Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 6
Single and Two-Level Anterior Cervical Discectomy and Fusion (ACDF) with Stand-Alone Cage-Plate: Single Centre Experience
Waleed Mohammad Awwad, Rohail Mumtaz*, Sarah Nasser AlJasser, Mana Adel AlMuhaideb, Waleed Albishi, Abdulaziz Almaawi and Khalid AM AlsalehRohail Mumtaz, Orthopedic Surgery Department, King Saud University, Riyadh, Saudi Arabia, Email: dr.rohael@gmail.com
Received: 19-May-2021 Accepted Date: Jun 23, 2021 ; Published: 30-Jun-2021
Abstract
Introduction: After almost a decade of employing the concept of intervertebral disc removal complemented by vertebral fusion as a therapeutic technique for herniated cervical discs, Anterior Cervical Discectomy and Fusion (ACDF) became the standard gold treatment of a spectrum of cervical diseases such as compressive myelopathy/ radiculopathy, disc herniation, and trauma. There is no discrepancy regarding the technique of ACDF in terms of using a standalone cage with an integrated spacer system or plating. This study reports 20 cases that underwent ACDF with standalone cage-plate and their radiological outcomes. Methods: A total of 20 patients who underwent single or twolevel ACDF with standalone cage-plate for radiculopathy or myelopathy between May 2017 and February 2019 at a tertiary University Hospital have retrospectively reported in this study. The patient’s demographics and radiological outcomes, including disc height, segmental lordotic angle, and global lordotic angle, were reported for each case preoperatively, immediately postoperatively, and at 12-month follow-up. As per protocol, all patients were on Calcium and Vitamin D for nine months after the procedure. Results: All cases had an excellent fusion rate at 12 months of follow-up. None of the cases we reported has faced subsidence. According to Odom’s criteria, the surgical outcome has been reported as excellent for all patients at 12 months of follow-up. Conclusion: ACDF with a standalone cageplate system has shown excellent fusion, clinical and radiological outcomes with no subsidence and pseudoarthrosis in short term.
Keywords
Anterior Cervical Discectomy and Fusion (ACDF), Myelopathy, Radiculopathy, Standalone cage plate
Abbreviations
ACDF: Anterior Cervical Discectomy and Fusion, PEEK: Poly Ether Ether Ketone, IRB: Institutional Review Board, KSU: King Saud University, SPSS: Statistical Package for the Social Science, GLA: Global Lordotic Angle, SLA: Segmental Lordotic Angle, RLNP: Recurrent Laryngeal Nerve Palsy
Introduction
Adverse drug reaction can be defined as, “An appreciably harmful or unpleasant reaction, resulting from an intervention After almost a decade of employing the concept of intervertebral disc removal complemented by vertebral fusion as a therapeutic technique for herniated cervical discs, Anterior Cervical Discectomy and Fusion (ACDF) became the gold standard treatment of a spectrum of cervical diseases such as compressive myelopathy/radiculopathy, disc herniation, and trauma. They were initially innovated in the 1950s by Smith and Robinson [1]. There has been a consensus in the literature regarding the technique of ACDF in terms of using a standalone cage with an integrated spacer system or plating [2].
There have been multiple types of cages and systems reported in the literature for the ACDF technique with its pros and cons. Those various systems vary from metal, plastic, and ceramic cages. Even though the lack of data supporting the choice of cage materials, plastic cages made from Polyetheretherketone (PEEK) have become a popular method for stabilizing the disc space after ACDF [3].
Recently there has been an increase in the usage of standalone Polyetheretherketone (PEEK) cages [4]. It is due to its low modulus of elasticity which closely resembles bone. Furthermore, they are radiolucent and help to observe the fusion across the instrumented level more accurately. Jun Cho, et al. reported no clinical outcome differences between those operated with standalone PEEK cages and zero profile devices [3].
There are many conflicts in the literature regarding single and multilevel ACDF with plating and without plating. Although, most of the authors report no differences in the clinical outcomes between the two procedures [5,6]. While, some were concerned that ACDF with standalone cage was associated with subsidence, pseudoarthrosis, and misalignment specifically [5,7,8]. Other studies have shown that cage-assisted ACDF without plating was associated with a lower complication rate and shorter hospital stay [9,10].
Our study aims to report the effectiveness of ACDF with standalone cage-plate, their radiological and clinical outcomes in terms of improved disc height, global lordotic angle, and segmental lordotic angle.
Materials and Methods
Study Duration
The study duration is two years and it is conducted from May 2017 till May 2019.
Study Method
It’s a retrospective study.
Study Sample (N)
Twenty patients were included who fulfilled the inclusion criteria.
Study Settings
The study is being conducted at King Saud University, Orthopedic surgery department.
Inclusion Criteria
Our inclusion criteria were cervical disc degeneration along with radiculopathy or myelopathy or a combination of both, and all of them must have undergone ACDF with a standalone cage plate system.
Exclusion Criteria
We excluded all those operated on for other cervical diseases such as infection, trauma, tumor, or deformity.
Institutional Review Board (IRB) Approval
The Institutional Review Board (IRB) approved the study at King Khalid University Hospital, King Saud University, Saudi Arabia, with the IRB number KSU-IRB 017E.
We reviewed retrospectively thirty-nine patients who underwent cervical spine surgery during May 2017 and May 2019 and included them in the study. Twenty patients met the criteria for our research, which was single or double-level ACDF with standalone cage-plate.
All involved patients were treated and followed up at King Khalid University Hospital. The data concerning each patient included age, gender, smoking status, the indication of surgery, levels involved, intra-operative time, estimated blood loss, length of hospital stay, and radiological outcomes including disc height, global lordotic angle, and segmental lordotic angle on standing lateral X-ray pre-operatively, immediate postoperatively, and at 12 months follow up. As per protocol, all patients were on Calcium and Vitamin D for nine months after the procedure. The flexion and extension imaging was performed at the final follow-up.
Disc height was measured by the length between the midpoints of two adjacent vertebrae; global and segmental lordotic angle was measured by the Cobb method [11]. Before treatment, any patient who initially had kyphosis had recorded global and lordotic angles with negative (-). Screw loosening was marked as a radiolucent line surrounding the implant >1 mm in width known as a halo sign [12]. Fusion was applied as a standard definition by observing bridging bone between adjacent vertebral endplates of the involved segments [13-18].
Surgical Technique
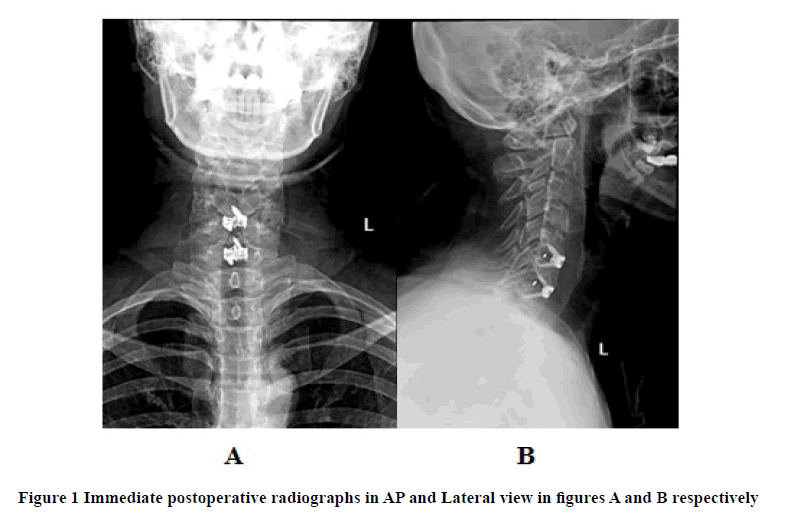
All surgeries were performed under general anesthesia. All the surgeries were performed through a left-sided skin incision in line with a skin crease at the desired level. After identification of the carotid pulsation, blunt dissection was performed to approach the prevertebral fascia. After the prevertebral facia's penetration, the appropriate level was confirmed under the image intensifier, followed by subperiosteal elevation of longus colli muscles and standard discectomy. After preparing the endplates, the suitable size cage is selected using a trail cage, and then the final cage was inserted and secured. Before closure, hemostasis was secured. No drains were used for any patient. The wound was thoroughly irrigated with 0.9% normal saline. Wound closure was performed with vicryl and monocryl. Finally, the antiseptic dressing was applied. Postoperatively all the patients were given rigid cervical collars until six weeks. For all the patients, there were not any intraoperative complications. Postoperative cervical spine X-rays were done (Figure 1).
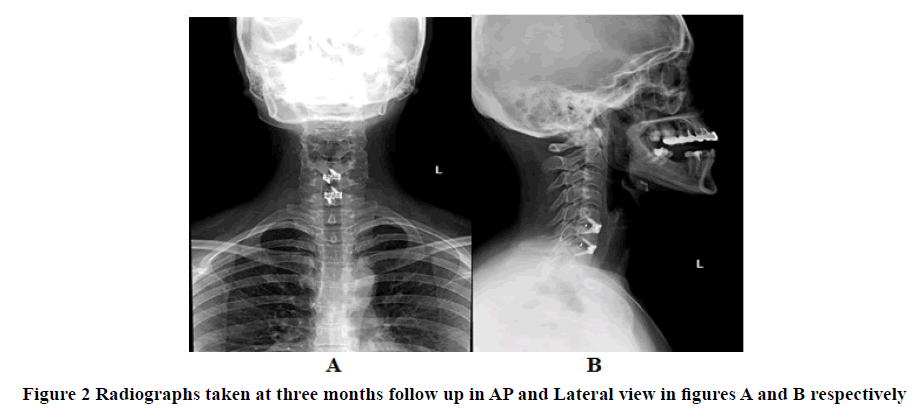
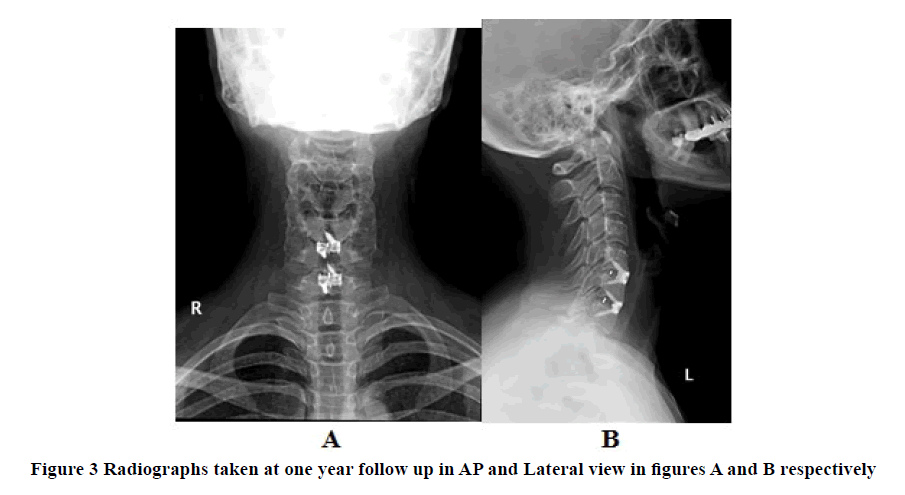
All the patients were seen in our clinic at three months, and one year after the surgery. Cervical spine X-rays were done at three months (Figure 2) and one year (Figure 3) and calculations were made for disc height to record subsidence.
Results
The analysis was conducted using Statistical Package for the Social Science (SPSS) software, version 23 (SPSS Inc., Chicago, Illinois, USA) is used for data entry and analysis.
Table 1 list all the patient's demographic characteristics, while Table 2 shows the indications, radiological outcomes at pre-op, immediate post-op, and 12 months post-op for each case.
The median pre-operative disc height was 3.8 with an interquartile range of 1.7, and the 12-months postoperative final disc height was 6 with an interquartile range of 1.3. The median pre-operative global lordotic angle was 10.2 with an interquartile range of 12, and the 12-months postoperative final global lordotic angle was 20.25 with an interquartile range of 8.89. The median pre-operative segmental lordotic angle was 1.85 with an interquartile range of 4.9, and the median 12-month postoperative final segmental lordotic angle was 9.8 with an interquartile range of 6.15 (Table 3, Table 4, and Table 5).
Table 1 Characteristics of patients included in this study
| No. | Age | Gender | Smoking Status | Segments | Intraoperative Time (Min) | Estimated Blood Loss (ml) | Length Of Hospital Stay (Days) |
|---|---|---|---|---|---|---|---|
| 1 | 42 | Female | Non-Smoker | C5/6, C6/7 | 165 | >150 | 5 |
| 2 | 68 | Male | Non-Smoker | C5/6, C6/7 | 209 | 8 | 1 |
| 3 | 42 | Male | Smoker | C5/6 | 96 | 7 | 2 |
| 4 | 56 | Male | Smoker | C5/6, C6/7 | 129 | 50 | 4 |
| 5 | 66 | Male | Smoker | C4/5, C5/6 | 195 | 200 | 3 |
| 6 | 54 | Female | Non-Smoker | C5/6 | 178 | 6 | 4 |
| 7 | 72 | Male | Smoker | C4/5 | 146 | 100 | 4 |
| 8 | 56 | Female | Non-Smoker | C5/6 | 107 | 50 | 3 |
| 9 | 71 | Male | Smoker | C4-5 | 102 | 15 | 8 |
| 10 | 52 | Female | Non-Smoker | C5-C6-C6-C7 | 159 | 15 | 4 |
| 11 | 34 | Male | Non-Smoker | C5-6 | 77 | 5 | 2 |
| 12 | 40 | Male | Non-Smoker | C5-6 | 74 | 7 | 5 |
| 13 | 39 | Female | Non-Smoker | C5-6 | 72 | 5 | 2 |
| 14 | 59 | Male | Non-Smoker | C3-4 | 74 | 6 | 3 |
| 15 | 54 | Female | Non-Smoker | C5-6 | 76 | 7 | 2 |
| 16 | 29 | Male | Non-Smoker | C5-6/C6-7 | 84 | 11 | 2 |
| 17 | 44 | Female | Non-Smoker | C5-6/C6-7 | 82 | 9 | 2 |
| 18 | 43 | Female | Non-Smoker | C5-6 | 73 | 8 | 2 |
| 19 | 53 | Male | Non-Smoker | C5-6 | 78 | 14 | 3 |
| 20 | 58 | Male | Non-Smoker | C5-6 | 69 | 6 | 2 |
Table 2 Indication, Radiological outcome pre-op, post-op, and 12 months post-op for each case
| Sr. No. | Indication of Surgery | Preop Radiology/Clinical outcome | Postop Radiology/Clinical outcome | 12 months postop Radiology/Clinical outcome | ||||||
| Disc height (mm) | GLA (1) (degrees) | SLA (2) (degrees) | Disc height (mm) | GLA (degrees) | SLA (degrees) | Disc height (mm) | GLA (degrees) | SLA (degrees) | ||
| 1 | Cervical stenosis+radiculopathy | C5-6: 4.33 | 7.1° | 0.8° | C5-6: 6.77 | 14.6° | 16.2° | C5-6: 6.93 | 20.8° | 15.4° |
| C6-7: 4.62 | C6-7: 7.02 | C6-7: 7.02 | ||||||||
| 2 | Cervical stenosis and myelopathy | C5-6: 2.37 | 10.6° | 6.4° | C5-6: 5.56 | 18.4° | 11.4° | C5-6: 2.83 | 11.3° | 5.2° |
| C6-7: 4.69 | C6-7: 6.11 | C6-7: 5.55 | ||||||||
| 3 | Degenerative disc+myelomalacia | C5-6: 5.59 | 31° | 1° | C5-6: 6.98 | 25.5° | 4.1° | C5-6: 5.48 | 37° | 7.5° |
| 4 | Cervical spinal+Myelopathy | C5-6: 3.88 | 17.7° | 1.6° | C5-6: 5.97 | 21.6° | 8.9° | C5-6: 5.65 | 19.03° | 8.4° |
| C6-7: 3.77 | C6-7: 6.94 | C6-7: 6.56 | ||||||||
| 5 | Cervical stenosis+radiculopathy+myelopathy | C4-5:3.79 | 9.7° | 3.2° | C4-5:6.63 | 23.5° | 16.7° | C4-5:6.58 | 24.6° | 12.9° |
| C5-6:3.48 | C5-6:6.98 | C5-6:6.93 | ||||||||
| 6 | Cervical stenosis+radiculopathy | C5-6: 3.6 | 2.4° | 7.9° | C5-6: 6.68 | 3.9° | 12° | C5-6: 6.68 | 15° | 12° |
| 7 | Cervical stenosis+radiculopathy | C4-5: 5.94 | 10.2° | 3° | C4-5: 7.82 | 11.7° | 12° | C4-5: 5.51 | 19° | 9.3° |
| 8 | Cervical myelopathy | C5-6: 5.93 | 10.2° | 7.5° | C5-6: 5.85 | 6.2° | 3.9° | C5-6: 5.68 | 3° | 5.7° |
| 9 | Cervical stenosis (brown-Sequard syndrome)+myelomalacia | C4-5: 7.9 | 20.9° | 5.4° | C4-5: 7.58 | 16.5° | 5.1° | C4-5: 7.58 | 25.8° | 5° |
| 10 | Cervical stenosis+myelopathy | C5-6: 1.81 | 4.1° | 0.6° | C5-6: 6.57 | 9.4° | 9° | C5-6: 6.58 | 8.6° | 2.1° |
| C6-7: 3.64 | C6-7: 6.57 | C6-7: 2.65 | ||||||||
| 11 | Cervical stenosis+myelomalacia (radiculopathy) | C5-6: 3.9 | 3.6° | 1.6° | C5-6: 5.9 | 11.7° | 8.5° | C5-6: 5.9 | 12.4° | 8.5° |
| 12 | Radiculopathy+myelopathy | C5-6: 3.7 | 7° | 0.5° | C5-6: 7 | 20° | 14.1° | C5-6: 7 | 25° | 14.1° |
| 13 | Cervical myelopathy | C4-5: 2.9 | -1° | -2.1° | C4-5: 4.9 | 11° | 9° | C4-5: 4.9 | 12.1° | 9° |
| 14 | Cervical myelopathy | C3-4: 3.9 | 14.9° | -3.6° | C3-4: 6.8 | 15.4 ° | -1.4° | C3-4: 6.8 | 18.9° | -1.4° |
| 15 | Cervical radiculopathy | C5-6: 3.8 | 20.5° | 0.9° | C5-6: 5.9 | 28.4 ° | 11.1° | C5-6: 5.6 | 28.1° | 11° |
| 16 | Cervical radiculopathy | C5-6: 3.7 | 25.1° | 16° | C5-6: 5.9 | 12.8° | 23° | C5-6: 5.9 | 26.2° | 23.1° |
| C6-7: 4.5 | C6-7: 6.9 | C6-7: 6.9 | ||||||||
| 17 | Cervical radiculopathy | C5-6: 2.9 | 7.1° | 4° | C5-6: 6.1 | 16.2° | 19.9° | C5-6: 6.1 | 19.7° | 19.9° |
| C6-7: 3.2 | C6-7: 6.1 | C6-7: 6.1 | ||||||||
| 18 | Cervical radiculopathy | C5-6: 1.4 | 5.6° | -1.5° | C5-6: 5.9 | 8.2° | 7.5° | C5-6: 5.9 | 15.8° | 7.8° |
| 19 | Cord compression+radiculopathy | C5-6: 2.9 | 17.3° | -2.6° | C5-6: 6.9 | 25.3° | 10.3° | C5-6: 6.9 | 27.1° | 10.3° |
| 20 | Cervical stenosis+radiculopathy | C5-6: 4.1 | 16.6° | 2.1° | C5-6: 7.1 | 21.4° | 11.5° | C5-6: 7.1 | 24.2° | 11.3 ° |
Legend: 1-Global Lordotic Angle, 2-Segmental Lordotic Angle.
Table 3 Median and Interquartile range of pre-operative, immediate post-operative, and 12-months post-operative disc height
| Pre-operative disc height | Immediate post-op disc height | 12 months post-op disc height | |
|---|---|---|---|
| Median | 3.8 | 6.6 | 6 |
| IQR | 1.7 | 1 | 1.3 |
Table 4 Median and Interquartile range of pre-operative, immediate post-operative, and 12-months post-operative global lordotic angle
| Pre-op Global Lordotic Angle | Post-op Global Lordotic Angle | 12-months post-op Global Lordotic Angle | |
|---|---|---|---|
| Median | 10.2 | 6.35 | 20.25 |
| IQR | 12 | 10.95 | 11.55 |
Table 5 Median and Interquartile range of pre-operative, immediate post-operative, and 12-months post-operative segmental lordotic angle
| Pre-op Segmental Lordotic Angle | Post-op Segmental Lordotic Angle | 12-months post-op Segmental Lordotic Angle | |
|---|---|---|---|
| Median | 1.85 | 11.25 | 9.8 |
| IQR | 4.9 | 6.37 | 6.15 |
We want to report further that none of our patients developed hoarseness of voice after surgery. Although that wasn't the variable under research, that was an additional finding.
Discussion
Even though ACDF has been associated with high osseous fusion rates, pseudarthrosis is still a significant complication. Given that there is a lack of standard criteria for determining fusion, pseudarthrosis rates after ACDF vary widely [19]. Nevertheless, has reported the percentage of pseudarthrosis to be 2.6%, with a reduction of pseudarthrosis rate when using autograft fusion compared to allograft fusion [19]. It has also been found that patients who underwent ACDF with a standalone cage had a higher pseudarthrosis rate than the patients who underwent the same procedure in addition to plate fixation [20].
However, in Hwang SL, et al. study patients who underwent titanium cage assisted-ACDF had long-term stabilization, increased lordosis, increased segmental height, and increased foraminal size in comparison to patients who underwent the same procedure in addition to plate fixation [9]. Moreover, the cage-only group patients had a lower complication rate and shorter hospital stays.
Furthermore, fusion rates were reported variably as well. In a study, both cage and plate use resulted in a higher fusion rate [20]. On the other hand, Kaiser MG, et al. reported fusion rates for one- and two-level ACDF with anterior fixation was 96% and 91%, respectively, compared to 90% and 72% for one- and two-level ACDF without anterior fixation [21].
The unsettlement of the adverse effects and reduced biomechanical stability of interbody cages was reported in the literature [22]. Goel first described a modification by discussing bicortical and tricortical screws integrated with the cage in 1997 [23]. The technique's idea was to position the screws in an oblique matter to engross the body's anterior cortex, traverse the cortices, and adjoin the disc space to enhance stabilization [24].
We, therefore; reported 20 cases of which an ACDF with coalition integrated plate and spacer system was the surgeon's method of choice, and we observed radiological outcomes in terms of disc height, global lordotic angle, and segmental height at three different time intervals which are pre-operatively, immediately postoperatively, and at 12 months post-operation as seen in Table 2 previously. According to the subsidence definition found in the literature, which is a decrease in disc height more than 3 mm from the immediate postoperative image until the 12 months postoperative image, none of the cases we reported has faced subsidence [25]. Similarly, a study with the same method used said 80% of their subjects had some degree of implant subsidence, yet none of their patients had subsidence >2 mm or collapse of any segment [26].
We operated on all the patients through the left-sided incision; there is enough data to support the left-sided approach based on its benefits, especially avoidance of the injury to the recurrent laryngeal nerve. We want to report further that none of our patients develop a change in voice after surgery. Although that wasn't the variable under research, that was an additional finding. The Left-sided approach followers believe that the recurrent laryngeal nerves follow an inconsistent course in the lower neck and increase the risk of Recurrent Laryngeal Nerve Palsy (RLNP) [27]. On the other hand, proponents of the right-sided approach confirmed that the right-sided method is technically easier for right-handed surgeons. There is a high incidence of right-sided RLNP because most of the data are from left-sided surgeries [28,29]. Recently, Johnson, et al. showed in their work that there is no increased risk associated with either approach [30]. In another series by Justin M. Haller, and his colleagues reported that superior to C7-T1, both RLNs had similar anatomic courses and received equal protection via soft-tissue [31]. So, they supposed there was not a side-to-side difference. The selection of side for ACDF is based chiefly on the surgeon’s preference unless there is a specific, compelling indication to advocate one approach over another. All of our patients reported complete resolution of symptoms and were satisfied with the surgical outcome at 12 months follow-up. According to Odom's criteria of surgical outcomes, all patients were graded excellent [32].
Limitation
Shortcomings of this study may include a small sample size. We suggest that the method of ACDF and its sequelae needs to be observed on larger sample sizes to give a more definitive answer on the pros and cons of ACDF with a standalone cage-plate system.
Conclusion
In conclusion, ACDF with a standalone cage-plate system has shown excellent fusion, clinical and radiological outcomes with no subsidence and pseudoarthrosis in short term.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
Ethics Approval and Consent to Participate
Ethical approval was granted by our institutional review board following the National Committee of Bio-Ethics (NCBE) guidelines with the IRB number of KSU-IRB 017E.
Availability of Data and Materials
The datasets used and analyzed during the current study are available from the corresponding author on request.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors’ Contributions
Waleed Awwad reviewed the final version of the manuscript. Rohail Mumtaz contributed to the study design and manuscript preparation and performed the literature review and statistical analysis. Khalid Alasaleh, Abdulaziz Almaawi, and Waleed Albishi contributed to the study design and manuscript preparation. Sarah Aljasser and Mana Almuhaideb contributed to the study design and data collection. Waleed Awwad contributed to the manuscript preparation and data collection. Rohail Mumtaz contributed to the manuscript preparation and data collection. All authors read and approved the final manuscript.
Acknowledgments
This work was supported by the College of Medicine Research Centre, Deanship of Scientific Research, King Saud University, Riyadh, Saudi Arabia.
References
- Smith, George W., and Robert A. Robinson. "The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion." The Journal of Bone & Joint Surgery, Vol. 40, No. 3, 1958, pp. 607-24.
- Cloward, Ralph B. "The anterior approach for removal of ruptured cervical disks." Journal of Neurosurgery, Vol. 15, No. 6, 1958, pp. 602-17.
- Cho, Hyun-Jun, et al. "Cervical Stand-alone polyetheretherketone cage versus zero-profile anchored spacer in single-level anterior cervical discectomy and fusion: Minimum 2-year assessment of radiographic and clinical outcome." Journal of Korean Neurosurgical Society, Vol. 58, No. 2, 2015, pp. 119-24.
- Gerszten, Peter C., et al. "Outcomes evaluation of zero-profile devices compared to stand-alone peek cages for the treatment of three-and four-level cervical disc disease." Cureus, Vol. 8, No. 9, 2016, p. e775.
- Fujibayashi, Shunsuke, Masashi Neo, and Takashi Nakamura. "Stand-alone interbody cage versus anterior cervical plate for treatment of cervical disc herniation: Sequential changes in cage subsidence." Journal of Clinical Neuroscience, Vol. 15, No. 9, 2008, pp. 1017-22.
- Han, Sang Youp, et al. "Stand-alone cages for anterior cervical fusion: Are there no problems?" Korean Journal of Spine, Vol. 13, No. 1, 2016, pp. 13-19.
- Jagannathan, Jay, et al. "Radiographic and clinical outcomes following single-level anterior cervical discectomy and allograft fusion without plate placement or cervical collar." Journal of Neurosurgery: Spine, Vol. 8, No. 5, 2008, pp. 420-28.
- Gercek, Erol, et al. "Subsidence of stand-alone cervical cages in anterior interbody fusion: Warning." European Spine Journal, Vol. 12, No. 5, 2003, pp. 513-16.
- Hwang, Shiuh-Lin, et al. "Three-level and four-level anterior cervical discectomies and titanium cage-augmented fusion with and without plate fixation." Journal of Neurosurgery: Spine, Vol. 1, No. 2, 2004, pp. 160-67.
- Shin, Jae Sik, Sung Han Oh, and Pyoung Goo Cho. "Surgical outcome of a zero-profile device comparing with stand-alone cage and anterior cervical plate with iliac bone graft in the anterior cervical discectomy and fusion." Korean Journal of Spine, Vol. 11, No. 3, 2014, pp. 169-77.
- Melgar, Miguel A., et al. "Segmental and global lordosis changes with two-level axial lumbar interbody fusion and posterior instrumentation." International Journal of Spine Surgery, Vol. 8, 2014.
- Sanden, B., et al. "The significance of radiolucent zones surrounding pedicle screws: Definition of screw loosening in spinal instrumentation." The Journal of Bone and Joint Surgery. British Volume, Vol. 86, No. 3, 2004, pp. 457-61.
- Phillips, Frank M., et al. "A prospective, randomized, controlled clinical investigation comparing PCM cervical disc arthroplasty with anterior cervical discectomy and fusion: 2-year results from the US FDA IDE clinical trial." Spine, Vol. 38, No. 15, 2013, pp. E907-18.
- Bohlman, H., et al. "Robinson anterior cervical discectomy and arthrodesis for cervical." The Journal of Bone & Joint Surgery, Vol. 75, No. 9, 1993, pp. 1298-307.
- Cho, Der-Yang, Wen-Yen Lee, and Pon-Chun Sheu. "Treatment of multilevel cervical fusion with cages." Surgical Neurology, Vol. 62, No. 5, 2004, pp. 378-85.
- Banwart, J. Christopher, Marc A. Asher, and Ruth S. Hassanein. "Iliac crest bone graft harvest donor site morbidity. A statistical evaluation." Spine, Vol. 20, No. 9, 1995, pp. 1055-60.
- Silber, Jeff S., et al. "Donor site morbidity after anterior iliac crest bone harvest for single-level anterior cervical discectomy and fusion." Spine, Vol. 28, No. 2, 2003, pp. 134-39.
- Yang, Jae Jun, et al. "Subsidence and nonunion after anterior cervical interbody fusion using a stand-alone Polyetheretherketone (PEEK) cage." Clinics in Orthopedic Surgery, Vol. 3, No. 1, 2011, pp. 16-23.
- Shriver, Michael F., et al. "Pseudoarthrosis rates in anterior cervical discectomy and fusion: A meta-analysis." The Spine Journal, Vol. 15, No. 9, 2015, pp. 2016-27.
- Song, Kyung-Jin, et al. "The efficacy of plate construct augmentation versus cage alone in anterior cervical fusion." Spine, Vol. 34, No. 26, 2009, pp. 2886-92.
- Kaiser, Michael G., et al. "Anterior cervical plating enhances arthrodesis after discectomy and fusion with cortical allograft." Neurosurgery, Vol. 50, No. 2, 2002, pp. 229-38.
- Shimamoto, Norimichi, et al. "Biomechanical evaluation of stand-alone interbody fusion cages in the cervical spine." Spine, Vol. 26, No. 19, 2001, pp. E432-36.
- MCH, Atul Goel. "Alternative tricortical methods of screw implantation for anterior cervical plate fixation: A preliminary report." Journal of Clinical Neuroscience, Vol. 7, No. 2, 2000, pp. 134-36.
- Goel, A. "Tricortical cervical inter-body screw fixation." Journal of Postgraduate Medicine, Vol. 43, No. 1, 1997, pp. 4-7.
- Park, Jae-Young, et al. "Subsidence after single-level anterior cervical fusion with a stand-alone cage." Journal of Clinical Neuroscience, Vol. 33, 2016, pp. 83-88.
- Kasliwal, Manish K., and John E. O’toole. "Integrated intervertebral device for anterior cervical fusion: An initial experience." Journal of Craniovertebral Junction and Spine, Vol. 3, No. 2, 2012, pp. 52-57.
- Jung, Axel, et al. "Recurrent laryngeal nerve palsy during anterior cervical spine surgery: A prospective study." Journal of Neurosurgery: Spine, Vol. 2, No. 2, 2005, pp. 123-27.
- Ebraheim, Nabil A., et al. "Vulnerability of the recurrent laryngeal nerve in the anterior approach to the lower cervical spine." Spine, Vol. 22, No. 22, 1997, pp. 2664-67.
- Weisberg, Noah Kawika, Dan M. Spengler, and James L. Netterville. "Stretch-induced nerve injury as a cause of paralysis secondary to the anterior cervical approach." Otolaryngology-Head and Neck Surgery, Vol. 116, No. 3, 1997, pp. 317-26.
- Johnson, Mark D., et al. "Right versus left approach to anterior cervical discectomy and fusion: An anatomic versus historic debate." World Neurosurgery, Vol. 135, 2020, pp. 135-40.
- Haller, Justin M., Michael Iwanik, and Francis H. Shen. "Clinically relevant anatomy of recurrent laryngeal nerve." Spine, Vol. 37, No. 2, 2012, pp. 97-100.
- Broekema, Anne EH, et al. "The odom criteria: validated at last: A clinimetric evaluation in cervical spine surgery." The Journal of Bone & Joint Surgery, Vol. 101, No. 14, 2019, pp. 1301-08.