Review Article - International Journal of Medical Research & Health Sciences ( 2022) Volume 11, Issue 10
Seroprevalence of TORCH Infections in Pregnant Women with Bad Obstetric History
ST Sahita* and SM DarjiST Sahita, Department of Obstetrics and Gynaecology, Dr. Baba Saheb Ambedkar Medical College and Hospital, New Delhi, India, Email: sanat61@gmail.com
Received: 16-Apr-2022, Manuscript No. IJMRHS-22-61050(PQ); Editor assigned: 18-Apr-2022, Pre QC No. IJMRHS-22-61050; Reviewed: 31-May-2022, QC No. IJMRHS-22-61050(R); Revised: 14-Jun-2022, Manuscript No. IJMRHS-22-61050; Published: 20-Jun-2022
Abstract
Introduction: Primary infection with TORCH complex (Toxoplasma, Rubella, Cytomegalo virus and Herpes Simplex Virus I and II) in pregnant women can lead to adverse outcome like low birth weight to congenital anomalies, sensory neural deafness, mental retardation, cerebral palsy and sometimes to fatal outcomes like abortion and still birth which are initially unapparent or asymptomatic and thus difficult to diagnosed on clinical ground.
Aim: To screen pregnant women with bad obstretic history for TORCH infection to minimize chances of congenital malformation in neonates.
Material and methods: Over a period of one year total 130 serum samples were collected from antenatal women having bad obstetric history attending to tertiary health centre. Samples were screened for IgG antibodies against Toxoplasma, Rubella, Cytomegalo Virus (CMV) by Immuno Comb (EIA) and ELISA Test.
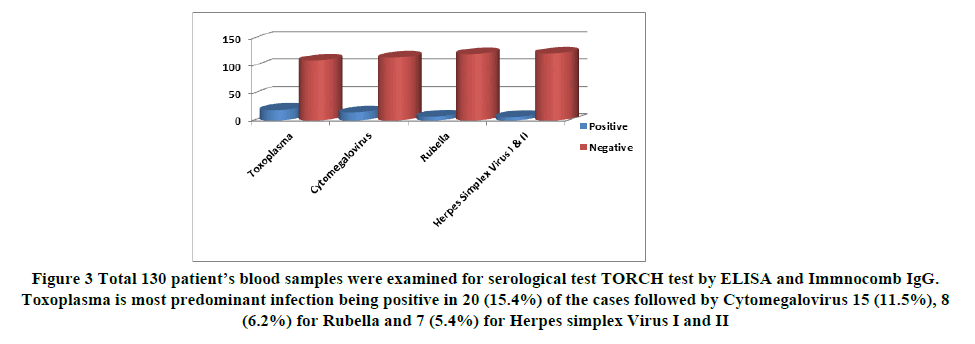
Results: It was found that Toxoplasma is most predominant infection being positive in 20 (15.4%) of the cases followed by 15 (11.5%) for Cytomegalovirus, 8 (6.2%) for Rubella and 7 (5.4%) for Herpes simplex Virus I and II.
Conclusion: This study showed that most of the infections have occurred during young age before or during first pregnancy. Hence all antenatal cases with bad obstetric history should be routinely screened for TORCH as early diagnosis and appropriate intervention will help in proper management of the cases.
Keywords
TORCH, Cogenital infection, ELISA, Immunocomb
Introduction
Predominantly members of TORCH complex microorganisms including Toxoplasma gondii, Rubella, Cytomegalovirus and Herpes simplex virus type I and II, infectious agent leads infection and may enter in to intrauterine circulation at any gestational age. They sometime lead an asymptomatic cause. On other hand, they may encounter us with bad prognosis including miscarriage sterility, congenital malformation and intra uterine fetal loss congenital and prenatal infection represents major causes of permanent disability among children worldwide linked together by acronym TORCH denoting Toxoplasma, Rubella, Cytomegalo virus and Herpes simplex virus [1,2].
Number of human pathogen that cross the placenta and infect the fetus, these agent causes asymptomatic/mild infection in mother while serious consequences in fetus [2].
Maternal infection play a critical role in pregnancy wastage and their occurrence in patient with Bad Obstetric History (BOH) is significant factor [3].
Most of the information on toxoplasma, in India is, on pregnancy wastage [4,5], Rubella and (CMV) Cytomegalovirus are reported to cause damage to the fetus if acquired during pregnancy [6,7].
Toxoplasma gondii is an intracellular protozoon, an agent of parasitic infection, known as Toxoplasmosis. The spectrum of congenital infection extends from asymptomatic finding up to intrauterine fetal loss and may include chorioretinitis hearing squelae, hydrocephalus mental and psychomotor disorder [8].
As gestation weeks progress, risk of vertical transfer increases and the risk of infection leading to more serious malformations decreases [9].
CMV is member of Herpesviridae species, having deoxyribonucleic acid encase in nuclear envelops and may remain as latent stage inside host cells. It can affect 0.5-1% at all live birth and it is the most frequently, seen agent of congenital viral infection, which leads to sensorineural deafness and mental retardation [10].
Human cytomegalovirus (CMV) and Rubella virus are increasingly recognized, as cause of congenital infection. Intrauterine transmission of CMV to baby, can occur irrespective of prior maternal exposure; whereas in rubella, a previous exposure actually prevents the virus from crossing the placenta, by generating protective antibodies.
Rubella virus is single stranded RNA and it is the causative agent of Rubella (Germen measles), in 20-50% of patients who have this infection, it leads an asymptomatic course. In adults and children the disease manifests itself with adenopathy and severe febrile rashes [11].
Following the Rubella vaccination practices, the incidence of rubella has been reduced drastically but the World Heath Origination (WHO) still estimates over 1,00,000 children worldwide are born with congenital rubella syndrome and more so in developing countries [12].
The risk of fetal infection is at highest level, during first 11 weeks and after 36 weeks of gestation if primary infection is contracted within the first 3 months probability of onset of Congenital Rubella Syndrome (CRS) is increases [13].
However diagnosis of acute Toxoplasma, Rubella, CMV and Herpes simplex infection can be established by demonstration of sero-conversation pair sera or demonstration of specific IgM antibodies [14].
The mother is the unusual source of transmission of herpes simplex virus infection during first half of pregnancy is associated with increased frequency of spontaneous abortion, still birth and congenital malformation [1].
However necessity of screening of these infectious agents during pregnancy is detectable issue. The decision to include TORCH groups of microorganism in antenatal screening program in a certain geographic region based on seroprevalence studies conducted at these regions [2].
Materials and Methods
Total 130 antenatal cases with BOH attending to Obstetrics and Gynecology OPD of tertiary care centre during period of one year were included in present study. To diagnose the Toxoplasmosis, Rubella, Cytomegalo virus and Herpes simplex virus I and II Infection blood samples were collected and subjected for the TORCH test.
Blood collection: 2 ml of blood was aseptically collected by venepuncture, in to tube containing clot activator. Blood samples were centrifuged and serum was separated.
Toxoplasma IgG antibody and Cytomegalovirus (CMV) IgG antibody were detected by Smart comb TM (By Fast EIA), Rubella IgG antibody were detected by Orgenics (By fast EIA), whereas HSV I and II IgG antibody were detected by ELISA (Globe Diagnostics Srl ).
EIA method: Each tooth is sensitized by two portion; Upper spot human IgG (Internal Control) and Lower spot inactivated (Toxoplasma, CMV, Rubella) antigen individually. Procedure and interpretation was carried out according to standard kit literature.
ELISA: Procedure and interpretation was carried out according to standard kit literature.
Result
The results show in Figures 1-3 and Tables 1-3.
| Positive | Negative | Total | |
|---|---|---|---|
| Toxoplasma | 20 (15.4%) | 110 (84.6%) | 130 (100%) |
| Cytomegalovirus | 15 (11.5%) | 115 (88.5%) | 130 (100%) |
| Rubella | 8 (6.2%) | 122 (93.8%) | 130 (100%) |
| Herpes Simplex Virus I and II | 7 (5.4%) | 123 (94.6%) | 130 (100%) |
| Mixed infections | Numbers |
|---|---|
| Toxoplasma+Rubella | 07 (Out of 20 toxoplasma IgG positive cases) |
| Cytomegalo virus+Rubella | 4 (Out of 15 cytomegalo virus IgG positive cases) |
| Cytomegalo virus+Herpes simplex virus type II | 01(Out of 15 cytomegalo virus IgG positive cases) |
| Toxoplasma+Cytomegalovirus | 01 (Out of 20 toxoplasma IgG positive cases) |
| Presentation | Toxoplasma +ve | Rubella +ve | CMV +ve | HSV +ve |
|---|---|---|---|---|
| Spontaneous abortion (n=65) | 15 (23.1%) | 7 (10.76%) | 4 (6.15%) | 2 (3.1%) |
| Intrauterine death (n=30) | 2 (66.6%) | 4 (13.3%) | 1 (3.33%) | 1 (3.33%) |
| Congenital malformation (n=20) | 2 (10%) | 5 (25%) | 2 (10%) | 0 |
| Still birth (n=10) | 2 (20%) | 3 (30%) | 1 (10%) | 0 |
| Pre-term labour (n=5) | 2 (40%) | 1 (20%) | 0 | 0 |
Figure 3. Total 130 patient’s blood samples were examined for serological test TORCH test by ELISA and Immnocomb IgG. Toxoplasma is most predominant infection being positive in 20 (15.4%) of the cases followed by Cytomegalovirus 15 (11.5%), 8 (6.2%) for Rubella and 7 (5.4%) for Herpes simplex Virus I and II
Table 2 showing the mixed infections. 7 cases were having Toxoplasma and Rubella infection and 1 case was having Toxoplasma and Cytmegalo viral infections. 04 cases were having cytomegalo viral infection with Rubella and 01 case was having Cytomegalo viral infection with Herpes simples virus type II.
Out of 130 cases undergone for TORCH serological test, 80 showed negative result.
Out of 65 patients with history of spontaneous abortions maximum seropositivity was for the Toxoplasma gondii 15 (23.1%).
Out of 30 cases of intrauterine death maximum seropositivity for Toxoplasma gondii 2 (66.6%) followed by Rubella 4 (13.3%), CMV 1 (3.33%) and HSV 1 (3.33%).
Out of 20 female who gave history of congenital malformation Rubella antibody seropositivity was found most commonly in 5 (25%) cases.
Out of 10 female who gave history of still birth Rubella antibody seropositivity was found most commonly in 3 (30%) cases.
Out of 10 female who gave history of pre-term labour Toxoplasma antibody seropositivity was found most commonly in 2 (40%) cases.
Discussion
Limited data is available regarding the prevalence of TORCH infections among pregnant women in general and particularly in this geographic area. Most of the studies in India have related the seroprevalence to presence of bad obstetric history. As most of the cases remain asymptomatic, determination of maternal antibodies in serum is used to detect infection. Reason for low seroprevalence in present study may be due to test were carried out in case with bad clinical history and cost of TORCH test also influence in investigation rate as it is one of the costlier serological test so patient may be reactant to undergo test procedure.
In present study, Toxoplama IgG antibody was found in 20 (15.4%) samples followed by cytomegalovirus 15 (11.5%), 8 (6.2%) for Rubella and 7 (5.4%) for Herpes simplex virus I and II which is correlating with study done by Shahshi Chopra, et al. December 2004 [14]. According to Susanta Kumar Sahu, et al. April 2019 [15] study carried out at Odisha prevalence of Rubella infections were commonest (68.4%) followed by CMV (57.2%), Toxopalsma (38.3%) HSV infection (21.1%) that again suggests that prevalence of these agents depends upon the geographical distribution.
Out of total 20 (15.4%) IgG antibody positive Toxoplasma cases, 7 cases having Rubella mixed infection and 01 case was having cytomegaloviral mixed infection, while 12 cases were having only Toxoplasma infection.
Out of total 15 positive cases of Cytomegalo virus IgG antibody 05 (33.33%) cases were having mixed infections with Rubella and 01 case was having Herpes simplex type II.
BOH of spontaneous abortion and pre-term labour was very commonly seen in Toxoplasma infection. Intrauterine death, congenital malformation and still birth was very commonly seen with Rubella infection [16].
Limitations
We have detected IgG antibody from single serum sample instead of testing the paired serum samples for titre of IgG antibody after 2 weeks. We could not test for detection of IgM antibodies to exclude recent infection as a part of our study. We also could not do follow up of our cases till their obstetric outcome. This could have given additional information about the actual burden of the infections.
Conclusion
All antenatal cases with BOH should routinely screen for TORCH as early diagnosis and appropriate intervention will help in proper management of these cases.
References
- Turbadkar D, Mathur M, and Rele M. Seroprevalence of TORCH Infection in bad obstetric history. Indian Journal of Medical Microbiology, Vol. 21, No. 2, 2003, pp. 108-110.
[Crossref] [Googlesholar] [Indexed]
- Numan, Onur, et al. TORCH Seroprevelance among patients attending Obstetric Care clinic of Hydarpasa Training and Research Hospital affiliated to Association of Istanbul Northern Anatolia Public Hospitals North Clin Istanb. Northern clinics of Istanbul, Vol. 2, No. 3, 2015, pp. 203
[Crossref] [Googlesholar] [Indexed]
- Mookherjee N, Gogate A and Shah PK. Microbiological evolution of women with bad obstetric history. Indian Journal of Medical Research, Vol. 101, 1995, pp. 103-107.
[Googlesholar] [Indexed]
- Sharma P, et al. (1997) Increasing Toxoplasma seropositivity in women with bad obstetric history and in new born. National Medical Journal of India, Vol. 10, 1997, pp. 65-66.
[Googlesholar] [Indexed]
- Dashore S, Dube S and Pandre V. Maternal toxoplasmosis in cases of pregnancy wastages. Journal of Obstet Gynaecol India, Vol. 41, 1991 pp. 17-20.
- Singla Nidhi, Neerja Jindal, and Aruna Aggarwal. Primary Rubella virus infection prevalence and relationship to pregnancy wastage. Indian journal of Pathology and Microbiology, Vol. 46, No. 4, 2003, pp. 688-689.
[Googlescholar] [Indexed]
- Kapil A, Broors. Primary cytomegalovirus infection in pregnancy and non-pregnant women. Indian Journal of Medical Microbiology, 1992, pp. 1053-1055.
- Kamlesh, Patel, et al. Antenatal detection of IgM and IgG antibodies to T gondii in hospital from central India. International Journal of Health System and Disaster Management, Vol. 2, No. 3, 2014, pp. 133.
- Feldman, Deborah M, Diane Timms, and Adam F. Borgida. Toxoplasmosios, Parvovirus and Cytomegalovirus in pregnancy. Clinics in laboratory medicine, Vol.30, No. 3, 2010, pp. 709-720.
[Crossref] [Googlescholar] [Indexed]
- Gibson, Catherine S, et al. (2006) South Australian cerebral palsy Research group Neurotropic Viruses and cerebral palsy population based case control study. BMJ, Vol. 332, No. 7533, 2006, pp. 76-80.
[Crossref] [Googlescholar] [Indexed]
- Onorato, Ida M, et al. (1985) Epidemiology of CMV infections Recommendations for prevention and control. Reviews of Infectious Diseases, Vol. 7, No. 4, 1985, pp. 479-497.
[Crossref] [Googlescholar] [Indexed]
- Moosavy, Seyed Hamid. Seroprevelance of Rubella Virus in women with spontaneous abortion. American Journal of Infectious Diseases, Vol.7, No.1, 2011, pp. 16-19.
[Crossref] [Googlescholar] [Indexed]
- Vijayalakshmi, Perumalsamy, et al. Rubella serosurveys at three Aravind eye hospital in Tamil Nadu India. Bull World Health Organ, Vol. 82, 2004, pp. 259-264.
- Chopra, Shashi, Usha Arora and Aruna Aggarwal. Prevelence of IgM antibodies to Toxoplasma, Rubella and cytomegalovirus infection during pregnancy. JK Science, Vol. 6, No. 4, 2004, pp. 190-192.
- Sahul, Susanta Kumar, Pradhan, Subrat Kumar and Nayak, Lal Mohan. Study carried out at Odisha, sero prevalence of TORCH infection among pregnant women. International Journal of Community Medicine and Public Health, Vol.6, No. 5, 2019, pp. 2189-294.
- Sen MR, Shukla BN and Banerjee Tuhina. Prevalence of serum antibodies to TORCH infection in and around Varanasi. Journal of Clinical and Diagnostic Research, Vol. 6, No. 9, 2012, pp. 1483.
[Crossref ] [Googlescholar] [Indexed]