Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 1
The Bacterial Colonization in Patients with Chronic Obstructive Pulmonary Disease (COPD)
Fadhil Husam Ahmed*Fadhil Husam Ahmed, Department of Medical Lab Techniques, College of Medical Technology, Al-Farahidi University, Baghdad, Iraq, Email: fadhilhusam20@gmail.com
Received: 02-Dec-2020 Accepted Date: Jan 22, 2021 ; Published: 29-Jan-2021
Abstract
This study investigates the bacterial colonies’ numbers in COPD patients. Two groups of people were included in this study; 25 healthy individuals’ groups and 32 COPD patients’ groups, which were further subdivided into three subgroups; 12 smokers, 13 secondhand smokers, and 7 nonsmokers. The sputum sample of each individual was collected to identify bacterial colonization. The results showed different types of bacterial isolates in the two studied groups. Streptococcus pneumonia and Staphylococcus aureus are the most common bacterial isolates in the patients’ group. The numbers of bacterial colonization among the COPD individual are greater than the healthy individual group.
Keywords
COPD, Lung functions, Bacterial colonies
Introduction
Chronic Obstructive Pulmonary Disease (COPD) is a chronic inflammatory lung disease that restricted the lung’s airflow. World Health Organization described that COPD is not one single disease but an umbrella term used to describe chronic lung diseases that cause limitations in lung airflow. The airflow restriction is mostly progressive and related to an abnormal inflammatory reaction of the lungs to harmful atoms or gases. COPD considers the top 10 causes of death that has an increasing prevalence and mortality. It is characterizing by a progressive weakening in lung function and inflammatory changes [1-6]. Previous studies have decided that patients with COPD have bacterial colonization in the lower respiratory tract which may be a significant construction of airway inflammation [7,8]. The main clinical findings of COPD include shortness of breath, cough, and production of sputum with acute exacerbations periods that characterizes by increased cough, more breath shortness, changing of the sputum color, and increase in production of sputum [9,10]. The most important factor to cause inflammation in the lung is smoking which leads to the progression of COPD caused by bacterial colonization [5,11-13]. Stable chronic obstruction patients showing more airway inflammation and the grade of inflammation is positively related to the severity of airway obstruction with more bronchial inflammation in patients with lower FEV1 (Forced Expiratory Volume at the first second of expiration) [14-17]. Earlier studies performed to evaluate the relationship between the airway’s bacterial colonization, inflammation, and lung function have been cross-sectional in design, and have note spoke the important relationship between these parameters [18-20]. Additional study has talking that bacterial colonization leads to increase airway inflammation and can contribute to the accelerated progression of airway obstruction [13,21].
The Aim of the Study
The study was aimed to investigate the most common bacterial colonies in COPD patients during the stable state as compared with healthy peoples, and to show the number of bacterial colonies with a decline in lung function as reflected by lung volume measurement.
Materials and Methodology
Patients Sample
This study was carried out on two groups: 32 patients with COPD within the range of age (26-65), and 25 healthy subjects as a control, within the age range (28-62 years old). COPD patients’ group was more subdivided into three subgroups: 12 smokers, 13 second hand smokers, and 7 non smokers.
Collections of Sputum Sample
Samples of Sputum were kept in a sterile container from each individual and analyzed bacteriologically by culturing on; MacConkey agar, blood agar, and nutrient agar. The Petri dishes were incubated for 24 hrs at 37°C. Bacterial isolates were diagnosed roughly according to the appearance of colonies and gram staining.
Evaluation of Lung Function
Lung function was rating by measurement of the pulmonary function tests FEV1 (Forced Expiratory Volume), FVC (Forced Vital Capacity), and FEV1% (the ratio of FEV1/FVC) which are the most common parameters used to evaluate the lung function and to give the respiratory diagnosis if the individual was healthy or with allergic lower airway disease such as COPD. The medical instrument used to measure the lung volumes is the medical micro lab spirometer.
Results
The findings of lung function tests are showing significant variations between the two studies groups in the three main lung functions tests FEV1, FVC, and FEV1%, illustrated in Table 1, and also find seven bacterial strains isolated from the patients with COPD. The most common bacterial isolates included are Streptococcus pneumonia and E. coli. While 3 bacterial strains were isolated from the healthy group, most of them belong to Streptococcus pyogenes (Figure 1).
| Groups | Number of Patients | FEV1 | FVC | FEV1% | Number of bacterial types | The most common bacterial colonies |
|---|---|---|---|---|---|---|
| Mean | ||||||
| COPD patients’ group | 32 | 2.55 | 3.39 | 75.22% | 7 | Streptococcus pneumonia |
| Healthy group | 25 | 3.59 | 3.95 | 90.89% | 4 | Streptococcus spp. |
Table 1: Illustrated the three main lung functions, the number of bacterial types, and the most bacterial strain in the main study.
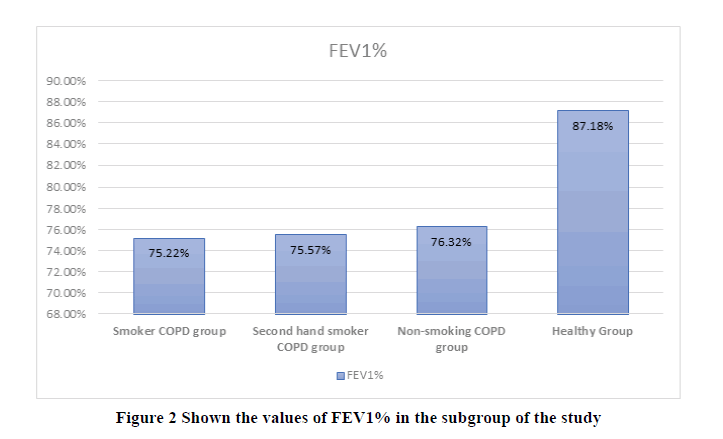
Table 2 shows the values of pulmonary function tests and the differences between the subgroups of the COPD group and the healthy group. This table shows that there are significant variances between the smoker, second-hand smoker, and non-smoking patients and the healthy group in all pulmonary function tests FEV1, FVC, and FEV1%. There are also significant variances between COPD smoking patients and healthy subjects in FEV1, FVC, and FEV1% (Figure 2). On the other hand, there is no significant difference between the three subgroups smoking, second-hand smoker, and non-smoking of the COPD patients in all of these lung parameters. The table also shows that smoker COPD patients have the highest number (7) of bacterial isolates types, and the most common bacterial isolates are Staphylococcus aureus and E coli.
| Groups | Number of Patients | FEV1 | FVC | FEV1% | Number of bacterial types | The most common bacterial colonies |
|---|---|---|---|---|---|---|
| Mean | ||||||
| Smoker COPD group | 12 | 2.55 | 3.39 | 75.22% | 7 | Staphylococcus aureus |
| Second hand smoker COPD group | 13 | 2.63 | 3.48 | 75.57% | 6 | E. coli |
| Non-smoking COPD group | 7 | 2.74 | 3.59 | 76.32% | 6 | Streptococcus pneumonia |
| Healthy group | 25 | 3.4 | 3.9 | 87.18% | 4 | Streptococcus viridans |
Table 2: Illustrated the values of pulmonary functions tests, numbers of bacterial types, and most common bacterial colonies in the subgroup of the study.
Table 3 shows lung function tests FEV1, FVC, and FEV1% expressed by mean in each isolation of bacteria and the percentage of COPD patient’s bacterial isolates. Staphylococcus aureus and E. coli are the most dominant bacterial isolates within these subgroups, which showing near the same percentage. Infected patients by these bacterial isolates Staphylococcus aureus and E. coli have the lowest value of FEV1: (2.2 and 2.25) respectively. While the lowest value of FEV1% was for the patients infected by Streptococcus pneumonia, the next dominant bacterial isolates (Figure 3).
| No. | Bacterial Isolate | Percentage | Mean | ||
|---|---|---|---|---|---|
| FEV1 | FVC | FEV1% | |||
| 1 | Staphylococcus aureus | 70.5 | 2.2 | 3.1 | 70.97% |
| 2 | E. coli | 70.9 | 2.25 | 3.14 | 71.66% |
| 3 | Pseudomonas | 11.7 | 2.75 | 3.35 | 82.09% |
| 4 | Staphylococcus + Streptococcus | 12.1 | 2.81 | 3.39 | 82.89% |
| 5 | Streptococcus pneumonia | 40.3 | 2.53 | 3.57 | 70.11% |
| 6 | Proteus | 11.9 | 3.16 | 3.93 | 80.41% |
| 7 | Klebsiella | 28.5 | 3.19 | 14.1 | 77.80% |
Table 3: Illustrated the percentage of bacteria isolation and lung function tests of bacterial isolates of COPD patients.
Discussion
The results of data analysis of this study proved that there is a significant decline in the lung volumes studied FEV1, FVC, and FEV1% of the COPD patients, even during the stable state. A similar finding was observed by another study [22]. The statistical analysis showed that COPD patients have different types of bacterial colonization from sputum samples than healthy groups. There are about seven bacterial strains in COPD patients. These are Staphylococcus aureus, E. coli, Pseudomonas, Staphylococcus with Streptococcus, Streptococcus pneumonia, Proteus, and Klebsiella. The healthy group has three types of bacteria only. These are Streptococcus pyogens, Streptococcus viridans, and Staphylococcus epidermidis, as reported by many other studies [23-25], which identified the presence of bacterial colonization in the lower airways of healthy nonsmoking, while another study [18,19] founded that the lower airways of healthy nonsmoking persons are germ-free. In brief, the recent study showed that COPD patients have clear deterioration in lung function tests and increased bacterial colony variations. This result is continual with the other study finding that is the person showed changes in the bacterial colonization nature suffered from a faster decrease in lung function than those with the persistence of one or more bacterial species [26].
Conclusion
The main bacterial colonies in COPD patients were Streptococcus pneumonia, E. coli, and Staphylococcus aureus. This group shows clear declines in lung function tests FEV1, FVC, and FEV1%, compared to the healthy group, which their lower airways occupied by an alternative type of bacterial isolates: Streptococcus pyogenes and Streptococcus viridans generally. There is clear interaction in the lung volumes between subjects colonized with different bacteria within the same group. To find the final effect of bacterial colonies on lung function tests, more quantitative and qualitative detection is required.
Declerations
Conflicts of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Singh, P., S. Khan, and R. K. Mittal. "Renal function test on the basis of serum creatinine and urea in type-2 diabetics and nondiabetics." Bali Medical Journal, Vol. 3, No. 1, 2014, pp. 11-4.
- Asai, Kazuhisa, and Kazuto Hirata. "Definition of Chronic Obstructive Pulmonary Disease (COPD): Is the Latest GOLD Classification of Severity Still Valid?." Chronic Obstructive Pulmonary Disease, Springer, Singapore, 2017, pp. 3-16.
- Moghoofei, Mohsen, et al. "Bacterial infections in acute exacerbation of chronic obstructive pulmonary disease: a systematic review and meta-analysis." Infection, Vol. 48, No. 1, 2020, pp. 19-35.
- Alqahtani, Jaber S., et al. "Prevalence, severity and mortality associated with COPD and smoking in patients with COVID-19: a rapid systematic review and meta-analysis." PloS one, Vol. 15, No. 5, 2020, pp. e0233147.
- Zhang, Qingling, et al. "Bacteria in sputum of stable severe asthma and increased airway wall thickness." Respiratory Research, Vol. 13, No. 1, 2012, pp. 35.
- Barnes, P. J., and B. R. Celli. "Systemic manifestations and comorbidities of COPD." European Respiratory Journal, Vol. 33, No. 5, 2009, pp. 1165-85.
- Beck, J. M. "Et aii The microbiome of the lung Transl." Research, Vol. 160, No. 4, 2012, pp. 258-66.
- Martinez, Fernando J. "Pathogen-directed therapy in acute exacerbations of chronic obstructive pulmonary disease." Proceedings of the American Thoracic Society, Vol. 4, No. 8, 2007, pp. 647-58.
- Celli, B. R., and P. J. Barnes. "Exacerbations of chronic obstructive pulmonary disease." European Respiratory Journal, Vol. 29, No. 6, 2007, pp. 1224-38.
- Beasley, Victoria, et al. "Lung microbiology and exacerbations in COPD." International Journal of Chronic Obstructive Pulmonary Disease, Vol. 7, 2012, pp. 555.
- Hilty, Markus, et al. "Disordered microbial communities in asthmatic airways." PloS one, Vol. 5, No. 1, 2010, pp. e8578.
- Pragman, Alexa A., et al. "The lung microbiome in moderate and severe chronic obstructive pulmonary disease." PloS one, Vol. 7, No. 10, 2012, pp. e47305.
- Shukla, Shakti D., et al. "Microbiome effects on immunity, health and disease in the lung." Clinical and Translational Immunology, Vol. 6, No. 3, 2017, pp. e133.
- Jabbar, Azza Sajid, and Zainab S. Wrewsh. "Lung volumes and the most common bacterial colonization in patients with allergic airways disease." Journal of Basrah Researches (Sciences), Vol. 38, No. 3A, 2012, pp. 117-23.
- Wedzicha, Jadwiga A., and Terence AR Seemungal. "COPD exacerbations: defining their cause and prevention." The Lancet, Vol. 370, No. 9589, 2007, pp. 786-96.
- Tufvesson, Ellen, Leif Bjermer, and Marie Ekberg. "Patients with chronic obstructive pulmonary disease and chronically colonized with Haemophilus influenzae during stable disease phase have increased airway inflammation." International Journal of Chronic Obstructive Pulmonary Disease, Vol. 10, 2015, pp. 881.
- Rabe, Klaus F., et al. "Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary." American Journal of Respiratory and Critical Care Medicine, Vol. 176, No. 6, 2007, pp. 532-55.
- Wilkinson, Tom MA, et al. "Airway bacterial load and FEV1 decline in patients with chronic obstructive pulmonary disease." American Journal of Respiratory and Critical Care Medicine, Vol. 167, No. 8, 2003, pp. 1090-5.
- Patel, I. S., et al. "Relationship between bacterial colonisation and the frequency, character, and severity of COPD exacerbations." Thorax, Vol. 57, No. 9, 2002, pp. 759-64.
- Zhang, M., et al. "Relevance of lower airway bacterial colonization, airway inflammation, and pulmonary function in the stable stage of chronic obstructive pulmonary disease." European Journal of Clinical Microbiology and Infectious Diseases, Vol. 29, No. 12, 2010, pp. 1487-93.
- Uhliarova, Barbora, et al. "The effect of smoking on CT score, bacterial colonization and distribution of inflammatory cells in the upper airways of patients with chronic rhinosinusitis." Inhalation Toxicology, Vol. 26, No. 7, 2014, pp. 419-25.
- Sykes, Annemarie, Patrick Mallia, and Sebastian L. Johnston. "Diagnosis of pathogens in exacerbations of chronic obstructive pulmonary disease." Proceedings of the American Thoracic Society, Vol. 4, No. 8, 2007, pp. 642-6.
- Zalacain, R., et al. "Predisposing factors to bacterial colonization in chronic obstructive pulmonary disease." European Respiratory Journal, Vol. 13, No. 2, 1999, pp. 343-8.
- Monso, E., et al. "Risk factors for lower airway bacterial colonization in chronic bronchitis." European Respiratory Journal, Vol. 13, No. 2, 1999, pp. 338-42.
- Sudeena, D., S. B. Lal, and Kattamuri Ramesh Kumar. "Profile of bacterial culture and sensitivity from the sputum of chronic obstructive pulmonary patients with acute exacerbations." Asian Pacific Journal of Health Sciences, Vol. 4, No. 1, 2017, pp. 173-82.
- Adinoff, Allen. "Association between airway bacterial load and markers of airway inflammation in patients with stable chronic bronchitis." Pediatrics, Vol. 108, No. 2, 2001, pp. 574.