Case Report - International Journal of Medical Research & Health Sciences ( 2022) Volume 11, Issue 12
Recurrent follicular conjunctivitis: A complication of Molluscum Contagiosum
Harshita Dubey*, Prabha Gupta and D. K. ShakyaHarshita Dubey, Department of Ophthalmology, Gajra Raja Medical College, Madhya Pradesh, India, Email: hdubey.92@gmail.com
Received: 13-Sep-2022, Manuscript No. ijmrhs-22-74430; Editor assigned: 20-Sep-2022, Pre QC No. ijmrhs-22-74430 (PQ); Reviewed: 24-Nov-2022, QC No. ijmrhs-22-74430 (Q); Revised: 28-Nov-2022, Manuscript No. ijmrhs-22-74430 (R); Published: 20-Dec-2022
Abstract
To report a case of Molluscum Contagiosum presented with recurrent follicular conjunctivitis, successfully treated with surgical excision. A 23-year-old male presented with chief complaints of grittiness, discomfort in closing the eye along with mild redness in the same eye. He had previously been seen by a different ophthalmologist and had been treated with topical antibiotics, steroids, and anti-viral eye drops but no relief in the symptoms. On Slit lamp examination single dome shape with a center, umbilicated core in the right lower eyelid was noticed. Suspecting Molluscum Contagiosum and no improvement with the course of topical medication given, we decided to excision. The lesion was surgically excised and was sent for histopathological examination. Molluscum Contagiosum (MC) resolves spontaneously within months in healthy, immunocompetent individuals, it requires surgical treatment in refractory cases. After surgical excision, the patient's symptoms have completely resolved and no signs of follicular conjunctivitis are present. He remains under follow-up and no recurrence has been seen for 6 months
Keywords
Molluscum Contagiosum (MC), Follicular conjunctivitis, Histopathological examination
Introduction
Molluscum contagiosum (MC) is caused by a poxvirus that produces benign, self-limiting papular eruptions on the skin and mucous membranes [1]. It is particularly common in hot, developing countries and communities with poor personal hygiene. The condition is mostly seen in children but during the past 30 years has become more common in immunocompromised adults and patients with atopic Dermatitis, Sarcoidosis, etc [2].
Lesions are typically small (between two and six millimeters) and often have central depressions or umbilications that contain a waxy, curd-like core. They can be located anywhere on the body and usually occur in clusters. Diagnosis is usually based on clinical findings, and histopathological examination and laboratory tests are often not necessary [1].
Ophthalmic MC lesions are often located on the eyelids. Chronic conjunctivitis or Keratoconjunctivitis can be associated with eyelid lesions [3].
Case Presentation
A 23-year-old male presented to the outpatient department of Jayarogya hospital, Gwalior with chief complaints of a single raised painless lesion on the lower lid of the right eye for the past 3 months and a history of grittiness, discomfort while closing the eye along with mild redness in the same eye. He had previously been seen by a different ophthalmologist and had been treated with topical antibiotics, steroids, and anti-viral eye drop with relief in the symptoms. But recurrence was seen on stopping the medication.
Examination
On Slit lamp examination (Right Eye)
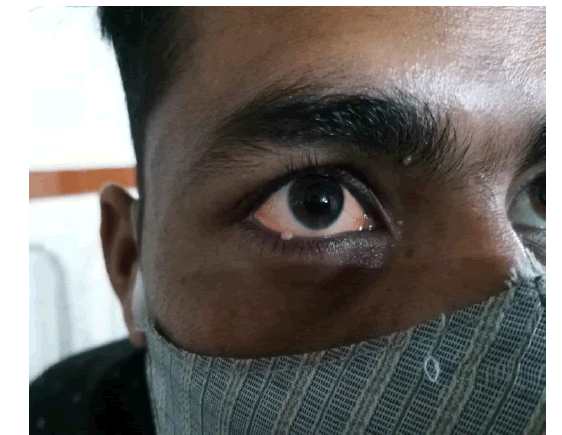
• Single lesion one-two millimeter dome shaped with a center umbilicated core in between the medial twothirds and lateral one-third of the right lower eyelid (Figure 1).
• The conjunctiva was hyperaemic and there was a follicular reaction in the lower fornix.
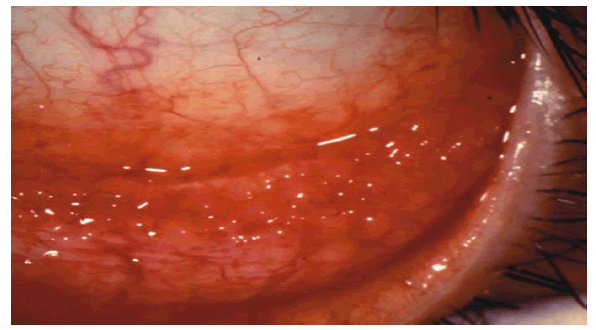
• A cornea was not involved (Figure 2).
Suspecting Molluscum Contagiosum and no improvement with the course of topical medication given we decided to excision. The lesion was surgically excised after clamping and hemostasis were ensured, preserving the integrity of the cyst wall the lesion was sent for histopathological examination.
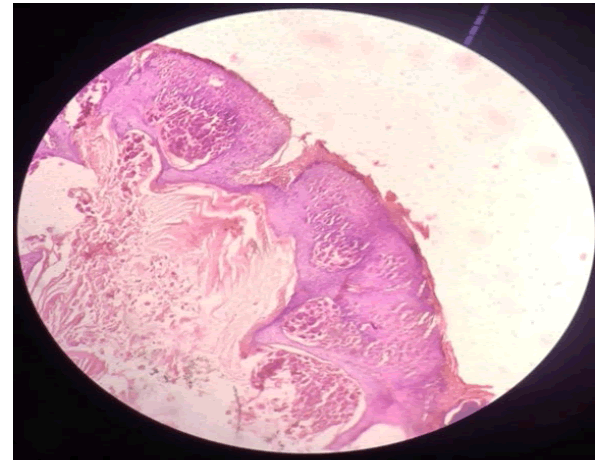
Histopathology report suggested stratified keratinized squamous epithelium with underlined dermis within the epidermis and a large central crater filled with molluscum bodies. The basal layers show intracytoplasmic eosinophilic inclusions that compress the nucleus to the periphery (Figure 3).
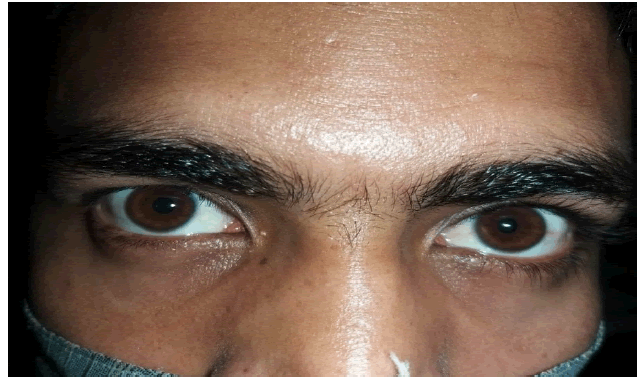
The patient's symptoms have completely resolved, and no signs of follicular conjunctivitis are present. He remains under follow up and no recurrence has been seen for 6 months (Figure 4).
Discussions
MC occurs worldwide but is more common in areas with tropical and humid climates. The virus is transmitted by close physical contact, autoinoculation, and occasionally, contaminated fomites (e.g., clothing, bath sponges, and towels), especially if the skin is wet. In adults, the disease may be spread by sexual contact and is typically found in a bathing-trunk distribution [2]. Ocular involvement of MC presents with round, small, hard papules on the eyelids. The virus proliferates in epithelial cells. After the lesions reach about 3 mm to 5 mm in diameter, a central depression forms due to the cellular damage mechanism and they typically develop the appearance of whitish lesions filled with caseous material and having a dimple or pit in the center [3]. Although the diagnosis is made clinically when these characteristic MC lesions are evident on the lids. The differential diagnosis of lid lesions can include basal cell Carcinoma, Papilloma, Chalazion, Sebaceous Cyst, Keratoacanthoma, Blepharitis, Wart, Eczema, obstructed nasolacrimal duct, and ectropion [2]. Viral proteins shed from the lid lesions into the tear film can lead to a hypersensitivity reaction with secondary chronic follicular reaction, punctate keratopathy in the conjunctiva, and some cases subepithelial opacities and pannus [4].
Conclusion
While MC lesions usually resolve spontaneously within a few monthsâ?? treatments such as excision, incision, Curettage, Cryotherapy, Cauterization, Topical Chemical Agents, and Oral Cimetidine can be used in refractory cases. It should be kept in mind that progressive corneal neovascularization and scarring may develop, especially in patients with chronic conjunctivitis and corneal involvement. There is no known antiviral treatment specific to MC. While topical ganciclovir is approved for use in acute herpetic keratitis, its efficacy has also been demonstrated against cytomegalovirus and some strains of adenovirus.Acknowledgements
I take this Opportunity to thank my our honorable, Professor and Head of the department, Dr. D.K. Shakya sir, Department of Ophthalmology, G.R. Medical College, Gwalior for his untiring humble support, wise knowledge,fatherly benevolence and guidance that helped me in the completion of my work. I proclaim my deepest love to my family who stood by me through all the thick and thins, provided me with ceaseless support, and filled me with the strength to take up this challenge. No writing assistance was taken from anyone else.
Declarations
Conflict of Interest
The authors’ declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding:
No funding source
Ethical approval
Not required
References
- Osadebe, Lynda U., et al. "Ocular molluscum contagiosum atypical clinical presentation." The Pediatric infectious disease journal, Vol. 33, No. 6, 2014, pp. 668-68.
Google Scholar Crossref - Serin, Sule, et al. "Eyelid molluscum contagiosum lesions in two patients with unilateral chronic conjunctivitis." Turkish journal of ophthalmology, Vol. 47, No. 4, 2017, p. 226.
Google Scholar Crossref - Schornack, Muriel M., et al. "Ocular manifestations of molluscum contagiosum." Clinical and experimental optometry, Vol. 89, No. 6, 2006, pp. 390-93.
Google Scholar Crossref - Mukherjee, Bipasha, Harshit Vaidya, and Md S. Alam. "Clinical profile and management outcomes of periocular molluscum contagiosum." TNOA Journal of Ophthalmic Science and Research, Vol. 58, No. 1, 2020, p. 5.
Google Scholar Crossref