Research - International Journal of Medical Research & Health Sciences ( 2022) Volume 11, Issue 11
Status of Telemedicine Use and Physician Satisfaction at Public Health Care Centers at King Abdulaziz Medical Center, Riyadh
Bander Ali Aldamkh*, Ali Abdulaziz A Alanzan, Ahmed Mohammed AlAbdulsalam and Muneera Abdullah BarajaBander Ali Aldamkh, Department of Family Medicine, King Abdullah International Medical Research Center/King Saud bin Abd, Kingdom of Saudi Arabia, Email: Aldamkh999@hotmail.com, aldamkhba@ngha.med.sa
Received: 27-Oct-2022, Manuscript No. ijmrhs-22-78442; Editor assigned: 31-Oct-2022, Pre QC No. ijmrhs-22-78442 (PQ); Reviewed: 01-Nov-2022, QC No. ijmrhs-22-78442 (Q); Revised: 04-Nov-2022, Manuscript No. ijmrhs-22-78442 (R); Published: 30-Nov-2022
Abstract
Objectives: To assess PHC physicians’ satisfaction with the use of telemedicine, and to assess the current status and use of telemedicine at national guard primary care clinics. Methods: This cross-sectional study included all primary healthcare physicians, with previous experience in telemedicine, working at primary healthcare centers at the National Guard Hospital, including the Health Care Specialty Center (HCSC), National Guard Comprehensive Specialized Clinic (NGCSC), King Abdulaziz city housing (Iskan Yarmouk), Prince Bader Housing Clinics (PBHC), Employee Health Centers (EHC), and King Saudi city housing (Dirab PHC) in early 2022. In addition, the study included all residents of the family medicine residency training program. Results: This study included 115 participants; more than half were less than 35 years old 72 (62.6%), and 70 (60.9%) were women. There were 22 (19.1%), 49 (42.6%), and 54 (47%) participants who had positive attitudes, and positive perceptions, and were satisfied, respectively. Conclusion: The responses from our study suggest that there is increased physician satisfaction with telemedicine. Young physicians were more satisfied than older physicians. There was a strong agreement that telemedicine could reduce unnecessary outpatient visits.
Keywords
Telemedicine, Primary care, Riyadh, Public health
Introduction
Telemedicine uses telecommunication technology and allows healthcare providers to monitor their patients in any area by exchanging health data across social, temporal, geographical, and cultural barriers. It could alleviate the imminent gap in the accessibility of healthcare services, and it is considered a chance to improve the flexibility of the healthcare service using video conferences, smartphones, and emails [1-5]. Telemedicine provides cost-effective, accessible, and advanced healthcare services in remote areas, making it a new channel for healthcare services [6]. In 1879, the earliest evidence of telemedicine was published, describing the diagnosis of a child via phone, while the modern form started in the 1960s in the military sector [6,7]. The modern form of telemedicine appears with Internet maturation, which facilitates the use of videoconferences, distance learning, and the transfer of high-quality data at low costs [6]. The American Medical Association predicts that “after COVID-19, $250 billion in care could shift to telehealth, boosting research and infrastructural development” [6,7]. Additionally, 76% of hospitals during the COVID-19 pandemic were connected to patients using telemedicine [6]. Most healthcare providers have become frequent users of telemedicine such as radiology, psychiatry, and cardiology (39.5%, 27.8%, and 24.1%, respectively) [6].
The dramatic expansion of telemedicine in recent decades, especially after COVID-19, needs to measure how physicians feel and their satisfaction with telemedicine has become increasingly important [8,9]. Physician satisfaction is a crucial issue in telemedicine’s success [10]. In addition, doctors’ satisfaction is important to evaluate, as it contributes greatly to the effectiveness and efficiency of any kind of consultation and management plan. A previous survey-based study showed that 87% of physicians were satisfied with the current telemedicine services [11]. In contrast, patient satisfaction was reported more frequently. During the COVID-19 pandemic, a study reported that more than 86% of patients were satisfied with the telemedicine experience [12]. In Saudi Arabia, the Ministry of Health (MOH) has recently created several health applications like “seha, tetamman, tawakklna, tabaud, mawid” which markedly increase the use of telemedicine [13,14]. Another public study showed that 51% of telemedicine users in Saudi Arabia were satisfied with the new technology [15]. It has been reported that perceived ease of use and usefulness of telemedicine are the most common factors affecting behavioral intention that results in actual telemedicine utilization and satisfaction [14,16,17. However, physician satisfaction was affected by their background experiences with telemedicine and their expectations. In addition, providing frequent education, support programs, symposiums, and training can improve telemedicine adoption and satisfaction [18,19]. Using mobile applications has helped healthcare providers monitor the progression of chronic disease and decrease non-essential visits during the coronavirus pandemic [20-23]. Most healthcare providers can use telemedicine mobile applications to detect COVID-19 by assessing their symptoms [24]. A cross-sectional study in Saudi Arabia reported that 86% of the participants knew the benefits of using telemedicine mobile applications (e.g., Seha and Mawid), and they used them to book appointments [20]. It can also decrease transportation costs by decreasing patient transfer to and from hospitals/clinics, which in turn effectively impacts the productivity and efficiency of the healthcare process and quality of life [2]. Stenlund and Mines indicated that videoconferencing allows healthcare providers to overcome some issues, such as geographic barriers, reduced stress, weather concerns, helped patients to have access to healthcare providers, education, and reduced travel time. Another study reported that video conferencing can be beneficial for oncology consultations, education for healthcare providers or clients, nursing visits, home hospices, and team meetings [25,26]. In contrast, telemedicine can cause a breakdown in the relationship between healthcare providers and patients and a breakdown in the relationship between healthcare workers and bureaucratic and organizational difficulties [27]. Watanabe et al. reported that most rural family healthcare providers were not aware of the virtual clinic, and most elderly patients with chronic diseases failed to read telehealth monitoring equipment [28,29]. In Saudi Arabia, the MOH conducted a study on the adoption of telemedicine and its role in alleviating some healthcare system challenges in Saudi Arabia. The first national project for telemedicine was launched in 2011 under the Saudi Telemedicine Network (STN), which covers all Healthcare Facilities (HCF) [15]. Additionally, the Saudi MOH collaborated with the Canada Health Infoway and Ontario Telemedicine Network to introduce guidance regarding a telemedicine roadmap and the STN roadmap development, which was issued in 2013 [15]. Recently, it has provided more advanced features to the current telehealth services to cope with the COVID-19 pandemic, which provided healthcare services using mobile applications (e.g., Seha, Mawid, Tawakklna, Tabaud, and Tetamman) [30]. Although telemedicine has been introduced in Saudi Arabia since 1993, few studies have been conducted on its benefits, advantages, and disadvantages in the Saudi Arabian healthcare system [5].
Aim of the Study
To assess the current status of telemedicine in primary healthcare centers at NGHA and the degree of satisfaction among healthcare providers.
Objectives
• To assess PHC physicians’ satisfaction with the use of telemedicine.
• To assess the current status and use of telemedicine at national guard primary care clinics.
• To assess the association between physicians’ demographic data and their satisfaction with telemedicine
Methods
This cross-sectional study included all primary healthcare physicians, with previous experience in telemedicine, working at primary healthcare centers at the National Guard Hospital, including the Health Care Specialty Center (HCSC), National Guard Comprehensive Specialized Clinic (NGCSC), King Abdulaziz city housing (Iskan Yarmouk), Prince Bader Housing Clinics (PBHC), Employee Health Centers (EHC), and King Saudi city housing (Dirab PHC) in early 2022. In addition, the study included all residents of the family medicine residency training program. This study was approved by the King Abdulla International Medical Research Center. The study was conducted using a self-administered questionnaire that was sent electronically to the participants. The questionnaire included 31 questions, which were divided into four sections: the first section included seven questions about demographics; the second section involved 12 questions that assessed the current status of telemedicine at PHC; the third section involved nine questions that assessed the perception of physicians on the advantages and disadvantages of telemedicine, and the fourth section involved questions about the satisfaction of physicians.
The questionnaire was developed by the authors after a comprehensive literature search and content validation were performed by three family medicine consultants. The questionnaire was pre-tested on ten subjects from our target population to ensure the clarity and accuracy of the tool. The Cronbach’s alpha for the questionnaire was 0.81.
Inclusion Criteria
all primary Healthcare physicians, who are working at the primary healthcare center at National guard hospital, Saudi Arabia, who had previous experience in using telemedicine, and all residents in the family medicine residency training program.
Exclusion Criteria
Those who did not use telemedicine.
Data Analysis
Data collected from the retrieved questionnaires were analyzed using IBM SPSS version 22. The categorical variables are represented using frequency and percentages whereas numerical variables are represented using mean and standard deviation. The chi-square test was used to compare proportions and P-value was considered significant when lower than 0.05.
Results
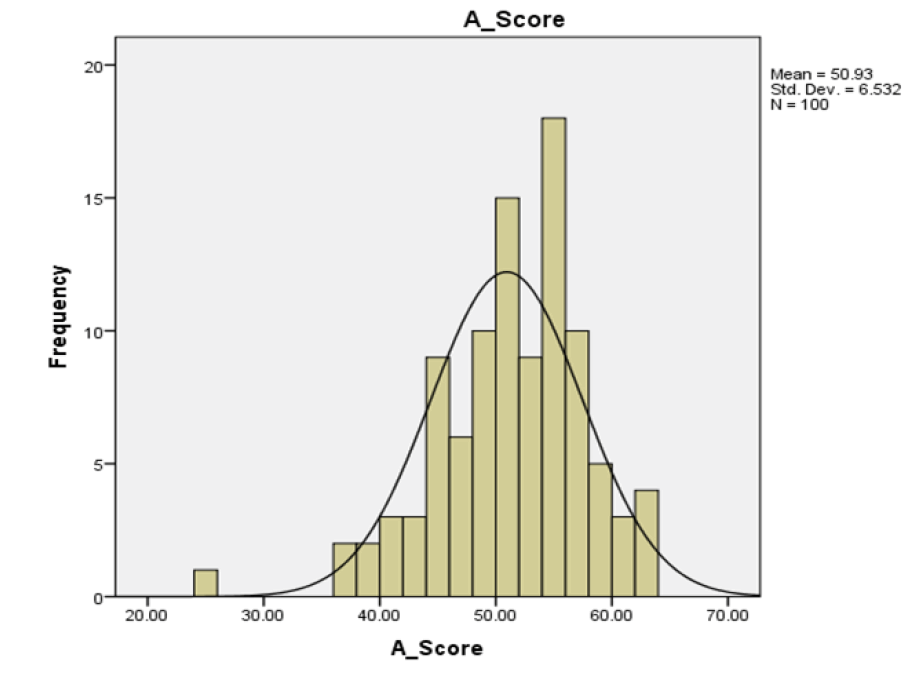
This study included 115 participants; 72 (62.6%) were less than 35 years old and 70 (60.9%) were women. Almost half of the physicians were residents 59 (51.3%), and only 26 (22.6%) had more than 15 years of experience. Less than half of the 55 (47.8%) participants reported rotating between centers; the demographics of the participants are shown in Table 1. The status of telemedicine is shown in Table 2. A few proportions reported receiving training courses for telemedicine consultation 16 (13.9%), and the largest proportions reported sessions number of 5-10 sessions 43 (37.4%), and duration of 5 minutes to 10 minutes 61 (53%). There 65 (65.5%), and 53 (46.1%) reported space and equipment, respectively. The mean scores for attitude and satisfaction are shown in Table 3. The mean ± SD of attitude among participants was 50.9 ± 6.5, whereas the mean ± SD of satisfaction was 25.7 ± 6.25. The attitudes, perceptions, and satisfaction levels of the participants are shown in Table 4 (Figure 1). There were 22 (19.1%), 49 (42.6%), and 54 (47%) participants who had positive attitudes, and positive perceptions, and were satisfied, respectively.
| Variables | N (%) |
|---|---|
|
Age |
|
| 25-34 | 72(62.6%) |
| ≥ 35 | 43(37.4%) |
|
Gender |
|
| Female | 70(60.9%) |
| Male | 45(39.1%) |
|
Profession |
|
| Consultant | 38(33%) |
| Resident | 59(51.3%) |
| Staff Physician | 18(15.7%) |
|
Experience |
|
| 0-5 years | 67(58.3%) |
| >5 years to 15 years | 22(19.1%) |
| >15 years | 26(22.6%) |
|
Centers |
|
| Rotating between centers | 55(47.8%) |
| Not rotating | 60(52.2%) |
| Variables | N (%) |
|---|---|
|
Receiving training course for telemedicine consultation |
|
| Yes | 16(13.9%) |
| No | 99(86.1%) |
|
Sessions |
|
| Less than 5 sessions | 26(22.6%) |
| 5 sessions to10 sessions | 43(37.4%) |
| >10 sessions | 33(28.7%) |
| Missing | 13(11.3%) |
|
Time |
|
| Less than 5 minutes | 22(19.1%) |
| 5 minutes to10 minutes | 61(53%) |
| >10minutes | 19(16.5%) |
| Missing | 13(11.3%) |
|
Space |
|
| Yes | 65(56.5%) |
| No | 37(32.2%) |
| Missing | 13(11.3%) |
|
Equipment |
|
| Yes | 53(46.1%) |
| No | 49(42.6%) |
| Missing | 13(11.3%) |
| Variables | Mean ± SD (Range) |
| Attitude | 50.9 ± 6.5 (25-63) |
| Satisfaction | 25.7 ± 6.25(7-35) |
| Variables | N (%) |
|---|---|
| Attitude toward telemedicine | |
| Negative | 26(22.6%) |
| Neutral | 52(45.2%) |
| Positive | 22(19.1%) |
| Missing | 15(13%) |
| Perception on telemedicine | |
| Negative | 1(0.9%) |
| Neutral | 50(43.5%) |
| Positive | 49(42.6%) |
| Missing | 15(13%) |
| Satisfaction | |
| Not satisfied | 8(7%) |
| Neutral | 38(33%) |
| Satisfied | 54(47%) |
| Missing | 15(13%) |
The correlations between attitude, perception, and satisfaction with the demographics of the participants and telemedicine status are shown in Tables 5-7. Regarding attitude, there were significant correlations between attitude and profession (p=0.047), the status of receiving a telemedicine training course (p=0.025), and space (p=0.01) (Table 5). None of the factors showed a significant association with perception (Table 6). Significant associations were found between satisfaction and space (p=0.001) and equipment (p=0.0001) (Table 7).
| Variables | Attitude | p-value | ||
|---|---|---|---|---|
| Negative | Neutral | Positive | ||
| Age | 0.5 | |||
| 25-34 | 15(23.1%) | 34(52.3%) | 16(24.6%) | |
| ≥ 35 | 11(31.4%) | 18(51.4%) | 17.1(%) | |
| Gender | 0.5 | |||
| Female | 18(29.5%) | 31(50.8%) | 12(19.7%) | |
| Male | 8(20.5%) | 21(53.8%) | 10(25.6%) | |
| Profession | 0.047* | |||
| Consultant | 6(20%) | 21(70%) | 3(10%) | |
| Resident | 13(23.6%) | 27(49.1%) | 15(27.3%) | |
| Staff Physician | 7(46.7%) | 4(26.7%) | 4(26.7%) | |
| Experience | 0.5 | |||
| 0-5 years | 15(24.2%) | 31(50%) | 16(25.8%) | |
| >years to15 years | 7(36.8%) | 9(47.4%) | 3(15.8%) | |
| >15 years | 4(21.1%) | 12(63.2%) | 3(15.8%) | |
| Centers | 0.056 | |||
| Rotating between centers | 14(26.9%) | 22(42.3%) | 16(30.8%) | |
| Not rotating | 12(25%) | 30(62.5%) | 6(12.5%) | |
| Receiving training course for telemedicine consultation | 0.025* | |||
| Yes | 1(7.1%) | 12(85.7%) | 1(7.1%) | |
| No | 25(29.1%) | 40(46.5%) | 21(24.4%) | |
| Sessions | 0.5 | |||
| Less than 5 sessions | 8(30.8%) | 13(50%) | 5(19.2%) | |
| 5 sessions to10 sessions | 11(26.2%) | 19(45.2%) | 12(28.6%) | |
| >10 sessions | 7(21.9%) | 20(62.5%) | 5(15.6%) | |
| Time | 0.5 | |||
| Less than 5 minutes | 4(18.2%) | 11(50%) | 7(31.8%) | |
| 5 minutes to10 minutes | 15(25.4%) | 32(54.2%) | 12(20.3%) | |
| >10minutes | 7(36.8%) | 9(47.4%) | 3(15.8%) | |
| Space | 0.01* | |||
| Yes | 11(16.9%) | 38(58.5%) | 16(24.6%) | |
| No | 15(42.9%) | 14(40%) | 6(17.1%) | |
| Equipment | 0.3 | |||
| Yes | 11(20.8%) | 28(52.8%) | 14(26.4%) | |
| No | 15(31.9%) | 24(51.1%) | 8(17%) | |
| p-value*; significant | ||||
| Variables | Perception | p-value | ||
|---|---|---|---|---|
| Negative | Neutral | Positive | ||
| Age | 0.2 | |||
| 25-34 | 0(0%) | 31(47.7%) | 34(52.3%) | |
| ≥ 35 | 1(2.9%) | 19(54.3%) | 15(42.9%) | |
| Gender | 0.2 | |||
| Female | 1(1.6%) | 34(55.7%) | 26(42.6%) | |
| Male | 0(0%) | 16(41%) | 23(59%) | |
| Profession | 0.2 | |||
| Consultant | 1(3.3%) | 16(53.3%) | 13(43.3%) | |
| Resident | 0(0%) | 24(43.6%) | 31(56.4%) | |
| Staff Physician | 0(0%) | 10(66.7%) | 5(33.3%) | |
| Experience | 0.2 | |||
| 0-5 years | 0(0%) | 29(46.8%) | 33(53.2%) | |
| >years to 15 years | 0(0%) | 11(57.9%) | 8(42.1%) | |
| >15 years | 1(5.3%) | 10(52.6%) | 8(42.1%) | |
| Centers | 0.2 | |||
| Rotating between centers | 0(0%) | 23(44.2%) | 29(55.8%) | |
| Not rotating | 1(2.1%) | 27(56.3%) | 20(41.7%) | |
| Receiving training course for telemedicine consultation | 0.4 | |||
| Yes | 0(0%) | 5(35.7%) | 9(64.3%) | |
| No | 1(1.2%) | 45(52.3%) | 40(46.5%) | |
| Sessions | 0.4 | |||
| Less than 5 sessions | 0(0%) | 15(57.7%) | 11(42.3%) | |
| 5 sessions to 10 sessions | 0(0%) | 18(42.9%) | 24(57.1%) | |
| >10 sessions | 1(3.1%) | 17(53.1%) | 14(43.8%) | |
| Time | 0.6 | |||
| Less than 5 minutes | 0(0%) | 10(45.5%) | 12(54.5%) | |
| 5 minutes to 10 minutes | 1(1.7%) | 28(47.5%) | 30(50.8%) | |
| >10minutes | 0(0%) | 12(63.2%) | 7(36.8%) | |
| Space | 0.2 | |||
| Yes | 0(0%) | 31(47.7%) | 34(52.3%) | |
| No | 1(2.9%) | 19(54.3%) | 15(42.9%) | |
| Equipment | 0.3 | |||
| Yes | 0(0%) | 24(45.3%) | 29(54.7%) | |
| No | 1(2.1%) | 26(55.3%) | 20(42.6%) | |
| Variables | Satisfaction | p-value | ||
|---|---|---|---|---|
| Not satisfied | Neutral | Satisfied | ||
|
Age |
0.6 | |||
| 25-34 | 4(6.1%) | 26(39.4%) | 36(54.5%) | |
| ≥ 35 | 4(11.8%) | 12(35.5%) | 18(52.9%) | |
|
Gender |
0.6 | |||
| Female | 4(6.7%) | 25(41.7%) | 31(51.7%) | |
| Male | 4(10%) | 13(32.5%) | 23(57.5%) | |
|
Profession |
0.2 | |||
| Consultant | 5(16.7%) | 10(33.3%) | 15(50%) | |
| Resident | 2(3.6%) | 24(42.9%) | 30(53.6%) | |
| Staff Physician | 1(7.1%) | 4(28.6%) | 9(64.3%) | |
|
Experience |
0.5 | |||
| 0-5 years | 4(6.3%) | 24(38.1%) | 35(55.6%) | |
| >5 years to 15 years | 1(5.3%) | 9(47.4%) | 9(47.4%) | |
| >15 years | 3(16.7%) | 5(27.8%) | 10(55.6%) | |
|
Centers |
0.2 | |||
| Rotating between centers | 2(3.8%) | 21(39.6%) | 30(56.6%) | |
| Not rotating | 6(12.8%) | 17(36.2%) | 24(51.1%) | |
|
Receiving training course for telemedicine consultation |
0.9 | |||
| Yes | 1(7.1%) | 5(35.7%) | 8(57.1%) | |
| No | 7(8.1%) | 33(38.4%) | 46(53.5%) | |
|
Sessions |
0.08 | |||
| Less than 5 sessions | 3(12%) | 11(44%) | 11(44%) | |
| 5 sessions to 10 sessions | 0(0%) | 18(41.9%) | 25(58.1%) | |
| >10 sessions | 5(15.6%) | 9(28.1%) | 18(56.3%) | |
|
Time |
0.5 | |||
| Less than 5 minutes | 0(0%) | 9(40.9%) | 13(59.1%) | |
| 5 minutes to10 minutes | 6(10.2%) | 23(39%) | 30(50.8%) | |
| >10minutes | 2(10.5%) | 6(31.6%) | 11(57.9%) | |
|
Space |
0.001* | |||
| Yes | 2(3.1%) | 20(30.8%) | 43(66.2%) | |
| No | 6(17.1%) | 18(51.4%) | 11(31.4%) | |
|
Equipment |
0.0001* | |||
| Yes | 1(1.9%) | 11(20.8%) | 41(77.4%) | |
| No | 7(14.9%) | 27(57.4%) | 13(27.7%) | |
|
p-value*; significant |
||||
Discussion
The use of telemedicine consultations has increased worldwide and in Saudi Arabia in recent years. It has become one of the pillars of the world’s health systems since COVID-19. Our study, conducted later in the pandemic, provided an excellent opportunity to assess the status of TM and satisfaction in primary healthcare systems in Saudi Arabia.
Most physicians in our study did not receive training courses for TM consultation. Lack of suitable training is considered a major barrier to the use in Saudi Arabia, as mentioned in previous studies [1,31]. However, our participants believed that continuous training is necessary for the proper use of telemedicine. Currently, there are many official training programs in the US for telehealth education that focus physicians, nurses, administrators, IT teams, and policymakers on engaging and interactive content [32].
Internationally, in Italy, the duration of teleconsultation depends on the type of consultation. The least duration was cardiac consultation, while dermatological and diabetic consultations required more time, but the usual time was between 5 minutes to 10 minutes. Similar results have been reported in 53% of the population have similar results [33].
Moreover, previous studies have recommended that telemedicine can be a good option if the proper place for teleconsultation is available; unavailability of spaces and equipment was a major obstacle [1,31]. However, in our study, most physicians reported that available places and equipment at primary care centers at NGHA had high standards for quality of care.
Many local and international studies have reported high satisfaction with telemedicine. Although physician satisfaction with telemedicine was an important consideration in our study, 54% of our physicians had a high satisfaction rate with telemedicine, which is consistent with previous studies [34-36]. In our study, satisfaction rates were found in clinics with available space and equipment.
Most previous studies have shown a positive attitude toward telemedicine [37,38]. However, in our study, despite a high satisfaction rate, physicians’ attitudes toward teleconsultation were neutral. The position of most participants, years of experience, and recent application of telemedicine consultation, especially during the COVID-19 pandemic, are likely to lead to a more negative attitude toward telemedicine and a decrease in the use of telemedicine. In addition, the unavailability of a training course for TM and technical issues that occur during consultations could be a factor. We found that the attitude toward using TM was negatively correlated with staff physicians, possibly due to limited experience.
The results of our study are limited to primary care centers in the National Guard and cannot be generalized due to primary health care settings, availability of telemedicine equipment, and facilities that vary compared to other primary health care centers in the Kingdom. Besides the limitations of the online survey, we did not combine the questionnaire with focus-group discussions/structured interviews, which could have improved the quality of the data. Patient feedback was not included in the study design, which would have probably had a greater impact on the study. policies and regulations of the National Guard in using telemedicine may have affected the results of our study and the attitudes of physicians.
Further studies should be conducted regarding TM use in PHC settings other than during the pandemic to compare different attitudes and styles of using TM. Furthermore, telemedicine training courses should be applied to all medical fields, starting from medical schools, residency training programs, and hospital courses, to reduce misuse and problems related to medical and technical issues. Consultation between information technology experts and clinicians can improve TM. Government regulation to improve technology-related issues and make telemedicine cost-effective will also help increase adoption. However, intense monitoring and evaluation of telemedicine programs are essential to maintain quality.
Conclusion
In conclusion, most participants did not receive a training course or education on telehealth. Lack of education and training was perceived as a barrier to the practice of telemedicine by most respondents. More than one-third of the participants were concerned about the lack of space and equipment. The responses from our study suggest that there is increased physician satisfaction with telemedicine. Young physicians were more satisfied than older physicians. While attitudes toward telemedicine were generally neutral, negative attitudes were observed more frequently by staff physicians. There was a strong agreement that telemedicine could reduce unnecessary outpatient visits.
Declarations
Conflict of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Albarrak, Ahmed I., et al. "Assessment of physician’s knowledge, perception and willingness of telemedicine in Riyadh region, Saudi Arabia." Journal of infection and public health, Vol. 14, No. 1, 2021, pp. 97-02.
Google Scholar Crossref - AlSanad, Abeer, and Nessrine Zemirli. "A guideline for using knowledge management in telemedicine systems dedicated for diabetes patients in Saudi Arabia." New Contributions in Information Systems and Technologies. Springer, Cham, 2015, pp. 193-01.
Google Scholar Crossref - Nessa, Ahasanun, et al. "Applicability of telemedicine in Bangladesh: current status and future prospects." 2008 Third International Conference on Convergence and Hybrid Information Technology, Vol. 1, 2008.
Google Scholar Crossref - TeleHealth Programs. "Health Resources and Service Administration." 2021, Health Resources and Services Administration, 2021.
- El-Mahalli, Azza A., Sahar H. El-Khafif, and Mona F. Al-Qahtani. "Successes and challenges in the implementation and application of telemedicine in the eastern province of Saudi Arabia." Perspectives in health information management/AHIMA, American Health Information Management Association, Vol. 9, 2012, 1-27.
Google Scholar - Waqas, Ahmed, et al. "Harnessing telemedicine for the provision of health care: bibliometric and scientometric analysis." Journal of medical Internet research, Vol. 22, No. 10, 2020.
Google Scholar Crossref - Tanya Albert H. "After COVID-19, $250 billion in care could shift to telehealth." American Medical Association Digital, 2020.
Google Scholar - Monnier, Jeannine, Rebecca G. Knapp, and B. Christopher Frueh. "Recent advances in telepsychiatry: an updated review." Psychiatric Services, Vol. 54, No. 12, 2003, pp. 1604-09.
Google Scholar Crossref - Williams, Tracy L., Carl R. May, and Aneez Esmail. "Limitations of patient satisfaction studies in telehealthcare: a systematic review of the literature." Telemedicine Journal and e-health, Vol. 7, No. 4, 2001, pp. 293-16.
Google Scholar Crossref - Jalabneh, Rawan, et al. "Use of mobile phone apps for contact tracing to control the COVID-19 pandemic: A literature review." Applications of Artificial Intelligence in COVID-19, 2021, pp. 389-04.
Google Scholar - Gilbert, Anthony W., et al. "Rapid implementation of virtual clinics due to COVID-19: report and early evaluation of a quality improvement initiative." BMJ open quality, Vol. 9, No. 2, 2020. p. e000985.
Google Scholar Crossref - Park, Hyung-Youl, et al. "Satisfaction survey of patients and medical staff for telephone-based telemedicine during hospital closing due to COVID-19 transmission." Telemedicine and e-Health, Vol. 27, No. 7, 2021, pp. 724-32.
Google Scholar Crossref - Muzafar, Saira, and N. Z. Jhanjhi. "Success stories of ICT implementation in Saudi Arabia." Employing Recent Technologies for Improved Digital Governance. IGI Global, 2020, pp. 151-63.
Google Scholar - Davis, Fred D. "A technology acceptance model for empirically testing new end-user information systems: Theory and results." Diss. Massachusetts Institute of Technology, 1985.
Google Scholar - Alshammari, Fares. "Perceptions, preferences and experiences of telemedicine among users of information and communication technology in Saudi Arabia." Journal of Health Informatics in Developing Countries, Vol. 13, No. 1, 2019.
Google Scholar Crossref - Davis, Fred D. "Perceived usefulness, perceived ease of use, and user acceptance of information technology." Management Information Systems Quarterly, 1989, pp. 319-40.
Google Scholar Crossref - Wilson, Vance E., and Nancy K. Lankton. "Modeling patients' acceptance of provider-delivered e-health." Journal of the American Medical Informatics Association, Vol. 11, No. 4, 2004, pp. 241-48.
Google Scholar Crossref - Yi, Youjae. "A critical review of consumer satisfaction." Review of marketing, Vol. 4, No. 1, 1990, pp. 68-23.
Google Scholar - Khalifa, Mohamed, and Vanessa Liu. "Satisfaction with internet-based services: the role of expectations and desires." International Journal of Electronic Commerce, Vol. 7, No. 2, 2002, pp. 31-49.
Google Scholar Crossref - Nguyen, Mary, et al. "A review of patient and provider satisfaction with telemedicine." Current allergy and asthma reports, Vol. 20, No. 11, 2020, pp. 1-7.
Google Scholar Crossref - Alqahtani, Jaber S., et al. "Prevalence, severity and mortality associated with COPD and smoking in patients with COVID-19: a rapid systematic review and meta-analysis." PloS one, Vol. 15, No. 5, 2020.
Google Scholar Crossref - Bai, Yan, et al. "Presumed asymptomatic carrier transmission of COVID-19." Jama, Vol. 323, No. 14, 2020, pp. 1406-07.
Google Scholar Crossref - Alumran, Arwa. "Role of precautionary measures in containing the natural course of novel coronavirus disease." Journal of Multidisciplinary Healthcare, Vol. 13, 2020, p. 615.
Google Scholar Crossref - Alakhrass, Hossam, et al. "Ministry of Health Saudi Arabia: COVID-19 website benefits and validity and reliability of the data." Health, Vol. 13, No. 1, 2021, pp. 40-46.
Google Scholar Crossref - Stenlund, Diana. "Videoconferencing and dietitian services: In rural Ontario communities." Canadian Journal of Dietetic Practice and Research, Vol. 73, No. 4, 2012, pp. 176-80.
Google Scholar Crossref - Carr-Hill, Roy A. "The measurement of patient satisfaction." Journal of public health, Vol. 14, No. 3, 1992, pp. 236-49.
Google Scholar Crossref - Hjelm, N. M. "Benefits and drawbacks of telemedicine." Journal of telemedicine and telecare, Vol. 11, No. 2, 2005, pp. 60-70.
Google Scholar Crossref - Watanabe, Sharon M., et al. "Improving access to specialist multidisciplinary palliative care consultation for rural cancer patients by videoconferencing: report of a pilot project." Supportive Care in Cancer, Vol. 21, No. 4, 2013, pp. 1201-07.
Google Scholar Crossref - Wade, Rachael, Kelly Shaw, and Colleen Cartwright. "Factors affecting provision of successful monitoring in home telehealth." Gerontology, Vol. 58, No. 4, 2012, pp. 371-77.
Google Scholar Crossref - Alghamdi, Saeed M., Jaber S. Alqahtani, and Abdulelah M. Aldhahir. "Current status of telehealth in Saudi Arabia during COVID-19." Journal of family & community medicine, Vol. 27, No. 3, 2020, pp. 208-11.
Google Scholar Crossref - Falgarone, Géraldine, et al. "A Teleconsultation Device, Consult Station, for Remote Primary Care: Multisite Prospective Cohort Study." Journal of medical Internet research, Vol. 24, No. 5, 2022.
Google Scholar Crossref - Uvahealth. "Telehealth Education & Training." UVA Health, 2022.
- Zanaboni, Paolo, et al. "Teleconsultation service to improve healthcare in rural areas: acceptance, organizational impact and appropriateness." BMC Health Services Research, Vol. 9, No. 1, 2009, pp. 1-9.
Google Scholar Crossref - Altulaihi, Bader A., et al. "Physician’s perception toward using telemedicine during COVID-19 pandemic in King Abdulaziz Medical City, Riyadh, Saudi Arabia." Cureus, Vol. 13, No. 7, 2021.
Google Scholar Crossref - Malouff, Timothy D., et al. "Physician satisfaction with telemedicine during the COVID-19 pandemic: the Mayo Clinic Florida experience." Mayo Clinic Proceedings: Innovations, Quality & Outcomes, Vol. 5, No. 4, 2021, pp. 771-82.
Google Scholar Crossref - Acharya, Rajesh V., and Jasuma J. Rai. "Evaluation of patient and doctor perception toward the use of telemedicine in Apollo Tele Health Services, India." Journal of family medicine and primary care, Vol. 5, No. 4, 2016, p. 798.
Google Scholar Crossref - Hu, Paul J., et al. "Examining the technology acceptance model using physician acceptance of telemedicine technology." Journal of management information systems, Vol. 16, No. 2, 1999, pp. 91-12.
Google Scholar Crossref - Shadangi, Preeti Y., et al. "Physician’s Attitude Towards Acceptance of Telemedicine Technology for Delivering Health Care Services." International Journal of Mechanical Engineering and Technology, Vol. 9, No. 11, 2018, pp. 715-22.
Google Scholar