Research Article - International Journal of Medical Research & Health Sciences ( 2022) Volume 11, Issue 10
Review on Prevalence of Asthmatic Patient
Owusu Emmanuel* and Gurleen KaurOwusu Emmanuel, Department of Respiratory Medicine, Global Groups of Institutes, Amritsar Punjab, India, Email: nanawusus96@gmail.com
Received: 05-May-2022, Manuscript No. IJMRHS-22-62827(PQ); Editor assigned: 09-May-2022, Pre QC No. IJMRHS-22-62827; Reviewed: 23-May-2022, QC No. IJMRHS-22-62827(R); Revised: 04-Jul-2022, Manuscript No. IJMRHS-22-62827; Published: 11-Jul-2022
Abstract
Asthma is a condition in which your airways narrow and swell and may produce extra mucus. This can make breathing difficult and trigger coughing, a whistling sound (wheezing) when you breathe out and shortness of breath. For some people, asthma is a minor nuisance. For others, it can be a major problem that interferes with daily activities and may lead to a life-threatening asthma attack. Asthma can't be cured, but its symptoms can be controlled; because asthma often changes over time.
Keywords
Asthma, Shortness of breath, Life-threatening, Whistling sound
Introduction
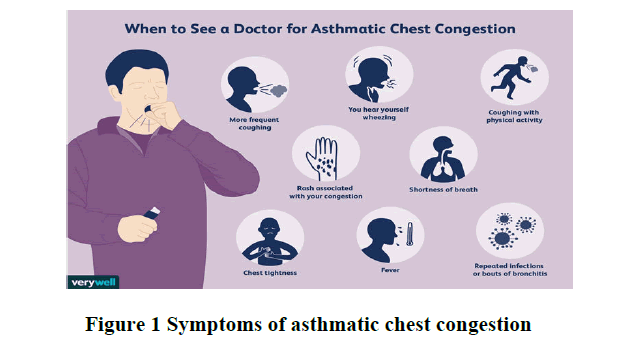
Symptoms
• Asthma symptoms vary from person to person. You may have infrequent asthma attacks, have symptoms only at certain times such as when exercising or have symptoms all the time.
Asthma signs and symptoms include:
• Shortness of breath.
• Chest tightness or pain.
• Wheezing when exhaling, this is a common sign of asthma in children.
• Trouble sleeping caused by shortness of breath, coughing or wheezing.
• Coughing or wheezing attacks that are worsened by a respiratory virus, such as a cold or the flu.
Signs that your asthma is probably worsening include:
• Asthma signs and symptoms that is more frequent and bothersome.
• Increasing difficulty breathing, as measured with a device used to check how well your lungs are working (peak flow meter).
• The need to use a quick-relief inhaler more often.
For some people, asthma signs and symptoms flare up in certain situations:
• Exercise-induced asthma, which may be worse when the air is cold and dry.
• Occupational asthma, triggered by workplace irritants such as chemical fumes, gases or dust.
• Allergy-induced asthma triggered by airborne substances, such as pollen, mold spores, cockroach waste, or particles of skin and dried saliva shed by pets (pet dander) (Figure 1).
Contact your doctor:
• If you think you have asthma. If you have frequent coughing or wheezing that lasts more than a few days or any other signs or symptoms of asthma see your doctor. Treating asthma early may prevent long-term lung damage and help keep the condition from getting worse over time.
• To monitor your asthma after diagnosis. If you know you have asthma, work with your doctor to keep it under control. Good long-term control helps you feel better from day to day and can prevent a life-threatening asthma attack.
• If your asthma symptoms get worse. Contact your doctor right away if your medication doesn't seem to ease your symptoms or if you need to use your quick-relief inhaler more often.
• Don't take more medication than prescribed without consulting your doctor first. Overusing asthma medication can cause side effects and may make your asthma worse.
• To review your treatment. Asthma often changes over time. Meet with your doctor regularly to discuss your symptoms and make any needed treatment adjustments.
Causes: It isn't clear why some people get asthma and others don't, but it's probably due to a combination of environmental and inherited (genetic) factors.
Asthma triggers: Exposure to various irritants and substances that trigger allergies (allergens) can trigger signs and symptoms of asthma. Asthma triggers are different from person to person and can include:
• Airborne allergens, such as pollen, dust mites, mold spores, pet dander or particles of cockroach waste.
• Respiratory infections, such as the common cold.
• Physical activity.
• Cold air.
• Air pollutants and irritants, such as smoke.
• Certain medications, including beta blockers, aspirin, and nonsteroidal anti-inflammatory drugs, such as ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve).
• Strong emotions and stress.
• Sulfites and preservatives added to some types of foods and beverages, including shrimp, dried fruit, processed potatoes, beer and wine.
• Gastroesophageal Reflux Disease (GERD), a condition in which stomach acids back up into your throat.
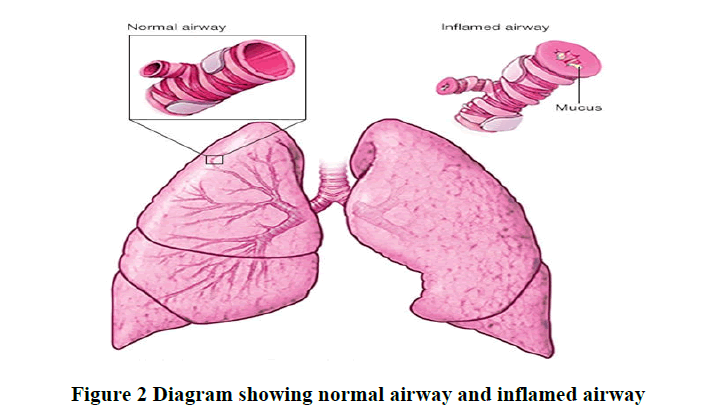
Risk factors: A number of factors are thought to increase your chances of developing asthma. They include:
• Having a blood relative with asthma, such as a parent or sibling.
• Having another allergic condition, such as atopic dermatitis which causes red, itchy skin or hay fever which causes a runny nose, congestion and itchy eyes.
• Being overweight.
• Being a smoker.
• Exposure to secondhand smoke.
• Exposure to exhaust fumes or other types of pollution.
• Exposure to occupational triggers, such as chemicals used in farming, hairdressing and manufacturing (Figure 2).
Complications: Asthma complications include:
• Signs and symptoms that interfere with sleep, work and other activities.
• Sick days from work or school during asthma flare-ups.
• A permanent narrowing of the tubes that carry air to and from your lungs (bronchial tubes), which affects how well you can breathe.
• Emergency room visits and hospitalizations for severe asthma attacks.
• Side effects from long-term use of some medications used to stabilize severe asthma.
• Proper treatment makes a big difference in preventing both short-term and long-term complications caused by asthma.
Prevention
While there's no way to prevent asthma, you can design a step-by-step plan for living with your condition and preventing asthma attacks.
• Follow your asthma action plan. With your doctor and health care team, write a detailed plan for taking medications and managing an asthma attack. Then be sure to follow your plan.
• Asthma is an ongoing condition that needs regular monitoring and treatment. Taking control of your treatment can make you feel more in control of your life.
• Get vaccinated for influenza and pneumonia. Staying current with vaccinations can prevent flu and pneumonia from triggering asthma flare-ups.
• Identify and avoid asthma triggers. A number of outdoor allergens and irritants ranging from pollen and mold to cold air and air pollution can trigger asthma attacks. Find out what causes or worsens your asthma, and take steps to avoid those triggers.
• Monitor your breathing. You may learn to recognize warning signs of an impending attack, such as slight coughing, wheezing or shortness of breath. But because your lung function may decrease before you notice any signs or symptoms, regularly measure and record your peak airflow with a home peak flow meter. A peak flow meter measures how hard you can breathe out. Your doctor can show you how to monitor your peak flow at home.
• Identify and treat attacks early. If you act quickly, you're less likely to have a severe attack. You also won't need as much medication to control your symptoms. When your peak flow measurements decrease and alert you to an oncoming attack, take your medication as instructed. Also, immediately stop any activity that may have triggered the attack. If your symptoms don't improve, get medical help as directed in your action plan.
• Take your medication as prescribed. Don't change your medications without first talking to your doctor, even if your asthma seems to be improving. It's a good idea to bring your medications with you to each doctor visit. Your doctor can make sure you're using your medications correctly and taking the right dose.
• Pay attention to increasing quick-relief inhaler use. If you find yourself relying on your quick-relief inhaler, such as albuterol, your asthma isn't under control. See your doctor about adjusting your treatment
Diagnosis
Physical exam: Perform a physical exam to rule out other possible conditions, such as a respiratory infection or Chronic Obstructive Pulmonary Disease (COPD). Your doctor will also ask you questions about your signs and symptoms and about any other health problems.
Tests to measure lung function: You may be given lung function tests to determine how much air moves in and out as you breathe. These tests may include:
Spirometry: This test estimates the narrowing of your bronchial tubes by checking how much air you can exhale after a deep breath and how fast you can breathe out.
Peak flow: A peak flow meter is a simple device that measures how hard you can breathe out. Lower than usual peak flow readings are a sign that your lungs may not be working as well and that your asthma may be getting worse. Your doctor will give you instructions on how to track and deal with low peak flow readings.
Additional Tests
Other tests to diagnose asthma include:
Methacholine challenge: Methacholine is a known asthma trigger. When inhaled, it will cause your airways to narrow slightly. If you react to the methacholine, you likely have asthma. This test may be used even if your initial lung function test is normal.
Imaging tests: A chest X-ray can help identify any structural abnormalities or diseases (such as infection) that can cause or aggravate breathing problems.
Allergy testing: Allergy tests can be performed by a skin test or blood test. They tell you if you're allergic to pets, dust, mold or pollen. If allergy triggers are identified, your doctor may recommend allergy shots.
Nitric oxide test: This test measures the amount of the gas nitric oxide in your breath. When your airways are inflamed a sign of asthma, you may have higher than normal nitric oxide levels. This test isn't widely available.
Sputum eosinophils: This test looks for certain white blood cells (eosinophils) in the mixture of saliva and mucus (sputum) you discharge during coughing. Eosinophils are present when symptoms develop and become visible when stained with a rose-colored dye.
Provocative testing for exercise and cold-induced asthma: In these tests, your doctor measures your airway obstruction before and after you perform vigorous physical activity or take several breaths of cold air (Table 1).
| Asthma classification | Signs and symptoms |
|---|---|
| Mild intermittent | Mild symptoms up to two days a week and up to two nights a month. |
| Mild persistent | Symptoms more than twice a week, but no more than once in a single day. |
| Moderate persistent | Symptoms once a day and more than one night a week. |
| Severe persistent | Symptoms throughout the day on most days and frequently at night. |
How Asthma is classified
Asthma is classified into four general categories:
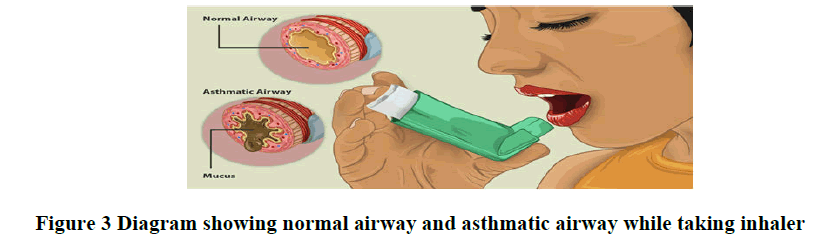
Treatment: Prevention and long-term control are key to stopping asthma attacks before they start. Treatment usually involves learning to recognize your triggers, taking steps to avoid triggers and tracking your breathing to make sure your medications are keeping symptoms under control. In case of an asthma flare-up, you may need to use a quickrelief inhaler [1].
Medications
Long-term asthma control medications: Generally taken daily, are the cornerstones of asthma treatment. These medications keep asthma under control on a day-to-day basis and make it less likely you'll have an asthma attack. Types of long-term control medications include:
Inhaled corticosteroids: These medications include fluticasone propionate (Flovent HFA, Flovent Diskus, Xhance), budesonide (Pulmicort Flexhaler, Pulmicort Respules, Rhinocort), ciclesonide (Alvesco), beclomethasone (Qvar Redihaler), mometasone (Asmanex HFA, Asmanex Twisthaler) and fluticasone furoate (Arnuity Ellipta).You may need to use these medications for several days to weeks before they reach their maximum benefit. Unlike oral corticosteroids, inhaled corticosteroids have a relatively low risk of serious side effects.
Leukotriene modifiers: These oral medications including montelukast (Singulair), zafirlukast (Accolate) and zileuton (Zyflo) help relieve asthma symptoms. Montelukast has been linked to psychological reactions, such as agitation, aggression, hallucinations, depression and suicidal thinking. Seek medical advice right away if you experience any of these reactions.
Combination inhalers: These medications such as fluticasone salmeterol (Advair HFA, Airduo Digihaler, others), budesonide formoterol (Symbicort), formoterol mometasone (Dulera) and fluticasone furoate-vilanterol (Breo Ellipta) contain a long-acting beta agonist along with a corticosteroid.
Theophylline: Theophylline (Theo-24, Elixophyllin, Theochron) is a daily pill that helps keep the airways open by relaxing the muscles around the airways. It's not used as often as other asthma medications and requires regular blood tests.
Quick-relief (rescue medications: These are used as needed for rapid, short-term symptom relief during an asthma attack. They may also be used before exercise if your doctor recommends it. Types of quick-relief medications include.
Short-acting beta agonists: These inhaled, quick-relief bronchodilators act within minutes to rapidly ease symptoms during an asthma attack. They include albuterol (ProAir HFA, Ventolin HFA, others) and levalbuterol (Xopenex, Xopenex HFA). Short-acting beta agonists can be taken using a portable, hand-held inhaler or a nebulizer, a machine that converts asthma medications to a fine mist. They're inhaled through a face mask or mouthpiece.
Anticholinergic agents: Like other bronchodilators, ipratropium (Atrovent HFA) and tiotropium (Spiriva, Spiriva Respimat) act quickly to immediately relax your airways, making it easier to breathe. They're mostly used for emphysema and chronic bronchitis, but can be used to treat asthma.
Oral and intravenous corticosteroids: These medications which include prednisone (Prednisone Intensol, Rayos) and methylprednisolone (Medrol, Depo-Medrol, Solu-Medrol) relieve airway inflammation caused by severe asthma. They can cause serious side effects when used long term, so these drugs are used only on a short-term basis to treat severe asthma symptoms. If you have an asthma flare-up, a quick relief inhaler can ease your symptoms right away. But you shouldn't need to use your quick relief inhaler very often if your long-term control medications are working properly. Keep a record of how many puffs you use each week. If you need to use your quick relief inhaler more often than your doctor recommends, see your doctor. You probably need to adjust your long-term control medication [2].
Allergy medications may help if your asthma is triggered or worsened by allergies. These include:
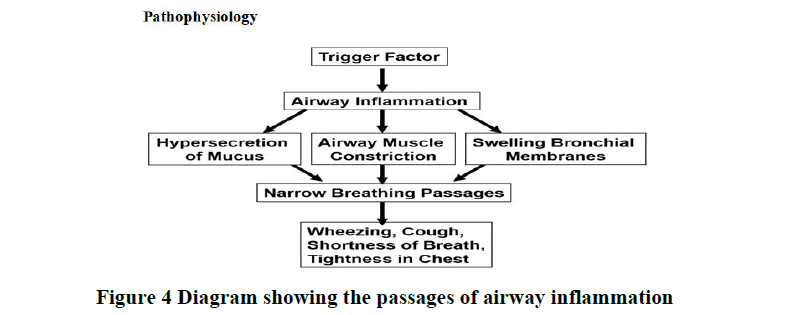
Allergy shots (immunotherapy): Over time, allergy shots gradually reduce your immune system reaction to specific allergens (Figures 3 and 4).
Pathophysiology
Statement of Problem: This study is to seek into the asthma on how it mostly affect individual and the method to put in place to prevent the reoccurrences of this diseases and better measures to put to in place to improve the health of the of the people who are suffering from the sickle asthma in our society. By doing this it will help people to know their status and how well to manage this diseases.
Research Objectives
• The research objective emphasizes on what to derive from the study and based on how to deal with such kind of situation. Therefore this study is to find out.
• Which age groups are mostly affected with Asthma?
• At which period do people experience the symptoms of Asthma?
• Which drug first come in mind when people suffering from Asthma?
Literature Review
On this study there were several theories and literatures which were delve into to find out in this study.
Literatures
Chronic conditions are often the catalyst for physical, psychological and financial burden. Individuals suffering from asthma often demonstrate difficulties in managing their condition as well as altering their lifestyle to include factors such as healthy exercise routines and appropriate environmental surroundings. Asthma, which is a chronic inflammatory disease of the airways, has been on the rise over the past decade with increasing prevalence within children in the United States (Centers for Disease Control and Prevention (CDC), 2009). It is estimated that a total of 22 million individuals suffer from asthma, with nearly 6 million of these individuals being children (National Institutes of Health (NIH), 2008). Physical side effects of the condition include coughing, wheezing, shortness of breath and chest tightness (NIH, 2008). These symptoms could greatly impact the quality of life experienced by the asthmatic individual due to restriction of activity, discomfort, embarrassment and the constant concern for their condition. It is crucial to identify such conditions early on and implement appropriate treatment given that patterns of behavior developed during childhood serve as predictors of development of adult disease. Thus, poor management of asthma in childhood and adolescence can lead to ineffective management in adulthood. This increases the risk of developing additional diseases such as obesity or cardiac disease due to the restrictions (such as exercising) placed on an individual with improperly managed asthma. Furthermore, the severity of asthma as a chronic condition is demonstrated in that approximately 5,500 individuals die from asthma related emergencies each year, Introduction to lit review should introduce subject and problem clearly state purpose, cite key sources and data, narrow the topic, subject key sources key sources purpose problem key data 2 and the overall financial costs of asthma reached an estimated $18 billion in 2009 (asthma and allergy foundation, 2010). Treatment for chronic asthma although it is generally a chronic condition, asthma can be controlled through effective lifestyle and medical management. Environmental exposure to allergens and air pollutants can cause and exacerbate the symptoms of asthma, but symptoms can be reduced through the regulation of environmental exposures and the use of medication. Medication for asthma consists of short-term relief of symptoms and long-term preventative controls, which act to prevent the occurrence of symptoms. The majority of individuals suffering from asthma utilize medication for short-term relief of symptoms, which are most commonly inhaled short-acting beta agonists that act quickly in relaxing the airway muscles once constriction has already occurred (NIH, 2008). The use of medication for long-term control aims to prevent the symptoms of asthma, including asthma attacks, which are episodes in which breathing is negatively affected due to restriction and inflammation of the airways (NIH, 2008). The most common and preferred long-term treatment is inhaled corticosteroids, which reduce inflammation and subsequently prevent the chain reaction that leads to the presence of symptoms (NIH, 2008). This preventative medication acts by blocking late-phase reactions to allergens, reducing hyper responsiveness, and inhibiting the activation of inflammatory cell migration (National Heart, Lung and Blood Institutes (NHLBI), 2007). Corticosteroids are the most potent and effective antiinflammatory medication currently available to individuals with asthma and other chronic lung disease (NHLBI, 2007). Thus, the use of medication for long-term control is often prescribed on a daily regimen and Key, current data Topic Sentence 3 greatly reduces the occurrence of symptoms. A report published by the Global Initiative for Asthma (GINA) (2009) stated that the use of corticosteroids can result in improved lung functioning in as little as 1 week, while discontinuing the use of corticosteroids can result in deterioration in asthma symptoms within weeks. In addition, research has demonstrated a close relationship between asthma and allergic rhinitis. This suggests that individuals with asthma often experience an exacerbation of symptoms due to allergies to substances such as dust, pollen, or dander. This occurs when an individual breathes in substances, such as those previously mentioned, thus initiating the onset of symptoms (such as itchiness, runny nose, watery eyes, sneezing). These symptoms are closely related to the onset of asthmatic symptoms. Thus, treatment for individuals with asthma often includes medication to treat both asthma and allergies in order to more effectively control the condition. Such regimens targeting the treatment of both asthma and allergy symptoms have been found effective in establishing control over the onset of symptoms. Despite the effectiveness of medication in the control of asthma symptoms, nonadherence to medical regimens often creates a barrier to successful intervention. In other words, the potential effectiveness of medication in controlling a wide range of conditions is being thwarted by a problem of human behavior. In the case of nonadherence it is crucial to examine the environmental contingencies affecting human adherence behavior in order to resolve the issue. Transition Topic narrows/thesis statement paragraph unity paragraph unity paragraph unity transition paragraph unity 4 Rates of non-adherence to medical regimens despite the medical advancements in treating chronic disease, nonadherence reduces the effectiveness of medical regimens in controlling the symptoms of various conditions. Individuals suffering from a variety of chronic disease often depend on medication to control, reduce or prevent symptoms from occurring. However, nonadherence continues to be a problem in the effective treatment of such disease. In a quantitative meta-analysis of adherence literature, DiMatteo (2004) examined 569 studies on adherence that were conducted over a 50-year period (1948-1998). Studies that defined and measured adherence to a prescribed medical regimen or preventative regimen (such as exercising) were included in the review. Results of the analysis indicated that adherence ranged from 4.6% to 100% with a median of 76% and an average adherence rate of 75.2%. The results of the meta-analysis represent the widespread problem of adherence among individuals prescribed a medical regimen. Research has shown that nonadherence is a significant problem for acute illnesses, chronic conditions such as asthma and even for conditions in which the effects of nonadherence can potentially be life threatening. For example, Mattar evaluated rates of adherence in children with otitis media, a typically acute illness. Patients (n=100) aged between 1 and 12 years old were prescribed an antibiotic regimen for otitis media. A follow-up appointment was scheduled and the amount of antibiotics consumed over a 10-day period was measured (taking into account the size of the spoon used to deliver medication). Results of the study indicated that only 5% of participants (n=100) demonstrated full compliance, thus indicating that 95% of participants failed to demonstrate adherence to medical LR arranged by theme/idea Selected sources by theme Body of Lit Review discusses key sources, arranged thematically. 5 regimens, Sublett, Pollard, Kadlec and Karibo further demonstrated the issue of nonadherence for individuals with asthma. In examining salivary theophylline (a medication used to treat respiratory disease) levels of participants with asthma, Sublett found that 98% had levels less than 10 mcg/ml with 75.5% due to low levels of medical adherence. Furthermore, Korsch demonstrated the problem of nonadherence in circumstances in which the side effects of nonadherence are potentially fatal by examining 14 participants undergoing immunosuppressive treatment following renal transplantation. Results of the study indicated that all participants disrupted the prescribed regimen following transplantation; eight participant’s lost allograft, or transplant, function and six decreased allograft function. This particular study was especially significant in its demonstration of the perpetuation of nonadherence to medication in circumstances in which nonadherence is potentially fatal or life threatening. The prevalence of nonadherence has further been demonstrated in adolescents who suffer from chronic conditions, specifically asthma. Several studies of asthmatic children have found that more than half of children on daily regimens for asthma fail to use medication as prescribed, demonstrated the issue of nonadherence to medical regimens by examining the extent to which adolescents with asthma comply with a prescribed dosage of medications. Results indicated that approximately 51% of adolescents demonstrated low adherence rates to prescribed regimens. McQuaid assessed adolescent adherence to preventative asthma medications and found an even lower rate of adherence. Participants’ medication intake was electronically monitored for a period of 1 month and results indicated that adherence was approximately 48% of prescribed doses. These studies demonstrate both the existence and the alarming Source evaluated Topic sentence 6 rates of nonadherence for adolescents who suffer from chronic conditions, specifically asthma. Cognitive behavioral approaches in increasing adherence most commonly, the issue of patient nonadherence to medical regimens has been approached utilizing a cognitive behavioral model. The theoretical underpinning of such an approach postulates that clinical populations “attend to, remember, and interpret events in ways that are congruent with their disorder”. It is assumed that “internal processes and states that mediate between the environment and behavior explain the behavior”. In other words, it is what the patient understands about the details of the regimen that determines level of adherence, and therefore nonadherence can be attributed to low levels of understanding regarding the medical treatment. This includes patient comprehension of factors such as biological understanding of disease, schedule of regimen, protocol regarding missed dosage, side effects, and prescription duration. Given this theoretical foundation, cognitive behavioral approaches seek to identify and modify maladaptive thinking and comprehension regarding the medical regimen in order to effectively increase patient adherence to prescription. The following research is a sample of cognitive behavioral studies that seek to modify thinking in order to increase adherence to medical regimens among adolescents. Further demonstrated the use of cognitive behavioral strategies to increase adolescent adherence to medical regimens among adolescents with diabetes. Participants (N=6) were trained in cognitive restructuring and problem solving during individual sessions. This consisted of LR arranged by theme/idea integrated quotes paraphrased in own words organized around ideas selected sources by theme 7 three phases: First, participants conceptualized their adherence efforts with an emphasis on factors that both interfere and facilitate adherence behaviors. The second phase was the skill acquisition and rehearsal phase in which participants learned how to challenge and restructure maladaptive thinking by examining evidence for and against these thoughts (developing alternative explanations). During this phase, participants were taught to identify the problem, brainstorm solutions to the problem, generate consequences to the potential solutions, and make decisions by weighing in the most desirable outcomes. Lastly, participants applied the skills acquired to hypothetical and potential future adherence issues (thus developing alternative cognitions). Dependent measures of interest consisted of glucose checking, insulin injections, meals and snacks, level of physical activity, and injection-meal timing (which were based on self-report at a 1-3 month follow-up). Results of the study demonstrated that the cognitive behavioral intervention had a positive impact on at least one of the five self-care behaviors for each participant. Given the low level of change in adherence behavior, the present study provides weak support for cognitive-behavioral methods as an effective approach to increasing adolescent adherence. Furthermore, Van Es utilized a cognitive-behavioral approach to increase the adherence of 112 asthmatic adolescents. The study examined the effectiveness of the Attitude-social influence-Self- Efficacy (ASE) model, which assumes that adherence behavior is determined by attitudes, social influences and selfefficacy expectations (derived from the theory of reasoned action and the social cognitive theory). Participants in the experimental group received standard, or usual, care from a pediatrician in addition to attending individual and group sessions with an asthma specialist. These sessions aimed to increase adolescent adherence by invoking a positive attitude, developing increased feelings of social selected sources by theme source evaluated study summarized 8 support and enhancing self-efficacy. Results, which were self-reported dependent measures, indicated that there were no statistically significant differences between the control group and experimental group during a 12- month follow-up. Yet, during the 24-month follow-up reported adherence was statistically higher in the experimental group. However, the researchers state that this could have been due to chance given that correction for multiple testing by means of the bonferroni method resulted in no significant differences between the two groups. The study exemplifies the use of a cognitive behavioral approach but demonstrates that this approach, based on the ASE model, was ineffective in increasing adolescent adherence throughout the course of the study. Although there were increases in adherence during a follow-up, these changes can be attributed to a multitude of other factors given that there was not an initial increase in adherence during the study. Further, the study demonstrated weakness in that measures of adherence were strictly based on self-reported dependent measures [3,4].
Methodology
Study design: This is a cross sectional study, conducted at Amandeep hospital.
Study area: Amandeep hospital in Verka city, Amritsar Punjab state.
Study population: Patients with Asthma attended to Amandeep Hospital in the period of study was 30.
Inclusion criterial: All patients with Asthma of both sexes attending to the hospitals were included in this study.
Data collection: Questionnaires were used to collect the information about demographic data, family history and symptoms.
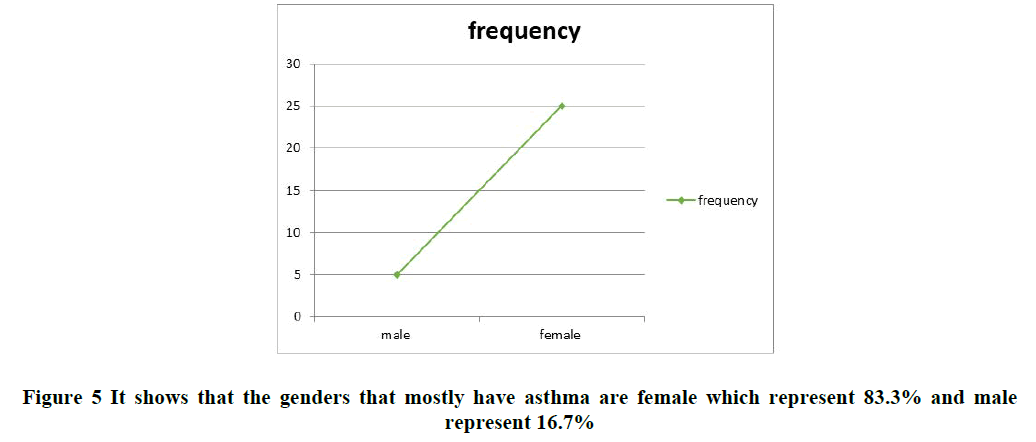
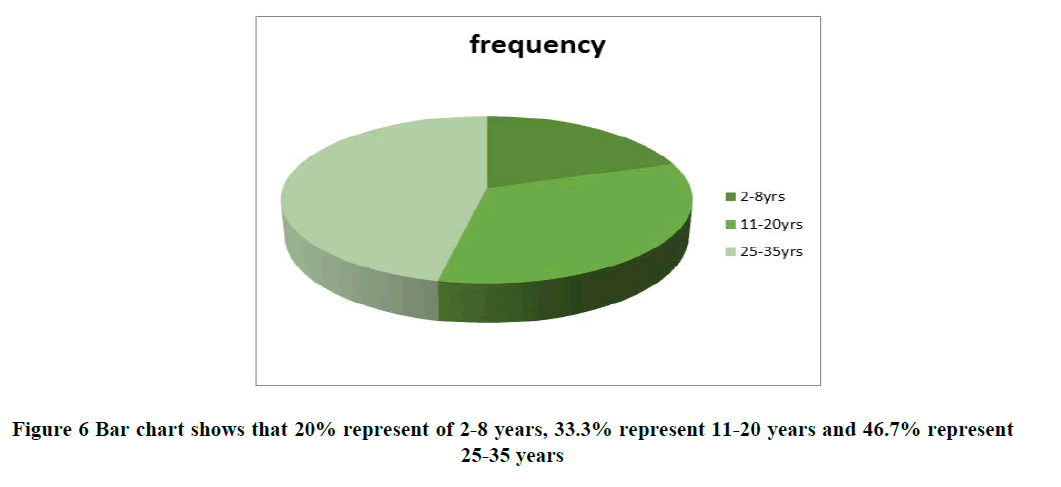
Data analysis: Data obtained was analyzed using Statistical Package for Social Sciences (SPSS) software package version 13 (by use T tests) (Tables 2 and 3 and Figures 5 and 6).
| Gender | frequency | percentage |
|---|---|---|
| Male | 5 | 16.70% |
| Female | 25 | 83.30% |
Data Analysis and Interpretation
Common Drugs for Asthma
• Fluticasone
• Budesonide
• Mometasone
• Ciclesonide
Discussion
Asthma is a condition in which your airways narrow and swell and may produce extra mucus. This can make breathing difficult and trigger coughing, a whistling sound (wheezing) when you breathe out and shortness of breath. For some people, asthma is a minor nuisance. For others, it can be a major problem that interferes with daily activities and may lead to a life-threatening asthma attack [5].
Asthma can't be cured, but its symptoms can be controlled. Because asthma often changes over time, it's important that you work with your doctor to track your signs and symptoms and adjust your treatment as needed. The study delve into how people are suffered from Asthma and the preventive measures that will help to improve the health of the people as it is clear that asthma does not have a cure so it is ascertained that it is very necessary that it is important to focus on the majority of people are normally affected by people. It is really necessary to put great measures on it to improve the health of the people.
Recommendation
• Routine measurement should be done for all patients as follow up visits.
• Adequately controlled studies using more inflammatory markers are warranted to define the role of chronic inflammatory state with vaso-occlusive crises and specific complications of the disease.
• Active community medical education about the Asthma through medical personnel and public societies
Conclusion
• According to the sex, the results showed increased male patients more than female patients. Most of the patients had family history of Asthma.
• Clinical feature in the study patients were severe breathing, wheezing, chest beating.
• It was also ascertained that age 2-8 years with Asthma was higher than the other age discussed.
References
- Jenkins, Christine, John Costello and Linda Hodge. Systematic review of prevalence of aspirin induced asthma and its implications for clinical practice. BMJ, Vol. 328, No. 7437, 2004, pp. 434.
[Crossref] [Googlescholar] [Indexed]
- Rehman, Amna, Fatima Amin and Saleha Sadeeqa. Prevalence of asthma and its management: A review. The Journal of the Pakistan Medical Association, Vol. 68, No. 12, 2018, pp. 1823-1827.
[Googlescholar] [Indexed]
- Rajan and Jessica P. Prevalence of aspirin-exacerbated respiratory disease among asthmatic patients: a meta-analysis of the literature. Journal of Allergy and Clinical Immunology, Vol. 135, No. 3, 2015, pp. 676-681.
[Crossref] [Googlescholar] [Indexed]
- Peters and Stephen P. Uncontrolled asthma: a review of the prevalence, disease burden and options for treatment. Respiratory Medicine, Vol.100, No. 7, 2006, pp. 1139-1151.
[Crossref] [Googlescholar] [Indexed]
- Toskala, Elina and David W. Kennedy. Asthma risk factors. In International Forum of Allergy and Rhinology, Vol. 5, No. 1, 2015, pp. 11-16.
[Crossref] [Googlescholar] [Indexed]