Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 5
Right Upper Lobe Collapse in a Healthy Individual, after Endotracheal Tube Extubation, for Elective Procedure
Archana Khokar1*, P N Shivpriya1, Swaraj Sonowal2 and Priyanka Singh12Department of Anaesthesiology, Dr Bhubaneswar Borooh Cancer Institute, Guwahati, Assam, India
Archana Khokar, Department of Anaesthesiology, Atal Bihari Vajpayee Institute of Medical Sciences and Dr Ram Manohar Lohia Hospital, New Delhi, India, Tel: 01123365525, Email: archukhokar89@gmail.com
Received: 21-Apr-2021 Accepted Date: May 18, 2021 ; Published: 25-May-2021, DOI: O
Abstract
Background: Hypoxia is a commonly encountered phenomenon with well-recognized causes in the perioperative period which requires timely diagnosis and management. Case presentation: In this case report we present a healthy adult male patient who had undergone liposuction for bilateral gynecomastia under general anesthesia. The operative surgical procedure and anesthesia were uneventful; however, the patient developed respiratory distress and a sudden decrease in SpO2 after extubation. He required re-intubation and ventilation immediately postoperatively for hypoxia and respiratory distress. On evaluation, he was found to have right upper lobe collapse which may have resulted from bronchospasm after endotracheal tube extubation. The patient was successfully managed with mechanical ventilation and bronchodilators. Conclusion: Greater awareness of this potential complication is needed for timely diagnosis and management.
Keywords
Hypoxia, Bronchospasm, Anaesthesia, Postoperative, Ventilation, Bronchodilator
Introduction
Acute lobar collapse due to reflex bronchoconstriction during endotracheal extubation is a rare entity. Stimulation of the airways by an endotracheal tube, secretions, or by the suction catheter may trigger reflex bronchoconstriction that can result in atelectasis. In this report, we present a healthy adult patient with Right Upper Lobe (RUL) collapse, which developed immediately after endotracheal extubation posted for an elective procedure.
Case Report
A 22-year-old male weighing 70 kg and height of 177 cm, American Society of Anesthesiologists (ASA) grade I scheduled for liposuction for bilateral gynecomastia under general anesthesia. There was no history of any drug allergy or asthma. General physical examinations were within normal limits. On evaluation, blood count, Total Leucocyte Count (TLC), and other biochemistry parameters were in the normal range. The patient’s Electrocardiogram (ECG) and chest X-ray were normal. In the preoperative room, inj. midazolam 1 mg i.v. was given. All the baseline parameters were recorded normal and anesthesia was induced with inj. fentanyl 100 μgm i.v, inj. Propofol 120 mg IV, and muscle relaxant inj. vecuronium 6 mg IV to facilitate endotracheal intubation. The trachea was intubated with an 8.5 mm single-use cuffed Endotracheal Tube (ETT) with a grade I laryngeal view. Tracheal tube position placement was confirmed by auscultation using a stethoscope and ETT fixed at 20 cm with a second black mark at the level of false vocal cords. Intra-operatively, anesthesia was maintained using sevoflurane (end-tidal of 2%) with oxygen (O2): nitrous oxide (N2O) mixture=50:50 and top-up doses of vecuronium. The intraoperative period was uneventful. At the end of the surgical procedure, inhalational anesthetic agents were stopped, and 100% O2 was given to the patient. Injection neostigmine 3.5 mg and inj. Glycopyrrolate 0.7 mg was given to facilitate neuromuscular recovery. Oral suctioning done and the trachea was extubated once the patient started taking regular, adequate, and spontaneous tidal volume breaths.
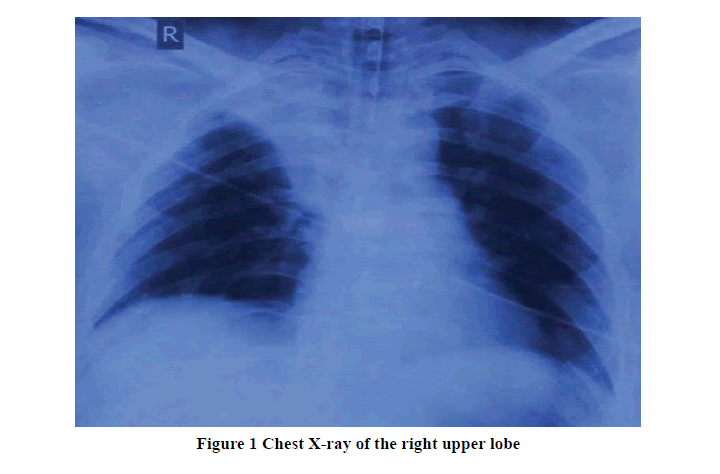
Immediately after the tracheal extubation patient developed respiratory distress, a fall in SpO2, and decreased breath sounds in the right upper zone, for which the patient was re-intubated and put on ventilator support, and shifted to the Intensive Care Unit (ICU) for further management. Arterial Blood Gas (ABG) revealed pH: 7.38, PCO2: 33.6 mmHg, PO2: 101 mmHg, SaO2: 98%, HCO3: 20.1 mmol/L, base excess: -3.5 mmol/L. Fiberoptic bronchoscopy did not show any kind of obstruction or mucus plug in the tracheobronchial tree; however, the patient’s peak airway pressure was high. Chest X-ray showed right upper lobe collapse as shown in Figure 1.
During the ICU stay, the patient received bronchodilator nebulization (salbutamol four puffs every eight hourly, budesonide four puffs twelve hourly, and ipratropium bromide four puffs every twelve hourly) inj. hydrocortisone 100 mg IV, inj. aminophylline 100 mg slow IV then 0.4 mg/kg/hour IV and mechanical ventilation continued with pressure-controlled mode with high peep. The next day, that is post-operative day 1 repeat chest X-ray revealed reexpansion of the collapsed right upper lobe, and the ABG picture was within normal limits. Thereafter, the patient was weaned off from the ventilator and extubated.
Discussion
A telectasis is one of the commonest causes of impaired oxygenation in an anesthetized patient. It may occur during induction, maintenance, or extubation; however, the incidence is very less during extubation [1]. The probable mechanisms of lobar collapse are obstruction of airways, anomalous bronchus, or endobronchial intubation. After complete airway occlusion, gas is trapped in the lung unit distal to the obstruction, and absorption of gas behind the occluded airway may result in a pulmonary collapse [2]. In our patient, fiberoptic bronchoscopy did not reveal any mucous plugs or obstruction due to foreign bodies or any kind of anomaly in the airways. The other cause of atelectasis due to endobronchial intubation was very less, as ETT was appropriately fixed and there were no clinical signs of endobronchial intubation. As the intraoperative period was uneventful so chances of drug-induced bronchospasm are unlikely.
In our patient, the sudden onset of respiratory distress occurred immediately after extubation and the probable mechanism behind this is the reflex bronchoconstriction, which can be triggered by inadvertent extubation and tracheal aspiration, or by the presence of excessive secretion in the airways. Proper suctioning under vision further excludes the tracheal aspiration or excessive secretions induced bronchospasm. Vagally induced bronchoconstriction might be the reason here; however, its incidence is more during induction or maintenance of anesthesia [3-6].
A review of the literature shows that the acute lobar collapse associated with bronchospasm mostly involves the RUL in an anesthetized patient [3,4,6,7]. It has been postulated that the right main-stem bronchus is relatively straight and has almost 90° take-off, which may create a favorable condition for the Bernoulli-effect around the opening of the RUL bronchus [8]. Increased airway resistance due to bronchospasm might have caused rapid laminar flow in the trachea, and therefore directed the airflow toward the right lower and middle lobes, bypassing the RUL bronchus [3,4].
It has been observed that the use of 100% oxygen at the end of general anesthesia facilitates postoperative atelectasis formation by increasing the rate of gas absorption from the un-ventilated alveoli. In our case, we believe that the presence of a high alveolar oxygen tension due to ventilation with 100% oxygen before tracheal extubation might have facilitated bronchospasm-induced atelectasis [7,9].
Conclusion
Bronchospasm may cause acute lobar atelectasis immediately after tracheal extubation. General anesthesia and the use of 100% oxygen may facilitate atelectasis formation during emergence from anesthesia which an anesthesia provider should be aware of.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Westhorpe, R. N., G. L. Ludbrook, and S. C. Helps. "Crisis management during anaesthesia: Bronchospasm." BMJ Quality and Safety, Vol. 14, No. 3, 2005, p. e7.
- Duggan, Michelle, and Brian P. Kavanagh. "Atelectasis in the perioperative patient." Current Opinion in Anesthesiology, Vol. 20, No. 1, 2007, pp. 37-42.
- Sprung, Juraj, Peter K. Schoenwald, and John Hayden. "Bronchospasm and" Reflex Right Upper Lobe Atelectasis"." Anesthesiology, Vol. 89, No. 3, 1998, p. 803.
- Yoo, Kyung Yeon, et al. "Recurrent attacks of post-intubation right upper lobe atelectasis." Acta Anaesthesiologica Taiwanica, Vol. 47, No. 4, 2009, pp. 212-15.
- Liu, Maywin, et al. "Intraoperative bronchospasm induced by stimulation of the vagus nerve." The Journal of the American Society of Anesthesiologists, Vol. 88, No. 6, 1998, pp. 1675-77.
- Kucukguclu, S., N. Gökmen, and F. Ylmaz. "Right lung atelectasis during general anesthesia with laryngeal mask airway." Pediatric Anesthesia, Vol. 16, No. 1, 2006, pp. 93-95.
- Uzman, Sinan, Mehmet Toptaş, and Tumay Uludag Yanaral. "Right upper lobe atelectasis after tracheal extubation in a morbidly obese patient." The American Journal of Case Reports, Vol. 13, 2012, pp. 146-48.
- Moylan, Fergus MB, and Daniel C. Shannon. "Preferential distribution of lobar emphysema and atelectasis in bronchopulmonary dysplasia." Pediatrics, Vol. 63, No. 1, 1979, pp. 130-34.
- Benoît, Zilgia, et al. "The effect of increased FIO2 before tracheal extubation on postoperative atelectasis." Anesthesia and Analgesia, Vol. 95, No. 6, 2002, pp. 1777-81.