Research - International Journal of Medical Research & Health Sciences ( 2023) Volume 12, Issue 3
Rhino-Orbito-Cerebral Mucormycosis and its Imaging Spectrum a Prospective Observational and Analytical Study in the Setting of Covid 19 Pandemic in a Tertiary Care Centre, AP, India
Bomidi Sudha Rani1*, P. Bujjibabu1, M. Umamaheswar Rao2 and Praveen32Department of Radiodiagnosis, Rajiv Gandhi Institute of Medical Sciences, Srikakulam, India
3Department of Microbiology, Andhra Medical College, King George Hospital, Visakhapatnam, India
Bomidi Sudha Rani, Department of Radiodiagnosis, Andhra Medical College, KGH, Visakhapatnam, India, Email: radiologysudha@gmail.com
Received: 02-Mar-2023, Manuscript No. ijmrhs-23-90584; Editor assigned: 04-Mar-2023, Pre QC No. ijmrhs-23-90584(PQ); Reviewed: 05-Mar-2023, QC No. ijmrhs-23-90584(Q); Revised: 22-Mar-2023, Manuscript No. ijmrhs-23-90584(R); Published: 30-Mar-2023
Abstract
Background: Rhino-Orbital-Cerebral Mucormycosis (ROCM) is a potentially fatal fungal infection that commonly affects diabetic and other immunocompromised patients. Necrotizing and Angioinvasive features of this class of pathogenic fungi facilitate the spread from sinuses into orbit and the brain with devastating consequences. Early diagnosis and timely intervention are key to successful treatment. Aims and Objectives: This article aims to interpret the findings on CT and MRI in ROCM. The primary objective of this study is to enumerate the imaging findings of all patients presented with Rhino orbital cerebral mucormycosis at various stages and to describe the management algorithm. The secondary objective is to follow up on aggressive cases after successful therapy. Materials and Methods: This prospective observational descriptive and analytical study was conducted in the Department of Radiodiagnosis, Andhra Medical College, King George Hospital, Visakhapatnam, India from April 2021 to august 2021 for 5 months. Reviewed 100 patients of the adult age group with strong clinical complaints suggestive of ROCM. Few patients are further followed up for another 6-month to 1-year period wherever necessary. Variables: Age, sex, diabetes, steroid use, O2 supplementation. Results: We present 100 cases of ROCM to emphasize the effectiveness of Magnetic Resonance Imaging (MRI) in the diagnosis of this potentially fatal form of mucormycosis. A Favorable outcome was achieved with surgical debridement and prolonged Amphotericin therapy. CT and MR imaging of 100 patients showed predominantly pan-sinus involvement (67%). Extension to the orbit and face (66%) preceded involvement of the deep skull base (62%) and brain (40%). Ontrast-Enhanced Computed Tomography (CECT) showed minimally enhancing hypodense soft tissue thickening as the predominant finding in involved areas, while MRI showed T2 hypointense with post-obstructive T2 hyperintense changes/ soft tissue thickening and heterogeneous post-contrast enhancement as the main finding. Bone erosion was seen less often (40%), with the rest of the patients (60%) showing extra sinus extension across grossly intact appearing bones on imaging. Conclusion: CT and MRI show a spectrum of findings in Rhino orbital cerebral mucormycosis. Imaging plays a major role in assessing the extent of involvement and complications. DWI may add specificity to the diagnosis by showing restricted diffusion in the path of fungal invasion. Thus Magnetic resonance imaging is the effective imaging modality for the diagnosis of ROCM, for the staging of the disease, for patient management, and follow-up. Recommendations: Aiming for better glycemic control in those with diabetes, appropriate use of systemic corticosteroids, and prevention of unnecessary use of antibiotics, antifungals, and other immunomodulators. Infection Prevention and Control (IPC) program measures at the facility level are essential to prevent the environmental spread of this pathogen.
Keywords
Magnetic Resonance Imaging (MRI), Rhino-Orbital-Cerebral Mucormycosis (ROCM), Angioinvasive Mucormycosis, Sinonasal Disease (SND)
Introduction
The purpose of this study is to confirm the probable ROCM at the earliest and categorize it into different stages and interpret based on the imaging findings that help in clinical decision-making and patient management. Mucormycosis is an acute and uncommon aggressive potentially lethal, angioinvasive fungal infection predisposed by diabetes mellitus, corticosteroids and immunosuppressive drugs, primary or secondary immunodeficiency, hematological malignancies, and hematological stem cell transplantation, solid organ malignancies and solid organ transplantation, iron overload, etc [1]. The disease originates in the sinonasal mucosae and extends rapidly to neighboring structures, including the orbit and sometimes the brain. ROCM is characterized by very high residual morbidity and mortality due to the angioinvasive property of the fungus, which causes vascular occlusion resulting in extensive tissue necrosis. The increasing incidence of Rhino-Orbito-Cerebral Mucormycosis (ROCM) in the setting of COVID-19 in India and elsewhere has become a matter of immediate concern [2-4].
ROCM being a rapidly progressive disease, even a slight delay in the diagnosis or appropriate management can have devastating implications on patient survival [5]. However, the outcome can be optimized by early diagnosis prompted by awareness of warning symptoms and signs and a high index of clinical suspicion, confirmation of diagnosis by appropriate modalities, and initiation of aggressive medical and surgical treatment by a multidisciplinary team [1,5].
The clinical presentation in the early stages is typical with fever, headache, facial pain, nasal discharge, and nasal obstruction. After infection of the nasal cavity and paranasal sinuses, the fungi cause a necrotizing vasculitis that extends rapidly into the deep face, orbits, cranial cavity, and brain through skull base partitions and foramina [2]. ROCM can be categorized clinically as Possible, Probable, and Proven. A patient who has symptoms and signs of ROCM in the clinical setting of concurrent or recently (<6 weeks) treated COVID-19, diabetes mellitus, use of systemic corticosteroids and tocilizumab, mechanical ventilation, or supplemental oxygen is considered as Possible ROCM. When the clinical symptoms and signs are supported by diagnostic nasal endoscopy findings, or contrast enhanced MRI or CT scan, the patient is considered as probable ROCM. Clinico-radiological features, coupled with microbiological confirmation on direct microscopy or culture or histopathology with special stains or molecular diagnostics are essential to categorize a patient as having proven ROCM [6].
As the critical care teams start receiving and caring for the increasing number of ROCM patients in the setting of COVID-19, a working staging system may help triage these patients and customize their care. Optimizing the outcome, minimizing the morbidity, and improving the survival in ROCM needs collaborative action and rapid response by a multi-disciplinary team comprising experts in diagnosis (radiology, microbiology, pathology, molecular biology), and medical (infectious disease, neurology, critical care) and surgical (otorhinolaryngology, ophthalmology, neurosurgery) care [7,8].
Early imaging helps assess the extent of involvement of this lethal disease which requires prompt and aggressive treatment. We studied the imaging findings in all patients presented to our hospital who have been diagnosed with Rhino orbital cerebral mucormycosis at various stages of the disease, we also studied the imaging findings of those patients who reported for follow-up after successful therapy.
Inclusion Criteria
• All adult age groups.
• Both covid positive and negative.
• Post covid management patients.
Exclusion Criteria
• Paediatric age group.
• Those who are not willing to participate in this study.
• Patients who left against medical advice.
Materials and Methods
CT scan was performed on a GE machine using a routine CT Paranasal Sinus (PNS) protocol with 130 kVP and 150 mA-220 mA tube current. Intravenous contrast medium (low osmolar, non-ionic, 300 mg/mL iodine content) was used routinely at a dose of 1 ml/kg administered by a pressure injector. Conventional MR Brain with PNS and orbits imaging including axial, coronal, and sagittal T1 weighted (TR/TE 40/12 ms), T2-weighted images (TR/TE 4000/ 100 ms) DWI, GRE/SWI, and fat-suppressed post-contrast T1 weighted images, were acquired. MRI imaging was performed using a 1.5 T GE machine. Image analysis was done by radiologists to look for sites and extent of involvement, signal characteristics, and complications.
Image interpretation: The sinuses showing opacification on CT or MRI were recorded in each case. The appearance on plain T1 and T2 images were documented. DWI, GRE, and SWI were also employed routinely. On post-contrast CT and MRI, the type of contrast enhancement and involvement of any extra sinus structures including orbit, face, pterygopalatine fossa, brain, and cavernous sinus were noted. The Presence of bone involvement was evaluated on the CT. Any complications like arterial thrombosis were noted on CT and MRI. Fat stranding and soft tissue extension similar in appearance to the intrasinus soft tissue were taken as evidence of orbital, retroantral, and pterygopalatine region involvement. Orbital cellulitis was seen as stranding in the retrobulbar fat. Cavernous sinus and internal carotid artery involvement were seen as a thickening and non-enhancement on post-contrast scans with the presence of abnormal surrounding soft tissue. Patients with intracranial extension were evaluated for dural enhancement, presence of extradural collections, infarcts, cerebritis, and intracerebral abscess. As patients presented to us at various stages of the disease, the patients in the study were divided into three groups based on the extent of regional involvement according to the classification suggested [4].
Results
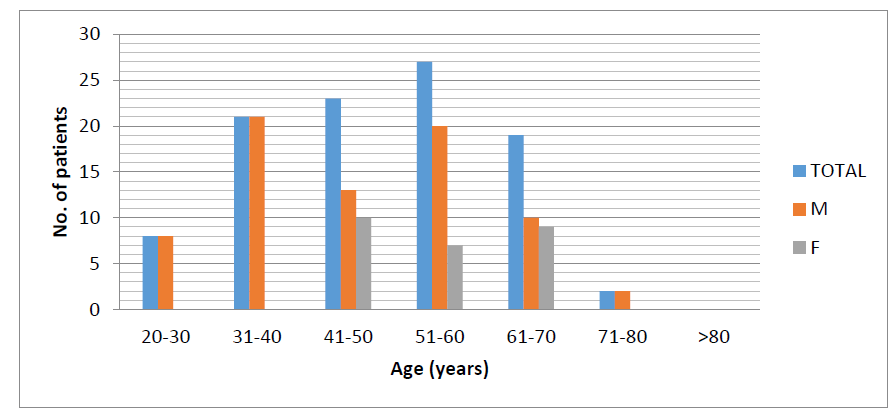
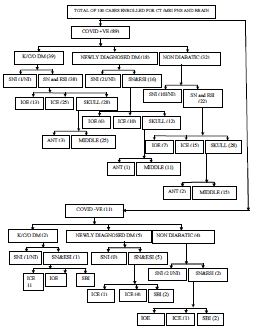
A total of 100 patients presented to the Department of Radiodiagnosis have enrolled in the study with Rhino orbital cerebral mucormycosis. We have done MRIs for all the patients. Few patients were taken for CT to look for underlying bone destruction. All patients underwent contrast-enhanced MRI, and histopathology confirmation was identified. Our study group comprised 74 males and 26 females with ages ranging from 23 years to 78 years. Mean49.9 years (Table 1, Figure A). The majority of patients (83.7%) were aged over 40 years, with those aged 40 years60 years (55%) being most affected. 41 patients (41%) had a history of uncontrolled diabetes, and 23 patients were newly diagnosed with diabetes after steroid usage. 89 patients are Covid positive and 11 are covid negative. 62 used iv steroids and 63 patients used O2 supplementation (Table 2). The clinical symptoms reported in our series were tabulated in Table 3.
| Adult age group | No. | % | M/F ratio |
|---|---|---|---|
| 20 years-30 years | 8 | 8% | 08:00 |
| 31 years-40 years | 21 | 21% | 21:00 |
| 41 years-50 years | 23 | 23% | 13:10 |
| 51 years-60 years | 27 | 27% | 20:07 |
| 61 years-70 years | 19 | 19% | 10:09 |
| 71 years-80 years | 2 | 2% | 02:00 |
| >80 years | 0 | 0 | 0 |
| Total patients (N=100) | No. | % |
|---|---|---|
| Covid positive with or without other risk factors | 89 | 89% |
| Covid negative with comorbidities/other risk factors | 11 | 11% |
| O2 supplementation | 63 | 63% |
| Uncontrolled diabetes | 65 | 65% |
| I.V Steroid usage | 62 | 62% |
| Chronic kidney disease | 6 | 6%SSS |
| Post pulmonary tuberculosis | 0 | 0 |
| Other2ndimmunodeficiency/Neutropenia/Advanced AIDS | 0 | 0 |
| Clinical symptom | No. | % |
|---|---|---|
| Headache | 80 | 80% |
| Nasal discharge and blockage | 85 | 85% |
| Facial swelling | 53 | 53% |
| Facial pain | 62 | 62% |
| Visual disturbances | 66 | 66% |
| Proptosis | 40 | 40% |
| Loosening of teeth | 9 | 9% |
In our study Imaging findings are categorized as isolated Sinonasal and Sinonasal with extra sinus involvement. In the majority of patients with isolated Sinonasal disease, pansinusitis is the most common presentation (67%).
On CT three types of contrast enhancement were seen, with heterogenous enhancement being the most common form. Other types included low-density opacification with no post-contrast enhancement and mild enhancement. In cases with non-enhancing opacification of sinuses, the presence of periantral, facial and orbital fat stranding and hypodense soft tissue extension indicated the aggressive nature of the infection. On MRI signal intensity of the sinonasal and extra sinus involving lesions are predominantly T2 hypointense with postobstructive T2 hyperintense changes. On T1WI the lesions are mostly iso to hypointense.
Enhancement of the lesions and pattern of extension of infection were best delineated on fat-suppressed postgadolinium images. The black turbinate sign described by Safder et al. to be a feature of early nasal mucormycosis was found only in 2 patients with available post-contrast MRI [5]. Details of extra sinus extension including the type of involvement are given in Table 4. Based on the classification by Rupa et al. most of the patients (56%) appeared to have advanced disease (stage 3) at presentation. Further details regarding the type of extension are given in Table 5.
| Site of involvement | No | % |
|---|---|---|
| Isolated sinonasal involvement | 16 | 16% |
| Extrasinus extension from SND | 84 | 84% |
| Orbital involvement and extensions | ||
| Focal/diffuse orbital inflammation | 66 | 66% |
| Optic nerve involvement | 11 | 11% |
| Orbital apex involvement | 50 | 50% |
| Extending into the superior orbital fissure | ||
| Cavernous sinus involvement | 36 | 36% |
| ICA involvement | 15 | 15% |
| Extending into the inferior orbital fissure | ||
| Pterygopalatine fossa involvement | 50 | 50% |
| Bone involvement | ||
| Neurocranium /calvaria/Skull base involvement | 62 | 62% |
| Viscerocranium/facial bones | ||
| Alveolar process of maxilla | 9 | 9% |
| Hard palate | 5 | 5% |
| Intracerebral involvement | ||
| Late Cerebritis/Abscess | 38 | 38% |
| Epidural collection | 17 | 17% |
| Infarcts | 16 | 16% |
| Pachymeningeal thickening and enhancement | 9 | 9% |
| Subperiosteal collection | 5 | 5% |
| Stage | Areas involved | No | % | Management | Survival rate |
|---|---|---|---|---|---|
| Stage 1 | Nose and paranasal sinuses alone | 16 | 16% | FESS and antifungals | 99% |
| Stage 2 | Paranasal sinuses and immediate adjacent areas which are surgically resectable | 28 | 28% | Surgical resection/surgical debridement and local/parenteral amphotericin B | 99% |
| Stage 3 | Intracranial Extention/ pterygopalatine fossa | 56 | 56% | Partially/non-resectable | 90% |
Chronic persistent form of bone involvement (68 cases) was seen in the surrounding bones of the involved sinuses predominantly frontal bone. The involved bones showed variable expansion, sclerosis, erosions, and irregular lytic destruction on follow-up imaging.
A few ROCM case scenarios with sinonasal and extra sinus involvement and also cases with intracranial and skull base extension are represented with the figures below.
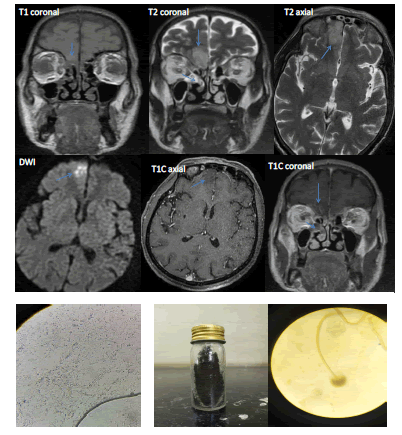
Case Studies 1
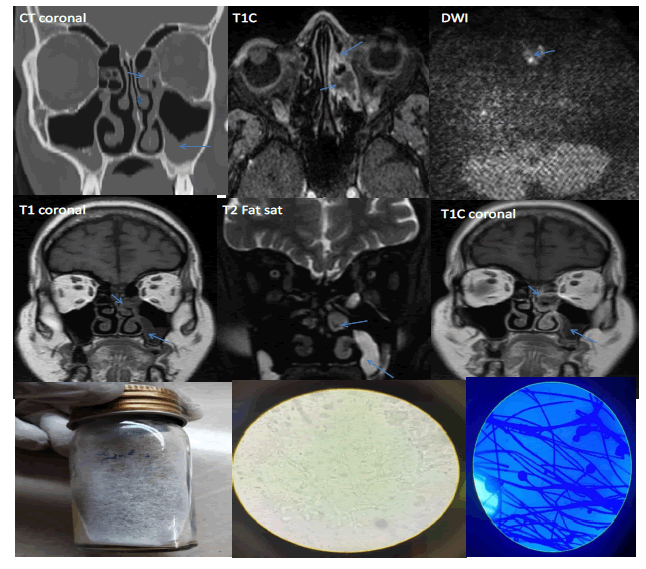
Stage 1 Early Aute Rhinosinusitis (Figure 1).
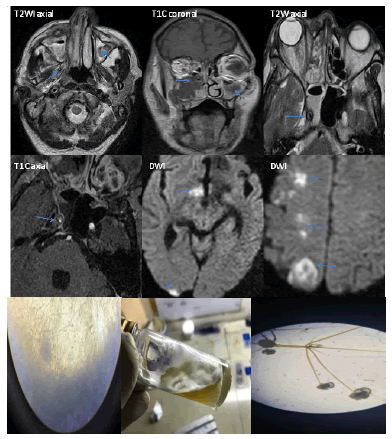
Figure 1. 49 year old post covid male patient newly diagnosed with diabetes after I.V. Steroids came with watering of the eye, pain, and, headache. CT and MRI showed sinonasal involvement (SNI) that is T1 hypo and T2 altered/mixed signal intensity with central nonenhancing necrotic component on T1 contrast. The lesion is predominantly involving nasal mucosa, middle turbinate, middle ethmoid sinus region, and showing diffusion restriction. Inflammatory narrowing of the Left nasolacrimal duct is seen as well. No e/o Extra Sinus Involvement (ESI) /Intra-Orbital Extension (IOE) /Intracranial Extension (ICE). Antifungal treatment is given. FESS was done. Histopathology/culture revealed mucor-positive. The patient recovered well. Follow-up is done. No recurrence. Microscopy: potassium hydroxide (KOH) 10% mount shows ribbon-shaped broad aseptate hyphae. Culture: Saborauds Dextrose Agar (SDA) with fluffy cottony white colonies. Lacto Phenol Cotton Blue (LPCB) shows hyphae suggestive of Mucor spp
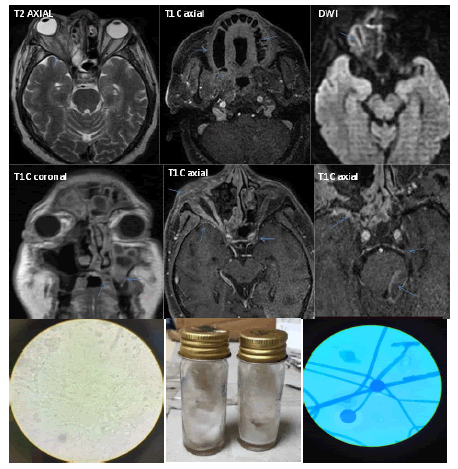
Case Studies 2
Stage 1 Acute Rhinosinusitis (Figure 2).
Figure 2. 62 year old covid positive known diabetic male patient presented with brown-colored sputum. On imaging, there is sinonasal disease on both sides with T1 hyper intense signal which is hypo intense on T2 and showing blooming on GRE suggestive of acute bleed/ hyphae/inspissated secretions. T2 hyperintense post obstructive changes were also seen in bilateral maxillary sinuses Antifungal treatment is given FESS was done and a biopsy revealed Aspergillus niger. Recovered well and follow-up done. No recurrence. On culture, there is Black, yellow, and green-colored velvety growth of Aspergillus on SDA. LPCB showing hyphae suggestive of Aspergillus. Gram staining showing budding yeast-Candida sp
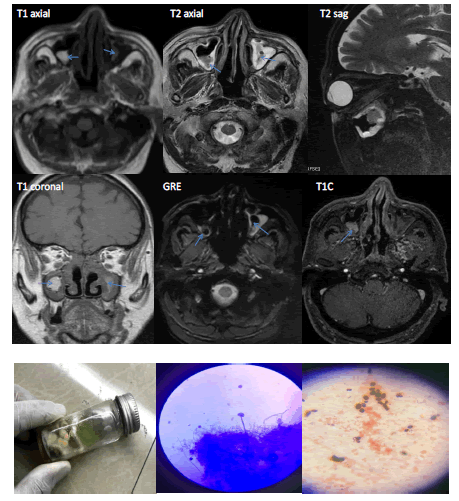
Case 3
Stage 2 Fulminant ROM (Figure 3)
Figure 3. A 63 year/male patient who is covid negative came with co morbidities and was newly diagnosed with diabetes after taking I.V. steroids. MRI showing sinonasal involvement predominantly on right side with post obstructive changes. Right Nasal mucosa, middle turbinate, ethmoid and maxillary sinus are predominantly involved with blockage of OMU. Extrasinus involvement was similar in appearance to intrasinus soft tissue and was seen extending into the right inferiomedial orbit with inflamed extraocular muscles. The colonized invasive fungal non-enhancing necrotic component is seen extending further into retro/periantral, premaxillary region, and pterygopalatine fossa eroding the underlying maxillary antrum and is showing blooming on GRE with subtle diffusion restriction. No intracranial extension. Culture on SDA showing black-colored velvety growth of Aspergillus niger. LPCB conforming Aspergillus niger. Patient expired with co morbidities
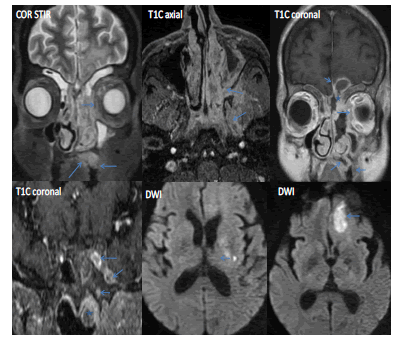
Case Studies 4
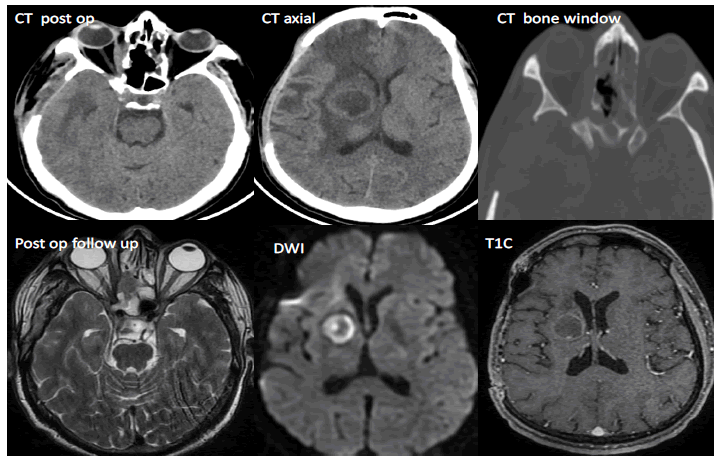
Stage 3 ROCM with early cerebritis (Figure 4)
Figure 4. A 61-year-old male patient covid positive and known diabetic was on steroid treatment presented with severe headache, pain in both eyes, swelling, and shortness of breath. MRI showing rhino sinusitis and intracerebral extension through the roof of right orbit and ethmoid sinus which appears as non-enhancing T2/FLAIR hyperintensity in the right basifrontal region that has low ADC value/ true diffusion restriction. Features suggestive of early cerebritis. Patient expired with uncontrolled diabetes. KOH mount shows septate hyphae. Culture on SDA showing black-colored growth, LPCB conforming Aspergillus niger
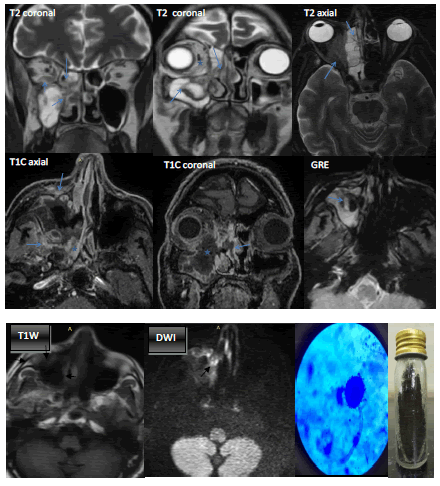
Case 5
Stage 3 ROCM with basifrontal abscess (Figure 5)
Figure 5. A 61-year-old female covid-positive patient known diabetic was on oxygen supplementation and steroids presented with headache, left eye proptosis, and blurring of vision. Images showing rhinosinusitis with left orbital extension eroding the medial wall of the orbit and involving the intra and extra-conal compartments, lacrimal duct, lachrymal sac, and left orbital apex. Further, the lesion is extending posteriorly into the cavernous sinus through SOF, pterygopalatine fossa through IOF, and other skull base foramina like the vidian canal and foramen rotundum. The Peri/Retro antral region, the infratemporal fossa and nasopharyngeal extension is also noticed. There is involvement of viscerocranium causing osteomyelitis of the hard palate and alveolar process of the maxilla. Intracranial extension is seen through ethmoid roof/cribriform plate causing left basi frontal abscess i.e pyogenic as there are no intracavitary projections and the core is showing diffusion restriction, due to secondary bacterial infection. Adjacent dural enhancement is seen as well. Distal left ICA showing thrombus causing left capsuloganglionic region infarcts. The fungal culture reported as sterile. Patient expired after post-op craniotomy
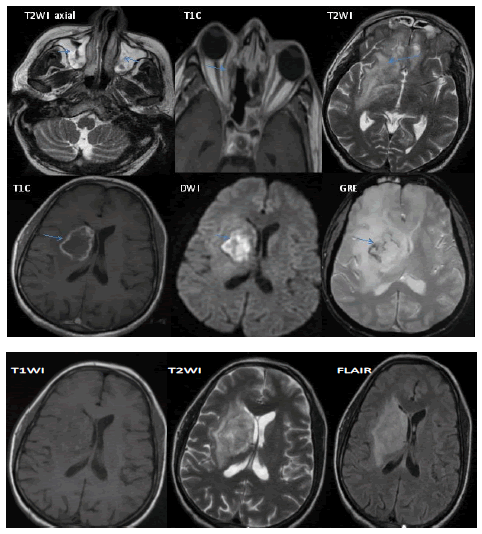
Case 6
Stage 3 ROCM with right cerebral abscess (Figure 6)
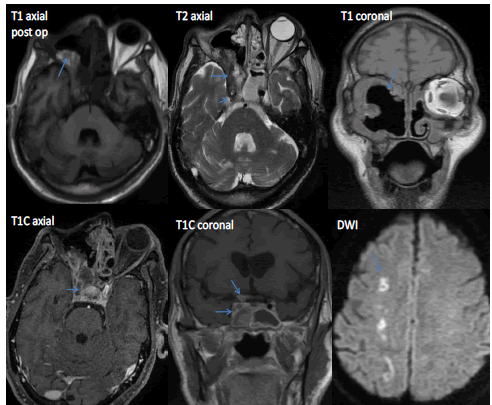
Figure 6. A 42-year-old covid positive patient newly diagnosed as diabetes after i.v steroids presented with headache and right eye pain. MRI showing rhinosinusitis, extending into medial extraconal compartment of right orbit sparing orbital apex. Bilateral basifrontal late cerebritis features and right capsuloganglionic region mycotic abscess are well seen with irregular crenated margins and enhancing wall with non-enhancing intracavitary papillary projections that are showing diffusion restriction. T2 Hyperintense central core is not enhancing. Gradient images showing areas of blooming. Functional Endoscopic Sinus Surgery (FESS) and Craniotomy are done
Post FESS/ extensive surgical debridement/antifungal agents and craniotomy follow-up scan (Figure 7). Post-craniotomy follow-up after 6 months (Figure 8).
Case 7
Stage 3 ROCM with anterior skull base involvement-acute left frontal osteomyelitis (Figure 9).
Figure 9. A 36-year-old covid-positive known diabetic patient with no h/o treatment with i.v steroids/oxygen supplementation. presented with left frontal swelling. MRI and CT Images are showing left ethmoidal sinusitis eroding lamina papyracea & extending into the medial extraconal compartment of the left orbit. T2 hyperintense concentric mucosal thickening is seen in bilateral maxillary sinuses, Right ethmoidal, and sphenoidal sinuses. There is T2 hyperintense left frontal sinusitis with intense enhancement on contrast and underlying aggressive bone destruction s/o left frontal bone osteomyelitis. This lesion is extending and involves adjacent bones like the greater wing of the sphenoid, zygoma, and soft tissues like periorbital/preseptal region /temporalis muscle and subcutaneous planes causing subperiosteal abscess as well. T1 hypointense and stir hyperintensity in the above lesion denotes early involvement of frontal bone osteomyelitis with intracranial spread (minimal epidural abscess) and adjacent dural enhancement (fungal patchy meningitis). No e/o adjacent venous thrombosis. The patient underwent surgery and is on follow-up. (Pott puffy tumor is a rare complication of sinusitis characterized by osteomyelitis of the frontal bone with subperiosteal abscess presenting as frontal swelling
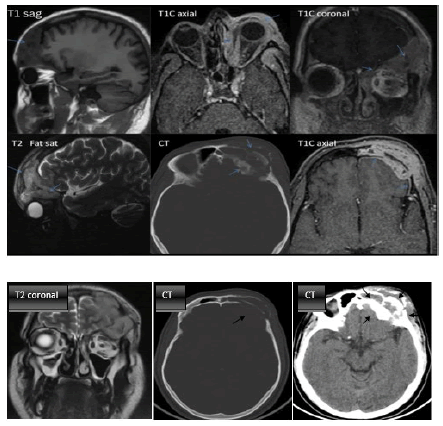
Case 8
Stage 3 ROCM with neurovascular spread- optic nerve infarction, intracranial abscess (Figure 10).
Figure 10. A 41-year-old post covid known diabetic patient having h/o treatment with i.v. steroids and oxygen supplementation presented with loosening of upper teeth on both sides and proptosis of the right eye with the painful loss of vision. Images showing sinonasal and extra sinus involvement such as diffuse orbital inflammation. The right optic nerve showing diffusion restriction, suggestive of optic nerve infarction. There is involvement of viscerocranium such as hard palate and superior alveolar process of maxilla with loss of teeth on the right side. Focal adjacent dural enhancement is seen on the right anterior medial aspect of temporal lobe with the underlying altered signal intensity of the greater wing of the sphenoid. Through orbital apex on the left side the lesion is extending into the cavernous sinus and causing perineural spread resulting in brainstem and posterior fossa abscess. Biopsy specimen of optic nerve showed ribbon-like broad hyphae on KOH mount, SDA showing Mucor growth, and LPCB revealed Mucor. Patient is expired
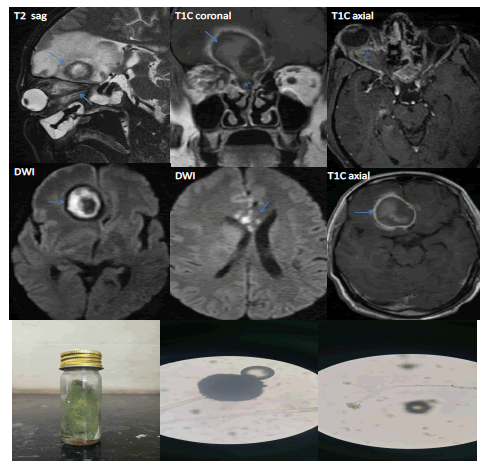
Case 9
Stage 3 ROCM with right basifrontal abscess and ACA territory acute infarct and right optic nerve compression/invasion (Figure 11).
Figure 11. A 64-year-old post covid newly diagnosed diabetic patient presented with right eye proptosis and severe headache. MRI showing sinonasal diasease and intraorbital extension through erosion of the medial wall of the right orbit and right nasolacrimal duct. There is diffuse orbital inflammation involving intraconal and medial extraconal compartments of right eye encasing and compressing optic nerve showing altered signal intensity/optic neuritis. Intracranial extension of invasive sinusitis into frontal lobe is seen through ethmoid roof on right side forming an abscess and on T1C there is rim enhancement. DWI showing peripheral true diffusion restriction of intracavitary projections but not the core. Suggestive of mycotic abscess extending into capsuloganglionic region as well. The abscess is showing mass effect and compressing/invading adjacent ACA and eventually causing acute infarcts in the genu of the corpus callosum. Orbital exenteration done. Biopsy specimen is positive for fungal elements. On SDA green velvety growth was produced. LPCB (scotch tape method) showing Aspergillus niger and Aspergillus flavus. Patient expired with co morbidities
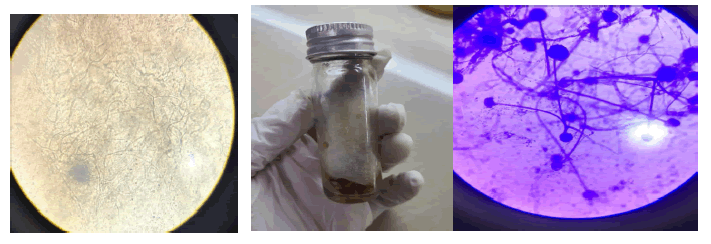
Case 10
Stage 3 Angioinvasive ROCM with orbital apex syndrome and acute infarcts (Figure 12).
Figure 12. 68 year old post covid male patient who is a known diabetic treated with i.v steroids and oxygen supplementation came with right eye blurring of vision. Bilateral Acute invasive fungal sinusitis showing non-enhancing hypointense signal and extending into right orbital apex, cavernous sinus and encasing/invading cavernous portion of ICA causing partial thrombus/obstructionn leading to acute infarcts showing diffusion restriction in Right MCA territory. Biopsy specimen on KOH mount showing positive for fungal elements. SDA with fungal growth. LPCB revealed Rhizopus along with rhizoids
Post-op follow up
Right ICA Thrombosis. Optic neuritis. Right parietal infarcts. Patient (Figure 13).
Flow Chart
Discussion
Mucormycosis, also known as zygomycosis and phycomycosis, was first described by Paulltauf in 1885. Even though it can involve different body organs the most common type is the rhino orbital cerebral form [9]. Phycomycetes are ubiquitous fungi occurring in soil, air, skin, body orifices, manure, spoiled food, and dust [10,11]. Inoculation occurs by inhalation, when spores reach the nasal cavity and/or nasopharynx. The fungus may then spread to the paranasal sinuses and subsequently to the orbit, meninges, and brain by direct extension [12]. Orbital involvement results from spreading through the nasolacrimal duct and medial orbital wall. Such invasion is facilitated by the thinness of the lamina papyracea, congenital dehiscence often presents along the medial wall, and the perforations of the medial wall by arteries and veins [13,14].
Generally, the presenting symptoms are low-grade fever, cephalgia, sinusitis, facial swelling, nasal discharge, and nasal obstruction, After infection of the nasal cavity and paranasal sinuses, the fungi cause a necrotizing vasculitis that extends rapidly into deep face, orbits, cranial cavity, and brain through skull base partitions and foramina causing orbital apex syndrome with blurred vision, and cranial palsies from cavernous sinus involvement [2,15-20 in which blindness is a much later finding [21].
Mucormycosis invades the walls of the blood vessels resulting in vascular occlusion, thrombosis, and infarction, as well as dissemination to the central nervous system from the primary focus [5,15,16]. Spread to the brain may occur via the orbital apex, orbital vessels/perineural spread, or via the cribriform plate of the ethmoid/frontal bone [17]. Our study group comprised 74 males and 26 females. The majority of patients were aged over 40 years, with those aged 40 years-60 years being most affected. Common presentation being nasal discharge. 41 patients had a history of uncontrolled diabetes, and 23 patients were newly diagnosed with diabetes after steroid usage. All patients are Covid positive except in 11 cases. 62 used i.v. steroids and 63 patients used O2 supplementation. In our study, we found that MRI signal intensity of the sinonasal and extra sinus involving lesions are predominantly T2 hypointense with postobstructive T2 hyperintense changes. On T1WI the lesions are mostly iso to hypointense. However there are few hyperintese areas within showing blooming on GRE and subtle diffusion restriction probably due to acute bleed/hyphae/inspissated secretions (Figure 2 and Figure 3).
In our study, only Sinonasal involvement is seen in 16 cases. Among these, 4 cases showing T2 hypointense signal and only in 2 cases black turbinate/black mucosa sign is well appreciated on post-contrast images (Figure 1). These are post-covid patients having uncontrolled diabetes and other comorbidities.
After the administration of gadolinium, the lesions showed variable enhancement patterns ranging from homogeneous to heterogenous or non-enhancing. Contrast-enhanced T1-weighted images help in delineating theintracranial spread when meningeal enhancement is present as well as in identifying invasion of the cavernous portion of the internal carotid artery by the disease. This had been previously described by Mohindra and associates [22]. Who showed that MRI can detect cavernous sinus invasion and vascular complications such as ischemia/infarction.
An aggressive sinonasal and orbital inflammatory process was observed in all of our 84 patients. This behaviour was also reported previously, who suggested that the association between orbital cellulitis and sinusitis in the context of immunosuppression should prompt the diagnosis of mucormycosis. However, the differential diagnosis should consider other fungi, Graves' disease, carotid-cavernous fistula and thrombosis, bacterial cellulitis, inflammatory pseudotumor, and paranasal sinus tumor The aggressive clinical features of the disease can suggest the diagnosis of fungal infection
Bone involvement was seen in 76 patients both neurocranium and viscerocranium are involved and the commonest bone involved is the frontal bone (Figure 7). Intracerebral involvement was seen in 85 patients. Among these 3 patients showed early cerebritis and 35 patients showed abscesses out of which 30 were fungal/ mycotic abscesses and the remaining 5 were pyogenic abscesses, probably due to secondary bacterial infection (Figure 4-6 and 9). 1 patient showed optic nerve infarction and brainstem and posterior fossa abscess in the intracranial compartment (Figure 8). In our study we noticed that Perineural spread/along the neurovascular bundle is more common with mucor. 17 patients showed epidural collections, 16 patients showed infarcts and 9 patients showed pachymeningitis (Figure 7 and 8). 5 patients showed sub-periosteal collection (Figure 10). In our study, surgical interventions like FESS were done in 90% of all patients. Orbital exenterations were performed in 18, orbital decompression was done in 10 patients, craniotomy was done in 5 patients, and maxillectomy was done in 6 patients. Mandibulectomy was done in 1 case. More extensive debridement of necrotic tissue was performed as required in each particular case according to imaging and surgical findings. All patients received appropriate antifungals like amphotericin-B, locally and parenterally. Correction of uncontrolled diabetes/diabetic ketoacidosis was done.
Mucormycosis has earned its reputation as the most acutely fatal fungal infection known to humans. Therefore it is important that if the diagnosis is suspected, the suspicion be acted on immediately. In our study prognosis is relatively good in younger individuals who are below 40 years. 12 patients (12%) who are above 40 years with a history of uncontrolled diabetes and steroid usage and with other co-morbidities have died. Among 12, 2 patients are of Covid negative and in stages 1 and 2, who died with comorbidities alone. 10 patients are of Covid positive and all died of intracranial extension succumbed to the disease and eventually died in stage 3. Several previous reports have suggested that when limited involvement of the paranasal sinuses is present, survival rates are between 50% and 80% [3]. However, when brain invasion has occurred, mortality is greater than 80% because of its lethal nature. Their findings are comparable to our study.
When all the imaging findings are correlated with culture and histopathology we found that out of 100 cases, 53 are mucor positive, 36 are sterile (we could not find growth of any fungal isolate) and the rest of the cases are non-mucor (other than mucor) and mixed group along with Aspergillosis, Candida.
Conclusion
Rhinocerebral mucormycosis is an acute, fulminant, and often lethal opportunistic infection typically affecting diabetic or other immunocompromised patients. Progressive and rapid involvement of the cavernous sinus, vascular structures, and intracranial contents is the usual evolution of rhino orbital cerebral mucormycosis. CT and MRI are valuable tools that are complementary to clinical evaluation in the early diagnosis to delineate the extent of the disease and its complications. Further imaging helps plan the surgery as it can give excellent anatomic detail. However, the prognosis is grave despite radical surgery and anti-fungal agents.
Declarations
Conflict of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article
Limitations
In the samples of Patients where fungal isolation/ culture came negative we tried to repeat the culture but unfortunately in some of the cases we could not do it because of the debilitated condition of the patient, in addition, a few patients died during the study.
Chronic persistent form of bone involvement after successful treatment was seen in 20 cases predominantly of frontal osteomyelitis and Cause could not be found out for this persistent infections in spite of effective treatment for 6 months.
Acknowledgements
My special acknowledgements to my post graduate students of Radiodiagnosis, Andhra medical college, Visakhapatnam and post graduate students of neurosurgery and microbiology. My sincere thanks to all the patients who participated and cooperated with us while collecting the data.
References
- Skiada, Anna, Ioannis Pavleas, and Maria Drogari-Apiranthitou. "Epidemiology and diagnosis of mucormycosis: an update." Journal of fungi, Vol. 6, No. 4, 2020, p. 265.
Google Scholar Crossref - Sen, Mrittika, et al. "Mucor in a viral land: a tale of two pathogens." Indian journal of ophthalmology, Vol. 69, No. 2, 2021, pp. 244-52.
Google Scholar - Sarkar, Sandip, et al. "COVID-19 and orbital mucormycosis." Indian Journal of Ophthalmology, Vol. 69, No. 4, 2021, pp. 1002-1004.
Google Scholar Crossref - Sen, Mrittika, et al. "COVID-19 and eye: a review of ophthalmic manifestations of COVID-19." Indian Journal of Ophthalmology, Vol. 69, No. 3, 2021, pp. 488-509.
Google Scholar Crossref - Cornely, Oliver A., et al. "Global guideline for the diagnosis and management of mucormycosis: an initiative of the European Confederation of Medical Mycology in cooperation with the Mycoses Study Group Education and Research Consortium." The Lancet infectious diseases, Vol. 19, No. 12, 2019, pp. 405-21.
Google Scholar Crossref - Honavar, Santosh G. "Code mucor: guidelines for the diagnosis, staging and management of rhino-orbito-cerebral mucormycosis in the setting of COVID-19." Indian journal of ophthalmology, Vol. 69, No. 6, 2021, pp. 1361-65.
Google Scholar Crossref - Abramson, Eugene, Dana Wilson, and ronald A. Arky. "Rhinocerebral phycomycosis in association with diabetic ketoacidosis: report of two cases and a review of clinical and experimental experience with amphotericin B therapy." Annals of Internal Medicine, Vol. 66, No. 4, 1967, pp. 735-42.
Google Scholar Crossref - Petrikkos, George, et al. "Epidemiology and clinical manifestations of mucormycosis." Clinical Infectious Diseases, Vol. 54, No. 1, 2012, pp. S23-S34.
Google Scholar Crossref - Nussbaum, Eric S., and Walter A. Hall. "Rhinocerebral mucormycosis: changing patterns of disease." Surgical neurology, Vol. 41, No. 2, 1994, pp. 152-56.
Google Scholar Crossref - Hopkins, M. A., and D. M. Treloar. "Mucormycosis in diabetes." American Journal of Critical Care, Vol. 6, No. 5, 1997, pp. 363-67.
Google Scholar Crossref - Kohn, Roger, and Robert Hepler. "Management of limited rhino-orbital mucormycosis without exenteration." Ophthalmology, Vol. 92, No.10, 1985, pp. 1440-44.
Google Scholar Crossref - Abramson, Eugene, Dana Wilson, and Ronald a. Arky. "Rhinocerebral phycomycosis in association with diabetic ketoacidosis: report of two cases and a review of clinical and experimental experience with amphotericin B therapy." Annals of Internal Medicine, Vol. 66, No. 4, 1967, pp. 735-42.
Google Scholar Crossref - Rangel-Guerra, Ricardo A., et al. "Rhinocerebral and systemic mucormycosis. Clinical experience with 36 cases." Journal of the neurological sciences, Vol. 143, No. 1-2, 1996, pp. 19-30.
Google Scholar Crossref - Thajeb, Peterus, Teguh Thajeb, and Daofu Dai. "Fatal strokes in patients with rhino-orbito-cerebral mucormycosis and associated vasculopathy." Scandinavian journal of infectious diseases, Vol. 36, No. 9, 2004, pp. 643-48.
Google Scholar Crossref - Ochi, James W., et al. "Rhinocerebral mucormycosis: results of aggressive surgical debridement and amphotericin B." The Laryngoscope, Vol. 98, No. 12, 1988, pp. 1339-42.
Google Scholar Crossref - Sherman, D. D., and B. N. Lemke. "Orbital anatomy and its clinical applications." Duane's Clin Ophthalmol, Vol. 2, 1992, pp. 13-20.
Google Scholar - Gamba, Jorge L., et al. "Craniofacial mucormycosis: assessment with CT." Radiology, Vol. 160, No. 1, 1986, pp. 207-12.
Google Scholar Crossref - Terk, Michael R., et al. "MR imaging in rhinocerebral and intracranial mucormycosis with CT and pathologic correlation." Magnetic resonance imaging, Vol. 10, No. 1, 1992, pp. 81-87.
Google Scholar Crossref - Harrill, Willard C., et al. "Chronic rhinocerebral mucormycosis." The Laryngoscope, Vol. 106, No. 10, 1996, pp. 1292-97.
Google Scholar Crossref - Van Johnson, E., et al. "Bilateral cavernous sinus thrombosis due to mucormycosis." Archives of Ophthalmology, Vol. 106, No. 8, 1988, pp. 1089-92.
Google Scholar Crossref - Mohindra, Sandeep, et al. "Rhinocerebral mucormycosis: the disease spectrum in 27 patients." Mycoses, Vol. 50, No. 4, 2007, pp. 290-96.
Google Scholar Crossref - Mnif, N., et al. "Imaging of rhinocerebral mucormycosis." Journal de Radiologie, Vol. 86, No. 9, 2005, pp. 1017-20.
Google Scholar Crossref