pessoa, R., Fernandes, R, and Brodsky, J. "What is missing for difficult airway management in the 21st century. Letter to Editor." Rev Bras Anestesiol 65.3 (2015): 235-236.
- Cook, T. M., and MacDougall-Davis, S. R. "Complications and failure of airway management." Br J Anaesth 109. S1 (2012): i68–i85.
- Pagano, L. "A new vocabulary and other innovations for improving descriptive in- training evaluations. "Acad Med 74 (1999): 1203-1207.
- Martin, M., et al. "Nationwide survey on training and device utilization during tracheal intubation in French intensive care units." Ann Intensive Care 10 (2020): 2.
- Borovcanin, Z., and Shapiro, J. R. "Design and implementation of an educational program in advanced airway management for anesthesiology residents. Review article."Anesthesiology Research and Practice, 737151 (2012): 1-7.
- Lilot, M., et al. "Simulation of difficult airway management for residents: Prospective comparative study." Rev Bras Anestesiol 69.4 (2019): 358-368.
- Metterlein, T., et al. "A comparison of various supraglottic airway devices for fiberoptical guided tracheal intubation." Rev Bras Anestesiol 67.2 (2017): 166-171.
- Etezadi, F., et al. "An assessment of intubation skill training in novice anesthesiology residents of Tehran university of medical sciences with the use of mannequins." Pain Med6.6 (2016):e39184.
- Kai, L. K., et al. "Frequency of difficult airway tract in patients submitted to general anesthesia in south Santa Catarina hospital." Arq Catarin Med 49.3 (2020): 101-110.