Research - International Journal of Medical Research & Health Sciences ( 2022) Volume 11, Issue 2
Sexual Life Importance in Patients with Reproductive Cancers: A Questionnaire-Based Study
Maria Grazia Criscuolo1*, Stefania Perna1, Carla Di Stefano2, Arturo Hermann3 and Gabriella Marfe12Department of Hematology Tor Vergata University, Rome, Italy
3Italian National Institute of Statistics (ISTAT), Rome, Italy
Maria Grazia Criscuolo, Department of Environmental, Biological and Pharmaceutical Sciences and Technologies, University of Campania Luigi Vanvitelli, Italy, Email: mariagrazia.criscuolo1982@gmail.com
Received: 04-Feb-2022, Manuscript No. ijmrhs-22-53492 (M); Editor assigned: 08-Feb-2022, Pre QC No. ijmrhs-22-53492 (P); Reviewed: 19-Feb-2022, QC No. ijmrhs-22-53492 (Q); Revised: 23-Feb-2022, Manuscript No. ijmrhs-22-53492 (R); Published: 28-Feb-2022
Abstract
Although several studies point out that cancer therapy can contribute to problems in sexual function, more research is needed to better understand the concerns and information of cancer patients about sexual life. This study aimed to identify the sexual life importance and the quality of communication with oncologists on this topic in patients with reproductive cancers. A total of 251 cancer patients from the oncological department completed a self-reported questionnaire along with two oncological consultations (T0 and T12 after 12 months). Chi-square analysis and t-test methods were used to compare the sexual life importance and quality communication of these patients according to gender, age, and education. The data of our study showed that male patients considered more important their sex life than female patients at the first consultation (T0). At the second consultation, (T12), a general increase of sexual life importance resulted for both sexes, along with a slight decrease in the difference between male and female patients. Regarding communication about sexual life, we observed at T0 that the female patients were more embarrassed to talk about their sexual life with their oncologist in respect to male patients. After one year (T12), there was a general increase in quality communication, accompanied by a moderate reduction of the difference between sexes. The importance of sexual life and the related quality of communication with the oncologists/Healthcare Professionals (HCPs)/Oncological Nurses (ONs) tend to significantly increase during the treatment. Implications for Practice: This study is limited in that specific sexual life concerns were determined with self-report measures. All health professionals did not always recognize emotional cues other than those related to physiological complaints. It follows that the issue of sexuality must be incorporated in interventions offered in the context of care for these women and men.
Keywords
Communication, Sexual life importance, Cancer patients, Oncologists, Breast cancer, Prostate cancer, Oncological consultation
Introduction
Sexuality plays a crucial role in the life of every person since it encompasses the physical, psychological, social, and cultural dimensions of the individuals. Different studies recognized how a cancer diagnosis and its treatment can impact the self-image and physical changes of the patients [1-3]. In this regard, many cancer patients reported many sexual problems that can also persist after the treatment [4-9]. For example, one study reported that among 40% and 100% of cancer patients experienced sexual disorders for both women and men [10,11]. Specifically, among men, prostate cancer patients have erectile dysfunction after prostatectomy, radiation, or hormone therapy [11]. Furthermore, these cancer patients try to face major challenges in sorting through new remedies to impotence and in finding new sexual terrain with their partners [12-14]. Furthermore, women after breast or gynaecology cancers reported different sexual dysfunctions such as decreased libido, and vaginal dryness [15]. Other studies observed that both male and female patients received less information about the potential sexual risks of the therapy in oncology care settings [16-21]. In particular, Reese, et al., observed that a sexual consultation was offered only to 22% of men and 17% of women during cancer treatment [22]. Although practice guidelines include discussion of sexual life for cancer patients, most of them do not have discussions on these topics with oncologists/Healthcare Professionals (HCPs)/Oncological Nurses (ONs) [23-26]. In a study, 76% of breast cancer patients reported that it was important to discuss treatment-related sexual problems with their oncologists, yet only 33% received such information [27]. Moreover, many patients are reluctant to communicate their sexuality to oncologists/HCPs/ONs because they very often feel a strong embarrassment to talk about these topics [28]. In another study, Reese, et al., observed that approximately 1/3 (22/67 patients) of women with breast cancer had sexual problems, and only 45% (10/22 patients) of them were able to have sexual health communication [29]. Furthermore, the authors reported that the discussion on sexual health occurred only with 27 patients (40%) and generally, the oncologists started the discussion in 72% of cases. The authors concluded that communication about sexual health was uncommon even for women reporting sexual problems [29]. Furthermore, the Quality of Life (QoF) is a critical aspect related to different kinds of cancer. In this regard, cancer can produce negative consequences in several areas of a cancer patient’s life [30-33]. In this scenario, effective communication between a cancer patient and oncologist/HCP can help to identify the sexual problems of patients after a diagnosis of cancer [34- 38]. Many gaps are persisting in knowledge about patient-oncologists/HCPs/ONs communication on sexual health in reproductive cancers. Few studies have examined the importance of these discussions and their relationship with the health status (both physical and mental) of cancer patients. The primary aim of this study was to better understand, through a simple questionnaire, (1) the sexual life importance in patients with reproductive cancers and (2) the quality of communication about these topics with the oncologists/HCPs/ONs.
Materials and Methods
Sample
The study sample consisted of participants from 18 years on, with a diagnosis of different kinds of cancer (such as breast, cervix, or prostate and testicle), who were attending an oncology outpatient. The study was conducted in a sample of 251 cancer patients and approved by the Ethics Committee of the Medical Faculty of the University. Informed consent was obtained from all individual participants included in this study before the initial oncological consultation.
Recruitment and Data Collection
The recruitment period was from 2017 and 2019 in a sample of 251 cancer patients (144 females and 107 males with a mean age of 47 years). Of these, 253 respondents completed the written informed consent form, resulting in a 98.6% response rate. After excluding two subjects who did not answer or fill in a blank, 251 subjects were finally included in the analysis. One of the researchers (MGC) trained the research staff to seek participants’ consent and collect data for this study. The research staff explained the purpose and procedure of this study to the subjects who then agreed to participate. The questionnaire was then distributed to the subjects in a separate room at the outpatient department. The time required to complete the questionnaire was approximately 20 min. There was no incentive to participate in this study.
Instrument
A brief questionnaire was given to the participants, which consisted of two parts: the first, asking general information about the age, sex, education level, marital status, and job. The second consists of the analysis of (1) sexual life importance and (2) quality of communication with oncologists/HCPs/ONs on sexual issues. Sexual life importance and quality of communication were measured with 2 items using the EORTC SHQ-C22 questionnaire at first oncological consultation (T0) and another oncological consultation after 12 months (T12). All items were assessed with a fivepoint Likert scale ranging as follows; 1 (not at all), 2 (a little), 3 (moderate amount), 4 (much), 5 (very much). Details of cancer site, cancer stage, time, and treatment were obtained from patients’ medical records.
Moreover, some participants’ written comments in response to the Open-Ended Question (What do you think about sex life after diagnosis and during the therapy?) were reported during the two oncological consultations (in Italian language and translated into English). In these comments, the cancer patients tried freely to figure out their emotions, their fears, their concerns, and their plans for the future. The transcripts of answers to the open-ended question were analyzed by all investigators according to the themes that emerged and were reported in the supplementary data.
Statistical Analysis
All statistical analyses were performed using the Statistical Package for Social Sciences (version 23, SPSS Statistics, IBM Corp, Chicago IL, USA, 2016). The socio-demographic characteristics and disease characteristics of the cancer patients were analyzed by using descriptive statistics. The importance of sex life and quality of communication with oncologists/HCPs/ONs according to gender, age and education were analyzed by Chi-square and t-test methods. To secure more reliable statistical results-as for other variables like type and stage of cancer there is too little data-the analysis was concentrated on three macro variables: gender, age, and education.
Results
Socio-Demographic Characteristics
At the time of the first visit, all patients filled out a brief socio-demographic questionnaire. Among our patients (pts=251), the mean age was 47 years (S.D. 10.44) and there were more females (57.37% =144) than males (42.62% n=107), respectively (Table 1). 60.55% of participants were employed, while 29.44% were not employed. Furthermore, 40.23% of patients had low education, while 59.76% had a high education (Table 1). The most common cancer type was breast cancer (32.5%) among the female patients, followed by cervix cancer (19.92%). Of the 107 male patients, 24.5% (n=59) had prostate cancer, while 19.12% (n=48) had a testicular germ-cell cancer. Most patients had in situ (54.98%), in situ, and local (27.49%) in situ and distant (17.2%) cancers and they had received surgical, surgical/ chemotherapy, or surgical/radiological (72.49%) treatment (Table 1).
| Characteristic | No. | % |
|---|---|---|
| Age/years | ||
| Mean | 47.82 | |
| S.D. | 10.44; Range=30-81 | |
| <60 | 223 | 88.84% |
| >60 | 28 | 11.15% |
| Sex | ||
| Female | 144 | 57.37% |
| Male | 107 | 42.62% |
| Marital Status | ||
| Unmarried | 88 | 35.05% |
| Married | 147 | 56.56% |
| Divorced | 16 | 6.37% |
| Education | ||
| Less than high school | 101 | 40.23% |
| High school and above | 150 | 59.76% |
| Employment | ||
| Yes | 152 | 60.55% |
| No | 99 | 29.44% |
| Cancer type | ||
| Breast | 94 | 37.45% |
| Cervix | 50 | 19.92% |
| Prostate | 59 | 23.50% |
| Testicular Germ-Cells (TGCs) | 48 | 19.12% |
| SEER stage | ||
| In situ | 138 | 54.98% |
| In situ and local | 69 | 27.49% |
| In situ and distant | 44 | 17.52% |
| Treatment received | ||
| Surgery | 13 | 5.17% |
| Chemotherapy | 69 | 27.49% |
| Radiotherapy | 0 | 0% |
| Surgery+Chemotherapy | 135 | 53.78% |
| Surgery+ Radiotherapy | 34 | 13.54% |
| Chemotherapy+Radiotherapy | 0 | 0% |
| SD: Standard Deviation; SEER: Surveillance Epidemiology and End Results (first consultation T0) | ||
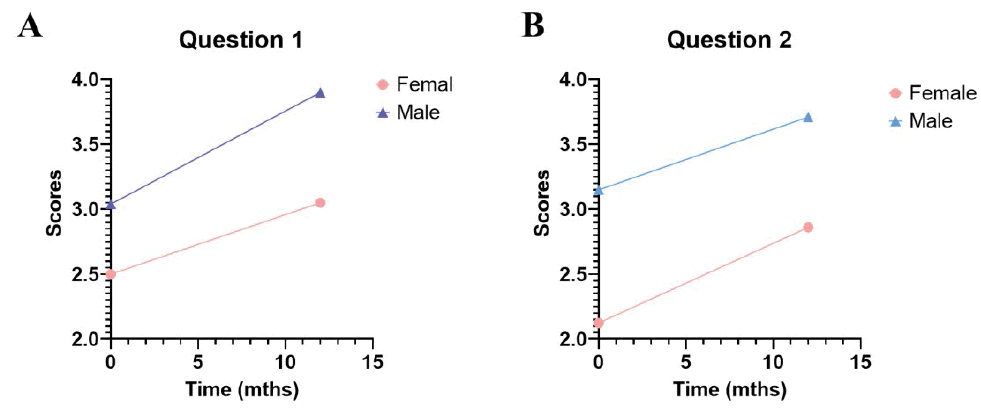
Sexual Life Importance of Cancer Patients in Two Different Consultations
In our study, all considered patients answered the questionnaire during two different consultations (T0 and T12). The sample at T0 consisted of 251 patients. The total average score for the first question on sexual life importance at the time T0 was 2.98. Considering sex, age, and education variables, the only significant difference was observed for sex, with the average score for females and males of 2.5 and 3.5 respectively (Figure 1A). Among female patients, 59% and 46.35% indicated that the sexual life was little important (score 2) or moderately important (score 3), respectively. Among male patients, 42% and 51% reported that their sexual life was moderately important (score 3) or much important (score 4), respectively. Significant differences were observed in the global scores of sexual life importance suggesting that male patients believed that the sex life was more important when compared with female patients (χ2= 9.1<0.01 t=11.8 <0.01) (Figure 1A) (Table 2).
| Items | Dimensions | Women (n=144) Mean ± SD | Men (n=107) | χ2 | (p) T (p) | |
|---|---|---|---|---|---|---|
| Sexual life | Global score | 2.9 ± 0.82 (n=251)* | ||||
| How much do you think is important in your sex life during the disease? | Not at all 1 | 2.5 ± 0.65 | 3.5 ± 0.66 | 9.1 | <0.01 11.8 <0.01 | |
| A little 2 | ||||||
| A Moderate amount 3 | ||||||
| Much 4 | ||||||
| Very much 5 | ||||||
| 2.5 ± 0.85 (n=251)* | ||||||
| Have you had communication with your oncologists about your sex life? | Not at all 1 | 2.1 ± 0.79 | 3.1 ± 0.51 | 11 | <0.01 12.5 <0.01 | |
| A little 2 | ||||||
| A Moderate amount 3 | ||||||
| Much 4 | ||||||
| Very much 5 | ||||||
| *: the whole sample | ||||||
At the second consultation (T12) the sample was reduced as 25 female patients 22 male patients died, respectively and hence the total sample was composed of 172 patients. The importance attributed to sex life (question 1) increased for both male and female patients by reaching the total average of 3,4, whereas the average score for females was 3,04 and for males 3.9 (Figure 1A). 81% of female patients believed that the sexual life was moderately (score 3) or much important (score 4), while 95% of male patients believed that the sexual life was much (score 4) or very much important (score 5).
The difference between male and female patients about the importance of sexual life significantly reduced over the considered time (χ2= 3.9<0.01 t=12.8<0.01) (Figure 1 A) (Table 3). In both T0 and T12 consultations, the individual scores behaved in “normal ways” with the higher frequencies about the average. We did not find a significant difference in the sexual life importance of the patients considering the age or the education (data not shown) in both consultations.
| Items | Dimensions | Women (n=103) Mean ± SD | Men (n=69) | χ2 | (p) T (p) |
|---|---|---|---|---|---|
| Sexual life | Global score | 3.4 ± 0.70 (n=172)* | |||
| How much do you think it is important your sex life during the disease? | Not at all 1 | 3.04 ± 0.64 | 3.9 ± 0.34 | 3.9 | <0.05 12.2 <0.01 |
| A little 2 | |||||
| A Moderate amount 3 | |||||
| Much 4 | |||||
| Very much 5 | |||||
| 3.2 ± 0.70 (n=172)* | |||||
| Have you had communication with your oncologists about your sex life | Not at all 1 | 2.86 ± 0.59 | 3.71 ± 0.54 | 4.4 | <0.05 12.2 <0.01 |
| A little 2 | |||||
| A Moderate amount 3 | |||||
| Much 4 | |||||
| Very much 5 | |||||
| *: the whole sample | |||||
Quality on Communication of Cancer Patients in Two Different Consultations
Participants were asked if they have had communication with their oncologists/HCPs/ONs about their sexual life (question 2). The total average score for the second question at the time T0 was 2.5. Specifically, the average score for females was 2.1 and for males 3.1 (Figure 1B). The majority of the female patients (91%) answered that they had little (2) or moderate amount (3) of communication on this topic, while the majority of the male patients (90%) answered that they had communication in moderate amount (3) on after first consultation (T0).
At the second consultation (T12), the quality of communication on sex life with their oncologists increased for both male and female patients by reaching a total average of 3.2, whereas the average score for females was 2.8 and for males 3.7 respectively (Figure 1B). The female patients (74%) answered that they had communication in moderate amount (3) on their sexual life, while the 14% and 75% of male patients answered that they had communication in moderate amount (3) or much important (4) on their sex life, respectively. The difference between male and female patients about the communication on their sexual life with their oncologists was highly significant (χ2=11<0.01 t=12.5<0.01) (Figure 1B) (Table 3) at the first consultation (T0). After one year (T12), we observed a decreased difference between female and male patients (χ2=4.4<0.05 t=12.2<0.01) (Table 3).
We did not find a significant difference in the quality of communication about the sexual life of the patients considering as variables the age or the education (data not shown) in both consultations.
Discussion
Different studies have pointed out that cancer may negatively impact the sexual function and sexual activity of cancer patients [39-41]. Generally, sexual health is correlated with physical, emotional, mental, and social wellbeing World Health Organization (WHO) [42]. This is a major issue for cancer patients who can often suffer from both sexual dysfunctions (such as erectile dysfunction or vaginal dryness) and psychological distress (such as body image and the formation relationships) [43-45]. Hence, these problems can be addressed through effective and emotional communication between oncologists/HCPs/ONs and patients [46-49].
Our study examined the sexual life importance and the quality of communication for reproductive cancers outpatients through a brief questionnaire in two different consultations at T0 and T12. At the beginning (T0), we observed that the sexual life importance of male patients was higher than those of female patients who (most of them) believed that their sexual life was not so important after a cancer diagnosis. We supposed that the female patients might be very embarrassed to talk about their sex life after a cancer diagnosis (T0). Therefore, oncologists/HCPs/ONs should support in particular female patients for coping with their sexual problems and their reluctance to ask for professional help. This result is following two previous studies showing that female patients talked less with oncologists/HCPs/ONs regarding sexual life than male patients [50,51]. The first study reported that only 4.8% of female patients talked with oncologists/HCPs/ONs about their sex life, whereas 21% of male patients did [50]. In the second study, Gilbert, et al., observed that approximately only 43% of female patients had communication with an oncologist/HCPs/ONs compared to 68% of male patients [51]. After one year, we noted that sex life importance become moderately or very important in most female patients (81%). This can happen because the emotional impact of cancer diagnoses, isolation, and loss of self-esteem can be reduced to face more easily their fear of sexual life after a year (T12). Furthermore, we reported the same result on the quality of communication on these topics: 1) the majority of the female patients (91%) had little communication with their oncologists/HCPs/ONs at T0; 2) the quality of communication increased for both sexes after a year. In this context, we could suppose that the behaviour of these patients can be linked both to increased confidence with their oncologist/HCPs/ONs and to a strong awareness of their sexual problems after treatment, evidenced by the short interviews given by some patients (Supplementary Data) [52-55]. Our results also suggest substantial room for improvement in clinical communication about sexual life for reproductive cancer patients [22,29,55]. In other words, it is necessary to support the emotional stability of all patients by providing good information and communication during cancer patient counselling. In this regard, the modifications that occur in the sexuality of cancer patients can be so profound and mutilating that the whole affective and sexual patients’ life can be impaired. Also, cancer could predispose to psychological and social isolation, based on negative feelings that permeate interpersonal relations. In this regard, both oncologists and other HCPs/ONs have to be aware of changes to sexuality and intimacy after cancer. Thus, they should be trained in communication skills to recognize the needs of patients [56-58]. On the other hand, oncologists/HCPs/ONs need more time to better understand what patients verbalize during oncological consultations [38,50,51]. In conclusion, oncologists/HCPs/ONs should not ignore the importance of sexuality for the physical and psychological well-being of the person with cancer. In the future, all oncological health professionals (oncologists/ HCPs/ONs) should ask themselves: is this person in need of factual knowledge, or is she/he more in need of emotional support? This is indeed a major challenge for future health care.
Conclusion
Discussion about sexual health for cancer patients is important for choosing the appropriate treatment pathways and improving the patient-oncologist/HCP/ON relationship. In this context, it will be possible to better address a range of sexual problems that patients with reproductive cancers experience during their treatment. In this way, clinical discussions of sexual health will lead to the implementation of effective solutions and better outcomes for patients.
Declarations
Acknowledgements
The research team wishes to thank all the people with cancer that participated in the study. All research staff who helped them complete the questionnaire after the oncological consultations The team also wishes to thank Vittoria De Santis for your help and methodological support.
Conflict of Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval
The authors declare that all the research meets the ethical guidelines.
Funding
The author(s) received no financial support for the research.
Authors’ Contributions
Maria Grazia Criscuolo and Stefania Perna conceived and planned the project. Gabriella Marfe, Carla Di Stefano, and Stefania Perna participated in study design in the development of methods for data collection and analysis. Arturo Hermann has developed a methodology, software, formal analysis, and data curation. All authors contributed to the refinement of the study protocol and approved the final manuscript.
References
- Gilbert, Emilee, Jane M. Ussher, and Yasmin Hawkins. "Accounts of disruptions to sexuality following cancer: The perspective of informal carers who are partners of a person with cancer." Health, Vol. 13, No. 5, 2009, pp. 523-41.
Google Scholar Crossref - Hawkins, Yasmin, et al. "Changes in sexuality and intimacy after the diagnosis and treatment of cancer: The experience of partners in a sexual relationship with a person with cancer." Cancer Nursing, Vol. 32, No. 4, 2009, pp. 271-80.
Google Scholar Crossref - Oldertroen Solli, Karianne, et al. "Male partners’ experiences of caregiving for women with cervical cancer-A qualitative study." Journal of Clinical Nursing, Vol. 28, No. 5-6, 2019, pp. 987-96.
Google Scholar Crossref - Ben Charif, Ali, et al. "Sexual health problems in French cancer survivors 2 years after diagnosis-The national VICAN survey." Journal of Cancer Survivorship, Vol. 10, No. 3, 2016, pp. 600-09.
Google Scholar Crossref - Charif, Ali Ben, et al. "Patient discussion about sexual health with health care providers after cancer-A national survey." The Journal of Sexual Medicine, Vol. 13, No. 11, 2016, pp. 1686-94.
Google Scholar Crossref - Bober, Sharon L., and Veronica Sanchez Varela. "Sexuality in adult cancer survivors: Challenges and intervention." Journal of Clinical Oncology, Vol. 30, No. 30, 2012, pp. 3712-19.
Google Scholar Crossref - Dizon, Don S., Daphne Suzin, and Susanne McIlvenna. "Sexual health as a survivorship issue for female cancer survivors." The Oncologist, Vol. 19, No. 2, 2014, pp. 202-10.
Google Scholar Crossref - Heyne, Svenja, et al. "Frequency of sexual problems and related psychosocial characteristics in cancer patients-Findings from an epidemiological multicenter study in Germany." Frontiers in Psychology, Vol. 12, 2021.
Google Scholar Crossref - Ussher, Jane M., Janette Perz, and Emilee Gilbert. "Perceived causes and consequences of sexual changes after cancer for women and men: A mixed method study." BMC Cancer, Vol. 15, No. 1, 2015, pp. 1-18.
Google Scholar Crossref - Carter, Jeanne, et al. "Interventions to address sexual problems in people with cancer: American Society of Clinical Oncology clinical practice guideline adaptation of Cancer Care Ontario guideline." Journal of Clinical Oncology, Vol. 36, No. 5, 2018, pp. 492-511.
Google Scholar Crossref - Siegel, Rebecca, et al. "Cancer treatment and survivorship statistics, 2012." CA: A Cancer Journal for Clinicians, Vol. 62, No. 4, 2012, pp. 220-41.
Google Scholar Crossref - Akhavan, Omid, et al. "Dose-dependent effects of nanoscale graphene oxide on reproduction capability of mammals." Carbon, Vol. 95, 2015, pp. 309-17.
Google Scholar Crossref - Yang, Yueyong, et al. "An all-carbon counter electrode for highly efficient hole-conductor-free organo-metal perovskite solar cells." RSC Advances, Vol. 4, No. 95, 2014, pp. 52825-30.
Google Scholar Crossref - Chambers, Suzanne K., et al. "Erectile dysfunction, masculinity, and psychosocial outcomes: A review of the experiences of men after prostate cancer treatment." Translational Andrology and Urology, Vol. 6, No. 1, 2017, pp. 60-68.
Google Scholar Crossref - Melisko, Michelle E., Mindy Goldman, and Hope S. Rugo. "Amelioration of sexual adverse effects in the early breast cancer patient." Journal of Cancer Survivorship, Vol. 4, No. 3, 2010, pp. 247-55.
Google Scholar Crossref - Hautamaki, Katja, et al. "Opening communication with cancer patients about sexuality-related issues." Cancer Nursing, Vol. 30, No. 5, 2007, pp. 399-404.
Google Scholar Crossref - Park, Elyse R., Rebecca L. Norris, and Sharon L. Bober. "Sexual health communication during cancer care: Barriers and recommendations." The Cancer Journal, Vol. 15, No. 1, 2009, pp. 74-77.
Google Scholar Crossref - Reese, Jennifer Barsky, et al. "Sexual concerns in cancer patients: A comparison of GI and breast cancer patients." Supportive Care in Cancer, Vol. 18, No. 9, 2010, pp. 1179-89.
Google Scholar Crossref - Ligibel, Jennifer A., and Crystal S. Denlinger. "New NCCN guidelines® for survivorship care." Journal of the National Comprehensive Cancer Network, Vol. 11, No. 5S, 2013, pp. 640-44.
Google Scholar Crossref - Rasmusson, E‐M., Lars Plantin, and Eva Elmerstig. "‘Did they think I would understand all that on my own?’ A questionnaire study about sexuality with Swedish cancer patients." European Journal of Cancer Care, Vol. 22, No. 3, 2013, pp. 361-69.
Google Scholar Crossref - Lindau, Stacy Tessler, et al. "Communication about sexuality and intimacy in couples affected by lung cancer and their clinical‐care providers." Psycho‐oncology, Vol. 20, No. 2, 2011, pp. 179-85.
Google Scholar Crossref - Reese, Jennifer Barsky, et al. "Effective patient-provider communication about sexual concerns in breast cancer: A qualitative study." Supportive Care in Cancer, Vol. 25, No. 10, 2017, pp. 3199-207.
Google Scholar Crossref - Runowicz, Carolyn D., et al. "American cancer society/American society of clinical oncology breast cancer survivorship care guideline." CA: A Cancer Journal for Clinicians, Vol. 66, No. 1, 2016, pp. 43-73.
Google Scholar Crossref - National Comprehensive Cancer Network. "NCCN clinical practice guidelines in oncology (NCCN Guidelines®) survivorship, Version 2, 2019." 2019.
Google Scholar Crossref - Hordern, Amanda J., and Annette F. Street. "Communicating about patient sexuality and intimacy after cancer: Mismatched expectations and unmet needs." Medical Journal of Australia, Vol. 186, No. 5, 2007, pp. 224-27.
Google Scholar Crossref - Lynch, Orlaith, Anita O’Donovan, and Patrick J. Murphy. "Addressing treatment‐related sexual side effects among cancer patients: Sub‐optimal practice in radiation therapy." European Journal of Cancer Care, Vol. 28, No. 3, 2019, p. e13006.
Google Scholar Crossref - Flynn, Kathryn E., et al. "Patient experiences with communication about sex during and after treatment for cancer." Psycho‐oncology, Vol. 21, No. 6, 2012, pp. 594-601.
Google Scholar Crossref - Harris, Melinda G. "Sexuality and menopause: Unique issues in gynecologic cancer." Seminars in Oncology Nursing, Vol. 35, No. 2, 2019, pp. 211-19.
Google Scholar Crossref - Reese, Jennifer Barsky, et al. "Patient-clinician communication about sexual health in breast cancer: A mixed-methods analysis of clinic dialogue." Patient Education and Counseling, Vol. 102, No. 3, 2019, pp. 436-42.
Google Scholar Crossref - Chang, Wei. "The relationship between psychological treatment and quality of life of breast cancer patients." Teachers College, Columbia University, 1993.
Google Scholar Crossref - Ohsumi, Shozo, et al. "Quality of life of breast cancer patients and types of surgery for breast cancer-current status and unresolved issues." Breast Cancer, Vol. 14, No. 1, 2007, pp. 66-73.
Google Scholar Crossref - Davies, Nicola J., et al. "Information satisfaction in breast and prostate cancer patients: Implications for quality of life." Psycho‐Oncology: Journal of the Psychological, Social and Behavioral Dimensions of Cancer, Vol. 17, No. 10, 2008, pp. 1048-52.
Google Scholar Crossref - Muzzatti, Barbara, et al. "Quality of life and psychological distress during cancer: A prospective observational study involving young breast cancer female patients." BMC Cancer, Vol. 20, No. 1, 2020, pp. 1-8.
Google Scholar Crossref - Harden, Janet, et al. "The influence of developmental life stage on quality of life in survivors of prostate cancer and their partners." Journal of Cancer Survivorship, Vol. 2, No. 2, 2008, pp. 84-94.
Google Scholar Crossref - Fortune-Greeley, Alice K., et al. "Using cognitive interviews to evaluate items for measuring sexual functioning across cancer populations: Improvements and remaining challenges." Quality of Life Research, Vol. 18, No. 8, 2009, pp. 1085-93.
Google Scholar Crossref - Hill, Emily K., et al. "Assessing gynecologic and breast cancer survivors' sexual health care needs." Cancer, Vol. 117, No. 12, 2011, pp. 2643-51.
Google Scholar Crossref - Lindau, Stacy Tessler, et al. "Physical examination of the female cancer patient with sexual concerns: What oncologists and patients should expect from consultation with a specialist." CA: A Cancer Journal for Clinicians, Vol. 66, No. 3, 2016, pp. 241-63.
Google Scholar Crossref - Criscuolo MG, et al. "Analysis of oncologists and patients communication during different consultations." Journal of Community Medicine & Health Education, Vol. 8, No. 5, 2018, p. 626.
Google Scholar Crossref - Carter, Jeanne, et al. "The physical consequences of gynecologic cancer surgery and their impact on sexual, emotional, and quality of life issues." The Journal of Sexual Medicine, Vol. 10, 2013, pp. 21-34.
Google Scholar Crossref - Huffman, Laura B., et al. "Maintaining sexual health throughout gynecologic cancer survivorship: A comprehensive review and clinical guide." Gynecologic Oncology, Vol. 140, No. 2, 2016, pp. 359-68.
Google Scholar Crossref - Avis, Nancy E., et al. "Sexual functioning among early post-treatment breast cancer survivors." Supportive Care in Cancer, Vol. 26, No. 8, 2018, pp. 2605-13.
Google Scholar Crossref - World Health Organization. "Defining sexual health: report of a technical consultation on sexual health, 28-31 January 2002, Geneva." World Health Organization, 2006.
Google Scholar Crossref - Fobair, Patricia, and David Spiegel. "Concerns about sexuality after breast cancer." The Cancer Journal, Vol. 15, No. 1, 2009, pp. 19-26.
Google Scholar Crossref - Burwell, Stephanie R., et al. "Sexual problems in younger women after breast cancer surgery." Journal of Clinical Oncology, Vol. 24, No. 18, 2006, pp. 2815-21.
Google Scholar Crossref - Safarinejad, Mohammad Reza, Nayyer Shafiei, and Shiva Safarinejad. "Quality of life and sexual functioning in young women with early‐stage breast cancer 1 year after lumpectomy." Psycho‐Oncology, Vol. 22, No. 6, 2013, pp. 1242-48.
Google Scholar Crossref - Frumovitz, Michael, et al. "Quality of life and sexual functioning in cervical cancer survivors." Journal of Clinical Oncology, Vol. 23, No. 30, 2005, pp. 7428-36.
Google Scholar Crossref - Jensen, Pernille T., et al. "Longitudinal study of sexual function and vaginal changes after radiotherapy for cervical cancer." International Journal of Radiation Oncology* Biology* Physics, Vol. 56, No. 4, 2003, pp. 937-49.
Google Scholar Crossref - Golbasi, Zehra, and Ayten Senturk Erenel. "The quality of sexual life in women with gynaecological cancers." Archives of Gynecology and Obstetrics, Vol. 285, No. 6, 2012, pp. 1713-17.
Google Scholar Crossref - Brotto, Lori A., et al. "A psychoeducational intervention for sexual dysfunction in women with gynecologic cancer." Archives of Sexual Behavior, Vol. 37, No. 2, 2008, pp. 317-29.
Google Scholar Crossref - Kim, Jung-Hee, and Hyun-Kyoung Kim. "Sexual behavior and sexual satisfaction according to gender in Korean patients with cancer." Korean Journal of Women Health Nursing, Vol. 20, No. 2, 2014, pp. 137-47.
Google Scholar Crossref - Gilbert, Emily, Janette Perz, and Jane M. Ussher. "Talking about sex with health professionals: The experience of people with cancer and their partners." European Journal of Cancer Care, Vol. 25, No. 2, 2016, pp. 280-93.
Google Scholar Crossref - Shin, Nayeon, and Jiyoung Kim. "Experience of chemotherapy in ovarian cancer patients." Asian Oncology Nursing, Vol. 17, No. 3, 2017, pp. 158-69.
Google Scholar Crossref - Broeckel, Jo A., et al. "Sexual functioning in long-term breast cancer survivors treated with adjuvant chemotherapy." Breast Cancer Research and Treatment, Vol. 75, No. 3, 2002, pp. 241-48.
Google Scholar Crossref - Kim, Hae Won, et al. "Gender differences in sexual information needs and relating factors in cancer patients: A cross-sectional survey." International Journal of Environmental Research and Public Health, Vol. 18, No. 7, 2021, p. 3752.
Google Scholar Crossref - Taylor, Sally, et al. "Detecting and discussing sexual problems during chemotherapy for breast cancer." Breast Journal, Vol. 19, No. 5, 2013, pp. 566-67.
Google Scholar Crossref - Otani, Marcia Aparecida Padovan, and Nelson F. Barros. "Communication between healthcare professionals and people undergoing cancer treatment." Brasília Medicalis, Vol. 49, No. 4, 2012, pp. 258-66.
Google Scholar Crossref - Epstein, Ronald M., et al. "Could this be something serious?" Journal of General Internal Medicine, Vol. 22, No. 12, 2007, pp. 1731-39.
Google Scholar Crossref - Svenaeus, Fredrik. "The hermeneutics of medicine and the phenomenology of health: Steps towards a philosophy of medical practice." Springer Science & Business Media, Vol. 5, 2000.
Google Scholar Crossref