Research Article - International Journal of Medical Research & Health Sciences ( 2022) Volume 11, Issue 12
Role of Acoustic Radiation Force Impulse (ARFI) Ultrasound Elastography in the Assessment of Cervical Lymphadenopathy
Priyanka Mattoo*Priyanka Mattoo, Department of Radio-diagnosis, Hamdard Institute of Medical Science and Research, New Delhi, India, Email: drpriyankakantroo@gmail.com
Received: 02-Aug-2022, Manuscript No. IJMRHS-22-71072; Editor assigned: 04-Aug-2022, Pre QC No. IJMRHS-22-71072 (PQ); Reviewed: 18-Aug-2022, QC No. IJMRHS-22-71072; Revised: 19-Oct-2022, Manuscript No. IJMRHS-22-71072 (R); Published: 04-Nov-2022
Abstract
Cervical lymphadenopathy is a common clinical problem across all age groups. There are many causes of lymph node enlargement; cause may vary from infective, reactive, neoplastic, drug induced and many more. Cervical lymphadenopathy often appears as the first clinical sign to an underlying malignancy or infection of head and neck.
Material and methods: A hospital based prospective study was conducted in the department of Radiodiagnosis, Hamdard Institute of Medical Science and Research, New Delhi over a period of one year from April 2021 to May 2022.
Results: A total of 80 patients with clinical diagnosis of cervical lymphadenopathy were included in the study. High resolution ultrasonography and elastography using ARFI imaging was done in all cases. Pathological correlation was done in all cases. Of total 80 patients, 41 lymph nodes were benign while 39 were malignant on FNAC/biopsy correlation.
Discussion: The present study was undertaken to evaluate the role of ARFI acoustic radio focus imaging in characterizing and differentiating benign verses malignant cervical lymph nodes and to determine the accuracy of diagnosis.
Conclusion: USG elastography (ARFI) is promising new technique that noninvasively and objectively complement the ultrasonography in characterization and differentiation of benign and malignant cervical lymph nodes.
Keywords
Cervical lymphadenopathy, Malignant lymphadenopathy, Invasive nature, Ultrasonography
Introduction
Cervical lymphadenopathy is a common clinical problem across all age groups. There are many causes of lymph node enlargement; cause may vary from infective, reactive, neoplastic, drug induced and many more. Cervical lymphadenopathy often appears as the first clinical sign to an underlying malignancy or infection of head and neck. Benign reactive and tubercular lymph nodes have well defined margins, homogenous echo pattern, maintained echogenic fatty hilum and less short axis to long axis diameter ratio and on color Doppler shows central vascularity whereas malignant lymph nodes usually have irregular border, heterogeneous echo pattern, loss of fatty hilum and relatively increased short axis to long axis diameter ratio with peripheral or mixed pattern on Doppler [1].
Ultrasound elastography is a new, rapid and noninvasive imaging technique that measures differences in tissue stiffness in various biological tissues. This technique allows for a qualitative and quantitative assessment of the lesions. There are two types of elastography strain elastography and shear wave elastography [2].
The first is strain elastography imaging, also called free hand real time elastography. It is used to depict relative tissue stiffness or displacement induced by deformation of the tissue. Manual compression is applied by the ultrasound probe and dedicated software is then used to estimate tissue deformation. Harder area shows less displacement and display dark strain images whereas softer tissues shows more displacement and brighter strain images in response to the same force.
The second is shear wave technique including Acoustic Radiation Force Impulse imaging (ARFI) is a technique that can be used to perform both quantitative and qualitative measurements of tissue stiffness and is independent of the amount of tissue compression. Therefore this study was aimed to assess the diagnostic accuracy of ARFI to differentiate benign or malignant cervical lymph nodes. ARFI provides true quantitative estimation of tissue stiffness and does not require external compression [3].
ARFI uses short duration high intensity brief acoustic radiation force (0.003-1 ms) to generate a localized displacement in tissue. This technique utilizes a single transducer to both transmit the radiation force and track the resulting displacement of tissue. To obtain displacement information for a spatial location through ARFI imaging, a reference line is first acquired by a conventional US pulse. Afterward, a radiation force impulse is induced in the same location to create a slight displacement. Thereafter, with the help of conventional US, a series of tracking lines are acquired for monitoring displacement and recovery of the tissue. To observe the recovery of tissue as it returns to its original configuration, approximately 4-6 ms of tracking are required. The repetition of this reference push-track procedure over other spatial locations allows the creation of a 2D image by aligning the displacements of each location in time relative to its pushing pulse. The shear wave velocity is proportional to the tissue stiffness. ARFI technique can be used to evaluate deeper tissues, which is not reachable by external compression. Moreover, it requires slight hardware modification to add an alternative to Doppler mode of M mode [4-8].
Materials and Methods
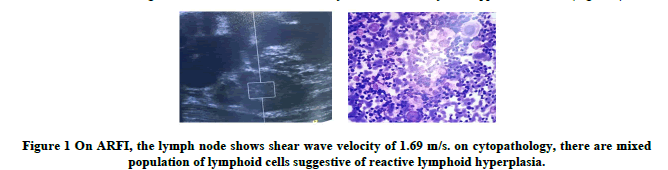
A hospital based prospective study was conducted in the department of radio diagnosis, hamdard institute of medical science and research, New Delhi over a period of one year from April 2021 to May 2022. Patients with clinical diagnosis of cervical lymphadenopathy were included in the study. The informed consent was obtained from all patients before the study. The clinical history and findings of physical examination were noted in all patients. Each patient was evaluated by grey scale ultrasonography and elastography on ultrasound machine Samsung HS 70 A. Biopsy or FNAC correlation was done for all the lesions. The patients were examined in supine position. Grey and color Doppler findings of lymph nodes included were size (in cms), location/side, short axis diameter, short to long axis diameter ratio, margins, echotexture, calcification, fatty hilum, vascularity on Doppler ultrasound (Figure 1).
High resolution grey scale USG was followed by elastography examination in all patients on ultrasound system. The ARFI technique using VTQ (Virtual Touch Quantification) was used to provide quantitative stiffness analysis. The transducer was gently placed in region of interest. After VTQ, in breath hold position; the Region of Interest (ROI) was obtained which is rectangle with dimension of 0.5 cm x o.6 cm and maximum depth of 4.0 cm. ROI was all included into the enlarged lymph node. The calculation of the Shear Wave Velocity (SWVs) was expressed in m/sec.
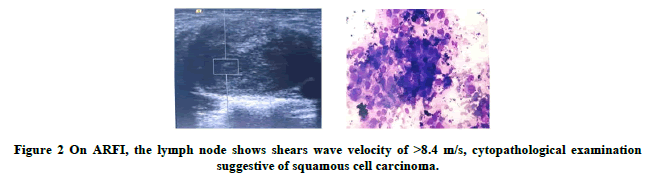
Five SWVs were obtained from the lesions (Figure 2). The median of SWVs value of the lesions was estimated. The observations on high resolution grey scale ultrasonography and ARFI measurements were correlated with histopathological diagnosis on FNAC or biopsy of nodes. The data was entered and analyzed using SPSS software. Continuous variables were assessed using mean, mode and median and categorical data was assessed with Chi square test [9-12].
Results
A total of 80 patients with clinical diagnosis of cervical lymphadenopathy were included in the study. High resolution ultrasonography and elastography using ARFI imaging was done in all cases. Pathological correlation was done in all cases. Of total 80 patients, 41 lymph nodes were benign while 39 were malignant on FNAC/biopsy correlation (Table 1). Among benign cervical lymph nodes, tubercular was the most common (21/41), while squamous cell carcinoma accounted for majority (18/39) of malignant lymph nodes [13].
| Etiology | Number of lymph nodes | Percentage (%) | |
|---|---|---|---|
| Benign | Tubercular lymphadenitis | 41 | 52 |
| 21 | 27 | ||
| Reactive lymphoid hyperplasia | 20 | 25 | |
| Malignant | Squamous cell carcinoma | 39 | 48 |
| 18 | 21 | ||
| Hodgkin’s lymphoma | 8 | 10 | |
| Small cell carcinoma | 6 | 7 | |
| Poorly differentiated carcinoma | 5 | 6 | |
| Papillary carcinoma of thyroid | 1 | 2 | |
| Malignant neurogenic tumor | 1 | 2 | |
| Total | 80 | 100 | |
Table 1 Distribution of cases according to final diagnosis (n=80).
The youngest patient was of 18 years of age and old one was 67 years, mean age was 34.5 years. All patients with benign lymphadenopathy were less than 40 years of age (100%). The maximum number of patients of tubercular lymphadenitis (75.6%), were in the age group of 18-30 years. 33% (13/39) of patients with malignant cervical lymph nodes were more than 40 years (Table 2). The study population consisted of 68% males and 32% females. Both benign (29/41) and malignant (27/39) lymph nodes were prevalent in males.
| Etiology | Number of patients | Age (in years) | ||||
|---|---|---|---|---|---|---|
| = 30 | 31-40 | 41-50 | >50 | |||
| Benign | Tubercular lymphadenitis | 41 | 31 | 10 | 0 | 0 |
| 21 | 17 | 4 | 0 | 0 | ||
| Reactive lymphoid hyperplasia | 20 | 14 | 6 | 0 | 0 | |
| Malignant | 39 | 10 | 12 | 13 | 4 | |
| Squamous cell carcinoma | 18 | 1 | 7 | 9 | 1 | |
| Hodgkin’s lymphoma | 8 | 6 | 2 | 0 | 0 | |
| Small cell carcinoma | 6 | 0 | 0 | 3 | 3 | |
| Poorly differentiated carcinoma | 5 | 3 | 1 | 1 | 0 | |
| Papillary carcinoma of thyroid | 1 | 0 | 1 | 0 | ||
| Malignant neurogenic tumor | 1 | 0 | 1 | 0 | 0 | |
| Total | 80 | 41 | 22 | 13 | 4 | |
Table 2: Age distribution of patients (n=80).
Most of the malignant lymph nodes showed heterogeneous echo pattern on ultrasound. Majority of the malignant lymph nodes showed short axis diameter/long axis diameter ratio >0.5 (35 out of 39 lymph nodes 89.7%). In 37 out of 39 (94.6%) of malignant lymph nodes, fatty hilum was not seen. 43.5% of lymph nodes shows ill-defined border (17 out of 39 lymph nodes). 7 out of 39 malignant (18%) showed calcifications in it. These were squamous cell carcinoma, papillary carcinoma of thyroid and Hodgkin’s lymphomas in FNAC [14-16].
(66.3%) of the malignant lymph nodes (26 out of 39) showed presence of both peripheral and mixed vascular pattern. Most of the benign lymph nodes showed homogenous echo pattern on ultrasound. Majority of the benign lymph nodes showed short axis diameter/long axis diameter ration <0.5 (38 out of 41 lymph nodes). In 32 out of 41 (78%) of benign lymph nodes, fatty hilum was seen. 100 % of benign lymph nodes shows well defined regular border (41 out of 41 lymph nodes). 4 out of 41 benign (4.8%) showed calcifications in it. This was tubercular lymphadenitis on FNAC.
(66.3%) of the malignant lymph nodes (26 out of 39) showed presence of both central/hilar and peripheral vascular pattern. 4% (10 out of 39) shows central/hilar vascularity.
Median shear wave velocity ranged between 1.7 to 8.4 in malignant lymph nodes. Majority of malignant lymph nodes demonstrated a shear wave velocity values less than 8.4 m/sec. 7 out of 39 malignant lymph nodes (20.8%) demonstrated shear wave velocity less than 3 m/sec (Table 3). On FNAC/histopathological analysis, these lymph nodes were found to be Hodgkin lymphoma. The mean SWV value (in m/s) in Hodgkin’s lymphoma (2.04 m/sec) was lower compared to the value in carcinoma (8.15 m/s).
| Malignant lymph nodes | Number | Mean shear wave velocity values (in m/s) | |||
|---|---|---|---|---|---|
| <3 | 3-6 | > 6 | Mean ± SD | ||
| Squamous cell carcinoma | 18 | 0 | 3 | 15 | 7.98 ± 1.38 |
| Hodgkin lymphoma | 8 | 7 | 1 | 0 | 2.04 ± 0.27 |
| Small cell carcinoma | 6 | 0 | 0 | 6 | 8.40 ± 0 |
| Poorly differentiated carcinoma | 5 | 0 | 1 | 4 | 8.40 ± 0 |
| Papillary carcinoma of thyroid | 1 | 0 | 0 | 1 | 8.40 ± 0 |
| Malignant neurogenic tumor | 1 | 0 | 0 | 1 | 8.40 ± 0 |
| Total | 39 | 7 | 5 | 27 | 6.888 ± 2.20 |
Table 3: Median shear wave velocity values in malignant cervical lymph nodes.
Median shear wave velocity ranged between 1.0 to 2.8 in benign lymph nodes. All benign lymph nodes (41/41) demonstrated a shear wave velocity values less than 3 m/sec (Table 4). A classical statistical difference was found between benign and malignant lymph nodes (p<0.0001) respectively (Table 5).
| Benign lymph nodes | Number | Median shear wave velocity in m/s | |||
|---|---|---|---|---|---|
| <3 | 3-6 | >6 | Mean ± SD | ||
| Tubercular lymphadenitis | 21 | 21 | 0 | 0 | 2.05 ± 0.46 |
| Reactive lymphoid hyperplasia | 20 | 20 | 0 | 0 | 2.025 ± 0.44 |
| Total | 41 | 41 | 0 | 0 | 2.042 ± 0.44 |
Table 4: Median shear wave velocity values in benign cervical lymph nodes.
| Shear wave velocity (m/s) | Benign lymph nodes | Malignant lymph nodes |
|---|---|---|
| Mean ± SD | 2.042 ± 0.44 | 6.888 ± 2.706 |
| Median | 2.2 | 8.4 |
| Range | 1.0-2.8 | 1.7-8.4 |
Table 5: Comparison of median shear wave velocity values in benign and malignant cervical lymph nodes.
Discussion
The present study was undertaken to evaluate the role of ARFI acoustic radio focus imaging in characterizing and differentiating benign verses malignant cervical lymph nodes and to determine the accuracy of diagnosis. A total of 80 patients referred to the department of radio diagnosis, Hamdard institute of medical sciences and research, New Delhi with clinical diagnosis of cervical lymphadenopathy were included in the study.
A total of 80 cervical lymph nodes were evaluated of which 39 (48%) were malignant whereas the remaining 41 lymph nodes (52%) were benign. Amongst the malignant lymph nodes, the squamous cell carcinoma was the most common (21%) whereas tubercular lymphadenitis accounted for the majority (27%) of the benign lymph nodes.
The youngest patients in our study were 18 years old and the oldest 67 years, the mean age was 34.5 years. All the patients with benign lymph nodes were less than 40 years (100%) while 33% of the patients with malignant lymph nodes were more than 40 years old. Our study included 56 males and 24 females.
The sonographic characteristic of all the lymph nodes were evaluated with high resolution grey scale ultrasonography and color Doppler imaging. On ultrasound 35 out of 39 malignant lymph nodes (89.7%) were heterogeneous in echo pattern compared to the benign cervical lymph nodes. 89.7% of the malignant lymph nodes showed short axis/long axis diameter ratio >0.5 (35 out of 39 lymph nodes). Majority (37/39) of malignant lymph nodes (94.6%) showed absent fatty hilum. 43.5% (17/39) of the malignant lymph nodes showed ill-defined margins on ultrasound. 66.3% of the malignant lymph nodes (26/39) showed presence of both peripheral and mixed pattern on Doppler USG.
Our findings were in concordance with Dayanand SM et al. who demonstrated most malignant lymph nodes have heterogeneous echo pattern. Fang WT et al. observed short to long axis ratio greater than 0.5 was significantly more frequent in malignant than benign lymph nodes. Khanna R et al. demonstrated that absent hilum was found in 83% of metastatic nodes with higher specificity and sensitivity. Dangore SB et al. observed central flow pattern in benign and peripheral pattern in malignant lymph nodes. Norling R et al. concluded statically significant proportion of malignant lymph nodes had heterogeneous pattern, ill-defined border, spherical shape and peripheral vascularity on color Doppler.
In our study we found that SWVs values were significantly higher in malignant lymph nodes as compared to benign lymph nodes. The SWVs of the malignant lymph nodes in our study were represented by a range of values from 1.7-8.8 m/s and SWVs of the benign lymph nodes ranged from 1.0-2.8 m/s. the cut off value for malignancy was 2.8 m/s. lymph nodes having SWVs greater than 2.8 m/s were considered malignant and less than or equal to 2.8 m/s were benign. Our findings were in agreement with those given by Choi YI where SWVs values for malignant lymph nodes were higher than benign nodes.
Fujiwara T also found that shear wave velocity of reactive lymph nodes was 1.52 ± 0.48 and that of metastatic/ malignant ++ lymph nodes were 2.46 ± 0.75 m/s. Cui XW also demonstrated that shear wave elastography of malignant nodes were homogenously stiffer than benign nodes. Therefore ARFI is found to be superior diagnostic performance over conventional USG and color Doppler in characterization and differentiation of benign and malignant lymph does.
Conclusion
USG elastography (ARFI) is promising new technique that noninvasively and objectively complement the ultrasonography in characterization and differentiation of benign and malignant cervical lymph nodes.
References
- de Jong RJ, et al. Metastatic neck disease: palpation vs. ultrasound examination. Archives of Otolaryngology-Head and Neck Surgery, Vol. 115, No. 6, 1989, pp. 689-690. [Crossref][Googlescholar][Indexed]
- Dayanand SM, Desai R and Reddy PB. Efficiency of ultrasonography in assessing cervical lymph node metastasis in oral carcinoma.National Journal of Maxillofacial Surgery, Vol. 1, No. 2, 2010, pp. 117-122. [Crossref][Googlescholar][Indexed]
- Khanna R, et al. Usefulness of ultrasonography for the evaluation of cervical lymphadenopathy.World Journal of Surgical Oncology, Vol. 9, 2011, pp. 29. [Crossref][Googlescholar][Indexed]
- Jayaraman V, Austin RD and Ramasamy R. The efficacy of colour Doppler ultrasound in differentiating malignant and non-malignant head and neck lymph node enlargement.International Journal of Dental Sciences and Research,Vol. 1, No. 1, 2013, pp. 8-15. [Googlescholar]
- Naik RM, et al. Efficacy of colour Doppler ultrasound in diagnosis of cervical lymphadenopathy.Journal of Maxillofacial and Oral Surgery. Vol. 12, No. 2, 2013, pp. 123-129. [Crossref][Googlescholar][Indexed]
- Genes I, et al. Ultra-sonographic and histopathologic features of cervical lymph nodes metastases.Romanian Journal of Morphology and Embryology, Vol. 55, No. 2, 2014, pp. 369-375.
- Fujiwara T, et al. Acoustic radiation force impulse imaging for reactive and malignant/metastatic cervical lymph nodes.Ultrasound in Medicine and Biology, Vol. 39, No. 7, 2013, pp. 1178-1183. [Crossref][Googlescholar][Indexed]
- Cui XW, et al. New ultrasound techniques for lymph node evaluation.World Journal of Gastroenterology, Vol. 19, No. 30, 2013, pp. 4850-4860. [Crossref][Googlescholar][Indexed]
- Ying M, et al. Review of ultrasonography of malignant neck nodes: grey scale, Doppler, contrast enhancement and elastography.Cancer Imaging, Vol. 13, No. 4, 2014, pp. 658-669. [Crossref][Googlescholar][Indexed]
- Sigrist RM, et al. Ultrasound elastography: Review of techniques and clinical applications.Theranostics, Vol. 7, No. 5, 2017, pp. 1303-1329. [Crossref][Googlescholar][Indexed]
- Sudhir R, et al. Efficacy of acoustic radiation force impulse elastography in differentiation of benign and malignant lymph nodes.Asian Journal of Oncology, Vol. 3, No. 2, 2017, pp. 106-110. [Crossref][Googlescholar]
- Prasad R, Gupta N and Banka A. 2025 too short time to eliminate tuberculosis from India.Lung India, Vol. 34, No. 5, 2017, pp. 409-410. [Crossref][Googlescholar][Indexed]
- Fang WT, et al. Ultrasound surveillance of cervical lymph node metastasis in thoracic esophageal carcinoma.Chinese Journal of Surgery, Vol. 41, No. 7, 2003, pp. 523-525.[Googlescholar][Indexed]
- Dangore SB, Degwekar SS and Bhowate RR. Evaluation of the efficacy of colour Doppler ultrasound in diagnosis of cervical lymphadenopathy.Dento Maxillo Facial Radiology, 2008; Vol. 37, No. 4, 2008, pp. 205-212. [Crossref][Googlescholar][Indexed]
- Norling R, et al. Staging of Cervical Lymph Nodes in Oral Squamous Cell Carcinoma: Adding Ultrasound in Clinically Lymph Node Negative Patients May Improve Diagnostic Work-Up. PLoS One, Vol. 9, No. 3, 2014, pp. e90360. [Crossref][Googlescholar][Indexed]
- Choi YJ, et al. Quantitative shear wave elastography in the evaluation of metastatic cervical lymph nodes.Ultrasound in Medicine and Biology. Vol. 39, No. 6, 2013, pp. 941-949. [Crossref][Googlescholar][Indexed]