Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 6
Telemedicine: A Regulatory Approach
Prasannakumar P Bhat* and Balamuralidhara VPrasannakumar P Bhat, Department of Pharmaceutics, JSS College of Pharmacy, JSS Academy of Higher Education and Research, Mysuru, Karnataka, India, Email: baligowda@jssuni.edu.in
Received: 13-May-2021 Accepted Date: Jun 22, 2021 ; Published: 30-Jun-2021
Abstract
Tele Medicine was coined in the early 70s. It has a general meaning ‘Healing at the distance’ and it has the purpose of overcoming the barrier of geographies and the use of information and technologies for the betterment of health care service. In India Ministry of Health and Family Welfare, ISRO department of information and technologies made effort to make telemedicine possible and in the USA it was in effect from the 19th century only. American Telemedicine Association is the main association for telemedicine and various states have different guidelines.
Keywords
Telemedicine, American Telemedicine Association, Ministry of Health and Family Welfare, Medicine prescription
Introduction
Tele Medicine was coined in the early 70s. It has a general meaning ‘Healing at the distance’. WHO defines telemedicine as providing health care services to people who are at the distance from actual health care centers, using various Information technologies intended for prevention, diagnosis, treatment of diseases.
There are four purposes for telemedicine:
• To provide a good clinical strength
• To overcome the barrier between geographies to connect to the patients who are not at the same place
• To effectively use the types of Information and Technologies for the betterment of health care.
• The major purpose of Telemedicine is to improve the quality of health care [1]
Advantages of Telemedicine
• The most useful advantage is that it provides access to specialists in various fields with whom a consultation shall be made
• Transportation time and cost can be saved
• Eliminates the traveling issues to children and elder
• Less chance of catching a new illness
• Better health [2]
Some examples of telemedicine include Live Video Conferencing, Remote Patient Monitoring, Mobile Health/Health [3].
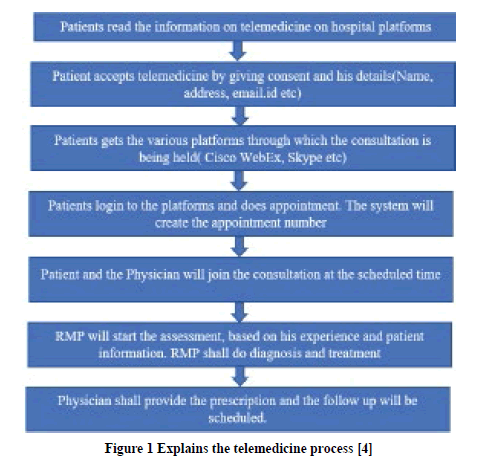
The general telemedicine process is given in Figure 1 in the below flowchart.
Figure 1. Explains the telemedicine process [4]
Telemedicine in India
As per the Ministry of Health and Family Welfare, Telemedicine can be defined as delivering health services to people where distance is a critical issue, using the ICT for prevention, diagnosis, treatment of patients [5]. Telemedicine practices in India are gaining an immense foothold recently. It was a combined effort from ISRO, Department of Information and Technology, Ministry of External Affairs, Ministry of Health and Family Welfare to introduce Telemedicine in India. In India, the telemedicine concept was made available in 2001 when ISRO linked the Apollo Chennai hospital to Apollo rural hospital in Andhra Pradesh. During the Covid-19 pandemic, telemedicine gained huge popularity and benefitted millions of people across the country [6]. The telemedicine industry will make a huge market by 2025 worth more than $5.4 Bn. The increased lifestyle diseases and a lot of pressure which is been created in the traditional medicine system have set up a great platform for telemedicine in India. Many start-ups like Practo, Doc Prime Call Health are currently operating in India with the regulatory grey area [7].
Only the Registered Medical Practitioner is permitted to provide telemedicine to the patients in India. They should follow the ethical and professional rules and standards while serving the people. There is a total of 7 key structures to be considered before providing telemedicine consultation.
They are:
Context: The RMP should use his experience to judge if telemedicine is required or not and also the technology available to treat the patients. It’s a Registered Medical Practitioner’s (RMP) duty to check the complexity of patients’ health conditions before conducting the telemedicine consultation.
Identifying the Registered Medical Practitioner and the patient: The consultation should go in hand with both RMP and patient knowing each other. RMP should collect the patient’s age, sex, address before the consultation.
Mode of communication: There is various kind of technologies are available in the world and should be chosen as per the requirements. Mainly there are three types namely text, audio, and video. These should be utilized effectively for treatment.
Type of consultation: This is nothing but the first consultation and the follow-up consultation. RMP should have adequate knowledge about which type has to be followed.
Consent: Before the beginning of the consultation, it is important to receive consent from the patient. If the patient is agreeable to consultant ship then consent is implied. If RMP initiates treatment, then it’s called explicit consultation.
Patient evaluation: The patient should be evaluated properly with the best experience from the RMP.
Patient management: The patient shall be given health education before any telemedicine consultation. Their progress shall be reported.
When it comes to prescribing medicine to patients, there will be certain limits. The categories for prescribing the medicine are given in Table 1.
| List O | List A | List B |
|---|---|---|
|
|
|
Table 1: Consist of categories for prescribing the medicine [5]
Telemedicine in the USA
In the USA, the origin of telemedicine can go back to ancient hieroglyphs where the information about the pandemic was exchanged. During the 19th century, there saw an advancement in technologies as a result telephone and typewriter were used to communicate between the patients and health care workers. NASA played a vital role in the development of telemedicine in the modern days [8].
In the USA, Telemedicine is regulated by American Telemedicine Association. This ATA is responsible for developing the guidelines for the telemedicine in USA [9]. ATA considers Telemedicine in synchronization with telehealth [10]. The practitioner has to comply with federal and state laws. Few states in America have limitations for prescribing the controlled substances through telemedicine and few states allow telemedicine with certain restrictions [11].
The USA has upgraded itself as a result of many states medical boards are providing regulations to the practitioner as well as patients within the state. The main organizations which work on telemedicine are the Federation of state medical board and the American Telemedicine Association.
There is a system called cross-state licensing and it permits the RMP to provide the consultation and service in different states where he is not licensed. There is also a system called mutual recognition system by which the licensing authorities agree to legally accept the policies and processes of a licensee’s home state. Recently multiple state boards are working to harmonize the standards.
Online Prescribing for controlled substances and chronic pain and certain diseases are allowed and again it follows state laws where the practitioner is registered. The physician and patient relationship are very necessary for a good treatment; hence there is an instance where the start of telemedicine was done by in-person physical examination and assessment followed by distance consultation. Taking the patient consent before the counseling is very much essential in the USA and taking consent varies from state to state. The majority of states take consent through written format and in special condition use of audio-visual methods are allowed [11].
Conclusion
Telemedicine is a new advanced model of the healthcare system and in the coming years has a huge impact on the health care of the world. In India, telemedicine came into existence in the early 2000s, and in the USA it has gained popularity in the 19th century. The USA regulations are much forwarded and India had got its guidelines in recent times. The USA has a separate set of rules for each state and India follows a single guideline. The take-home point from this article may be there should exist harmonized and simple regulations for telemedicine and much research has to be made for the betterment of society in the coming years. We have seen a drastic grain in the use of telemedicine in the pandemic time and it has become a permanent part of the health care sector. We could see the use of telehealth medicine for the majority of treatment and Pharma industry and IT sector should join hands to make it a grand success by the advancement of technologies for people.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
References
- World Health Organization."Telemedicine: opportunities and developments in member states. Report on the second global survey on eHealth." World Health Organization, 2010.
- Chiron Health. "Advantages of telemedicine for patients." https://chironhealth.com/definitive-guide-to-telemedicine/telemedicine-info-patients/advantages-telemedicine-patients/
- Keystones Technologies. "4 types of telemedicine" https://keystonetechnologies.com/blog/4-types-of-telemedicine/
- Jnr, Bokolo Anthony. "Use of telemedicine and virtual care for remote treatment in response to COVID-19 pandemic."Journal of Medical Systems,Vol. 44, No. 7, 2020, pp. 1-9.
- Ministry of Health and Family Welfare. "Telemedicine Practice Guidelines." 2020. https://www.mohfw.gov.in/pdf/Telemedicine.pdf
- Weininger, Gabe, et al. "Association between cardiac surgeons’ number of years in practice and surgical outcomes in New York Cardiac centers."JAMA Network Open,Vol. 3, No. 11, 2020, p. e2023671.
- INC42 Plus, Datalabs. "Why telemedicine is the next big opportunity in Indian healthtech?" 2020. https://inc42.com/datalab/telemedicine-market-opportunity-in-indian-healthtech/
- Kichloo, Asim, et al. "Telemedicine, the current COVID-19 pandemic and the future: A narrative review and perspectives moving forward in the USA."Family Medicine and Community Health,Vol. 8, No. 3, 2020, p. e000530.
- Krupinski, Elizabeth A., and Jordana Bernard. "Standards and guidelines in telemedicine and telehealth."Healthcare, Vol. 2, No. 1, 2014, pp. 74-93.
- ATA. "Telehealth: Defining 21st century care." 2020. https://www.americantelemed.org/resource/why-telemedicine/
- Chiron Health. "Educate yourself on state telemedicine regulations." https://chironhealth.com/telemedicine/regulations/