Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 9
Radiological and Clinical Evaluation of Breast Lesions with Histopathological Correlation: A Prospective Study in a Tertiary Care Centre
Bomidi Sudha Rani*, P Bujjibabu, M Umamaheswar Rao and M Siva SreedharBomidi Sudha Rani, Department of Radio-diagnosis, King George Hospital, Visakhapatnam, India, Email: radiologysudha@gmail.com
Received: 16-Aug-2021 Accepted Date: Sep 23, 2021 ; Published: 30-Sep-2021, DOI: O
Abstract
Introduction: Breast cancer is a global problem. The incidence of breast cancer is rising in developing countries. As of 2021, breast cancer accounting for 12% of all new annual cancer cases worldwide, according to the World Health Organisation (WHO). Early diagnostic workup and intervention can significantly alter the course of the disease in favour of decreasing morbidity and mortality. Aims and objectives: To highlight the role of the combined modality approach (Full-Field Digital Mammography, Digital Breast Tomosynthesis, Sonomammography) in diagnosing breast lesions in the interpretation of Breast Imaging Reporting and Data system (BI-RADS) score both in diagnostic and screening settings. To diagnose early occult malignant lesions in both screening and diagnostic mammography and also to differentiate malignant lesions from benign pathologies. Settings and Design: A prospective longitudinal study was conducted from January 2019 to September 2019 (9 months) in the Department of Radio-diagnosis, Andhra Medical College, King George Hospital, Visakhapatnam, India using a Digital Mammography machine which was followed by Sonomammography. Materials and Methods: 880 women who presented to the department of Radiodiagnosis for screening mammography without symptoms and diagnostic mammography with various symptoms were evaluated with Full-Field Digital Mammography (FFDM), Sonomammography/Ultrasonography (USG), and Digital Breast Tomosynthesis (DBT) when indicated. Clinical findings, imaging findings based on BI-RADS, and histopathological findings were correlated and conclusions were drawn for the combined approach in our study. Variables: Age, Family history, Breast tenderness, Palpable abnormality/Lump, Nipple discharge. Results: A total of 880 women were enrolled in the study. The majority came for screening mammography and was in the age group of 40 to 49 years. Out of 880 examined 293 (33.3%) were diagnosed as benign and 45(5.5%) as malignant lesions, and diagnostic accuracy for BI-RADS 4, 5, and BI-RADS3 (upgraded) was found to be 92.85% through this combined modality approach when correlated with histopathological examination. Conclusion: Combination of FFDM, DBT, and USG/Sonomammography significantly increased sensitivity (92%), specificity (100%), positive predictive value (100%) and decreased false-positive rates and also increased the diagnostic confidence compared to the individual modality. This combined modality approach is beneficial in significantly decreasing the callbacks and unnecessary surgical interventions in selective cases. Recommendations: The ACR (American College of Radiology) and SBI (Society of Breast Imaging) recommend that women start getting annual mammograms at age 40 and continue as long as they are in good health.
Keywords
Benign and malignant breast lesions, BI-RADS, Combined modality approach (FFDM, DBT, USG)
Introduction
Breast cancer is the most common female cancer in India with a projected number of cases in 2025 to be approximately 2,32,832 as reported by the National Centre for Disease Informatics and Research governed by the Indian council of medical research [1].
Early detection increases the chances of survival, decreases the cost of health care and morbidity in this subset of the population. The gold standard diagnostic approach is through triple assessment that comprises clinical examination, imaging, and needle biopsy [2].
At present, there are three diagnostic modalities for imaging that are widely used in conjunction with a physical examination. Mammography, Magnetic Resonance Imaging (MRI), and Ultrasonography (USG). Mammography uses low dose X-rays for imaging and the sensitivity of this method is around 75% [3,4]. Screen film mammography is gradually replaced by Full-Field Digital Mammography (FFDM) [5]. A three-dimensional imaging advancement of FFDM is called DBT, an important tool for cancer screening [6,7]. MRI is another technique with high sensitivity but has low specificity and is not cost-effective. It is time-consuming and is recommended in high-risk patients [8]. Currently, there is a trend of using a combined approach by adding screening ultrasound to mammography. Ultrasound is a safe adjunct screening tool especially in mammographically dense breasts because it is non-invasive, real-time imaging, inexpensive with no radiation exposure.
Several studies have reported the advantage of using the combined modality approach in increasing the sensitivity in breast screening and diagnosis [9,10]. In the present study, we evaluated the combined approach and its correlation with histopathology in the early and accurate diagnosis of breast carcinoma.
Methods
Study Design and Patient Population
This observational prospective, single centred study was carried out at a tertiary care hospital over 9 months. Women referred for screening and diagnostic mammography to the Department of Radiology in Andhra medical college, Visakhapatnam, between January 2019 and September 2019 were enrolled in the study. The procedure was explained to lessen fear and anxiety and informed consent was obtained from all women before the study.
Inclusion Criteria
• All the Asymptomatic (without clinical breast disease) women of age above 40 years
• Women of age <40 with high-risk history
• Symptomatic patients with clinically palpable breast masses, pain, nipple discharge
• Operated cases of breast cancer with a contralateral breast mass
Exclusion Criteria
• Women aged below 40 years
• Ulcerated and fungating mass lesions
• Post-trauma patients
• Male population
Evaluation Criteria
The study population was divided into screening and diagnostic mammography groups based on the presentation of the case. Screening cases included asymptomatic women aged >40 years presenting for breast cancer screening along with women who had already undergone treatment for breast cancer and were on yearly follow-up and also their family members who come under high risk. Diagnostic cases included women presenting with breast complaints such as nipple discharge, palpable lump, and pain in the breast.
Cases were evaluated according to ACR guidelines edition 2013 for breast density and age. Mediolateral Oblique (MLO) and Craniocaudal (CC) views were obtained for FFDM, while for tomosynthesis only MLO view was used. Additional views or spot compression views were obtained where ever appropriate as the extremely dense breasts lowers the sensitivity of mammography. We combined sonomammography with screening mammography to increase diagnostic confidence. The images were interpreted at the workstation. BI-RADS score was assigned to each study. The clinical details were correlated and the final diagnosis was drawn from the FNAC/histopathological examination.
Breast Imaging and BI-RADS Grading
Mammography in all patients included in this study was carried out on Fujifilm Digital Mammography System AMULET Innovality in the Department of Radiodiagnosis and Imaging, Andhra Medical College, India, which was followed by Sonomammography on Samsung RS 80A MODEL, machine using a linear array (5 MHz-12 MHz) and convex array (2 MHz-5MHz) transducers.
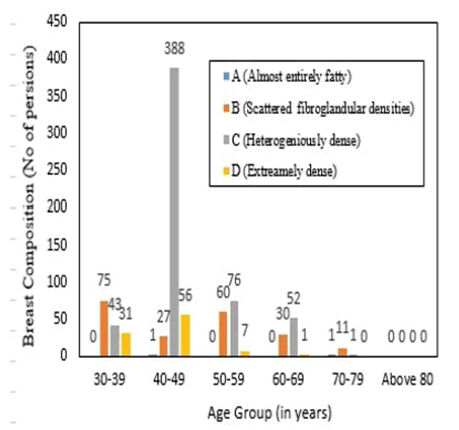
Mammograms were interpreted according to the Breast Imaging Reporting and Data system (BI-RADS) diagnostic categories on a five-point scale, with BI-RADS 1 (negative), 2 (benign finding), 3 (probably benign), 4a (low suspicion for malignancy) 4b (moderate suspicion for malignancy) 4c (high suspicion for malignancy), and 5 (highly suggestive of malignancy). Breast density grades were also determined according to ACR BI-RADS by dividing into 4 subcategories: A (almost entirely fatty), B (scattered fibroglandular tissue), C (heterogeneously dense), D (extremely dense breast which lowers the sensitivity of mammography).
Statistical Analysis
Descriptive statistics were used to represent the data.
Results
Baseline Characteristics
Mammography was performed in 880 patients, screening mammography was performed in 630 (71.5%), and diagnostic mammography in 250 (28.4%) cases. The ages of the patients ranged from 30-80 years. Among 880 patients, 2.5% (22) of cases were of high risk and the majority (10) of them fell in the age group of 40-49, six in the age group of 50-59 years, three each in the age group of 30-39 years and 60-69 years.
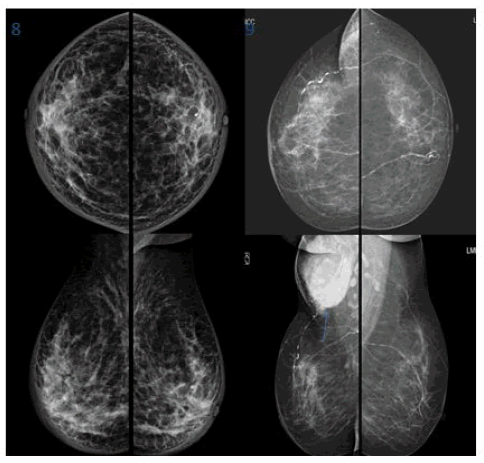
Mammographic and Radiological Diagnosis of the Breast Lesions
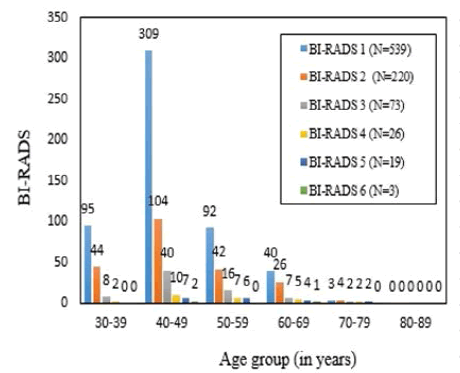
Among the 880 patients, 61.2% (539) were normal and 33.3% (293) were diagnosed as benign/probably benign breast disease (BI-RADS 2 and 3). Forty-five cases were diagnosed as suspicious for carcinoma or highly suggestive of carcinoma of the breast (BI-RADS 4 and 5) and three were known biopsy-proven cases (BI-RADS 6). Breast density grades were also categorized based on age. Among 880 cases 95 (10.79%) had dense breasts, 580 (65%) had heterogeneously dense breasts, 203 (23%) had scattered fibro glandular tissue and 2 (0.22%) had predominantly fatty breasts (Table 1, Figure 1, and Figure 2).
| Age group (years) | BI-RADS 1 | BI-RADS 2 | BI-RADS 3 | BI-RADS 4(N=26) | BI-RADS 5 | BI-RADS 6 | ||
|---|---|---|---|---|---|---|---|---|
| (N=539) | (N=220) | (N=73) | 4a (7) | 4b (9) | 4c (10) | (N=19) | (N=3) | |
| 30-39 Breast density | 95 | 44 | 8 | 1 | 0 | 1 | 0 | 0 |
| 74D/21C | 30D/14C | 6C/1B/1D | 1C | - | 1C | - | - | |
| 40-49 Breast density | 309 | 104 | 40 | 4 | 3 | 3 | 7 | 2 |
| 279C/20D/10B | 71C/25D/8B | 26C/5B/8D/1A | 2C/2D | 3C | 2C/1D | 4B/3C | 2C | |
| 50-59 Breast density | 92 | 42 | 16 | 2 | 3 | 2 | 6 | 0 |
| 49C/43B | 9B/5D/28C | 11C/4B/1D | 2C | 1B/2C | 1B/1C | 2B/3C/1D | - | |
| 60-69 Breast density | 40 | 26 | 7 | 0 | 1 | 4 | 4 | 1 |
| 25B/15C | 26C | 7C | - | 1C | 1B/2C/1D | 4B | 1C | |
| 70-79 Breast density | 3 | 4 | 2 | 0 | 2 | 0 | 2 | 0 |
| 2B/1A | 4B | 1C/1B | - | 2B | - | 2B | - | |
| >80 | 0 | 0 | 0 | - | 0 | - | 0 | 0 |
Benign Lesions
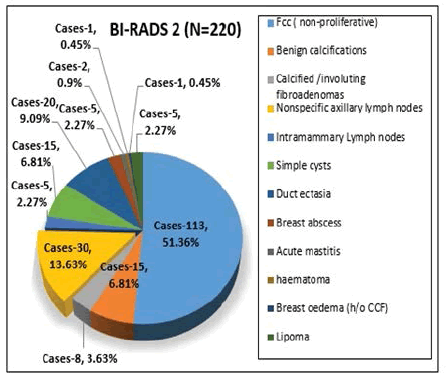
Most of the women with benign breast lesions presented with focal tenderness, palpable abnormality, and nipple discharge. Among the 220 benign cases, (BI-RADS 2) non-proliferative type of Fibrocystic Changes (FCC) seen especially in 40-50 years age group is the commonest in our study followed by benign calcifications, non-specific axillary lymph nodes, breast abscess, mastitis, lipoma, breast edema, and axillary hematoma.
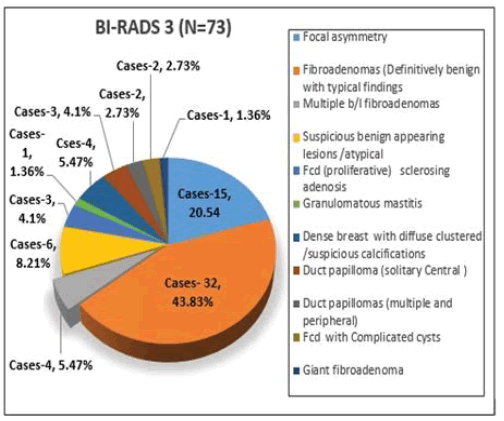
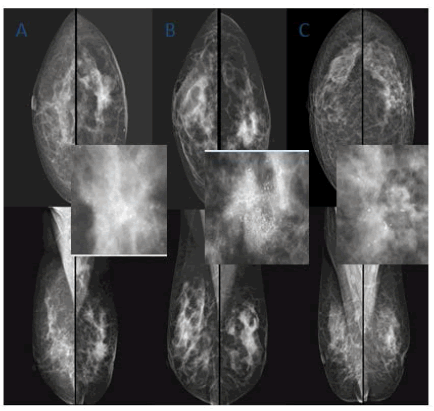
Among the 73 cases categorized as BI-RADS 3, the most common lesions were fibroadenomas followed by, focal asymmetry, suspicious benign-looking lesions, proliferative FCC (sclerosing adenosis), duct papillomas, suspicious calcifications, FCC with complicated cysts, Granulomatous Mastitis, Giant Fibroadenoma (Table 2, Table 3, Figure 3, and Figure 4).
| Radiological diagnosis | No. of Cases | Percentage (%) |
|---|---|---|
| BI-RADS 2 (N=220) | ||
| FCC (non-proliferative) | 113 | 51.36 |
| Benign calcifications | 15 | 6.81 |
| Calcified/involuting fibroadenomas | 8 | 3.63 |
| Nonspecific axillary lymph nodes | 30 | 13.63 |
| Intramammary Lymph nodes | 5 | 2.27 |
| Simple cysts | 15 | 6.81 |
| Duct ectasia | 20 | 9.09 |
| Breast abscess | 5 | 2.27 |
| Acute mastitis | 2 | 0.9 |
| Haematoma | 1 | 0.45 |
| Breast oedema (h/o CCF) | 1 | 0.45 |
| Lipoma | 5 | 2.27 |
| Radiological diagnosis | No. of Cases | Percentage (%) |
|---|---|---|
| BI-RADS 3 (N=73) | ||
| Focal asymmetry | 15 | 20.54 |
| Fibroadenomas (Definitively benign with typical findings) | 32 | 43.83 |
| Multiple B/L Fibroadenomas | 4 | 5.47 |
| Suspicious benign-appearing lesions/atypical | 6 | 8.21 |
| FCC proliferative/sclerosing adenosis | 3 | 4.1 |
| Granulomatous mastitis | 1 | 1.36 |
| Dense breast with diffuse clustered/suspicious calcifications | 4 | 5.47 |
| Duct papilloma (solitary Central) | 3 | 4.1 |
| Duct papillomas (multiple and peripheral) | 2 | 2.73 |
| FCC with Complicated cysts | 2 | 2.73 |
| Giant Fibroadenomas | 1 | 1.36 |
Short-Interval follow-up for BI-RADS 3
73 cases of BI-RADS 3 were reassessed and followed up and depending upon the characteristics they were reclassified. Details are tabulated in (Table 4).
| BI-RADS 3 | Procedures are done radiological and surgical | Cytology/Histopathology report | Follow up BI-RADS 6 months (Upgrade/Downgrade) | Further, follow up 1 year/2 years/3 years |
|---|---|---|---|---|
| Focal asymmetry (15) | NA (Not Applicable) | NA | Stable (9) | Follow-up |
| Resolved BI-RADS 2 (6) | Routine screening | |||
| Definitively benign typical fibroadenomas (32) | NA | NA | Stable | Follow-up |
| Suspicious benign-appearing (6) | Reassessed and reclassified processed for biopsy | Malignant (3) | BI-RADS 4 | Operated |
| The rest of the lesions are benign (3) | Stable | Follow-up | ||
| Sclerosing adenosis (3) | NA | NA | Stable | Follow-up |
| Complicated cysts (2) | USG guided fluid aspiration | Infective | BI-RADS 2 | Routine screening |
| Duct papilloma (solitary central) (3) | Secretions | Benign | BI-RADS 2 | Follow-up |
| Multiple peripheral duct papillomas (2) | Microdochectomy done | Benign | BI-RADS 2 | Follow-up |
| Granulomatous mastitis (1) | Reassessed & reclassified processed for biopsy | Malignant (1) | BI-RADS 4 | Operated |
| Diffuse Clustered/suspicious calcifications (4) | NA | NA | Stable | Follow-up |
| Giant fibroadenoma | Reassessed and proceeded for biopsy | Benign | BI-RADS 3 | Operated |
Malignant Lesions
Among the 45 malignant cases, most of the women presented with palpable mass and tenderness, except one female who is asymptomatic and came for screening mammography. The majority were in the age groups of 40-50 years. The Majority of the mass lesions are single and more than 1 cm in size with irregular shape except for 7 cases where the margins were smooth and mass lesions were well circumscribed and later they were diagnosed as lymphomas, phyllodes, and invasive duct cell carcinoma on Histopathological correlation. Three cases were less than 1 cm and were easily diagnosed by the microcalcifications, associated skin thickening, and mild nipple retraction. In 4 cases, along with malignant lesions, there are few probably benign lesions in both breasts. Follow up done for other benignlooking lesions and found stable (Table 5).
| Radiological Diagnosis | Size >1c | Shape and margins | Quadrant | Right Breast | Node possitve | Calcified | Associated changes | Single | Multiple | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Well circumscribed | Irregular | Obscured | mic.lobulated | Indistinct | Spiculated | UO | UI | LI | RA | LO | ST | NR | AD | |||||||
| BI-RADS 4 (N=26) | 3 | 1 | 25 | 1 | 4 | 8 | 7 | 11 | 1 | 7 | 7 | 0 | 13 | 13 | 8 | 17 | 13 | 17 | 26 | 3 |
| BI-RADS 5 (N=19) | 0 | 5 | 14 | 4 | 9 | 2 | 4 | 12 | 3 | 1 | 2 | 1 | 4 | 15 | 6 | 14 | 16 | 14 | 19 | 1 |
| BI-RADS 6 (N=3) | 0 | 1 | 2 | 0 | 1 | 1 | 1 | 0 | 0 | 2 | 1 | 0 | 3 | 0 | 1 | 3 | 3 | 3 | 3 | 0 |
| Total | 3 | 7 | 41 | 5 | 14 | 11 | 12 | 23 | 4 | 10 | 10 | 1 | 20 | 28 | 15 | 34 | 32 | 34 | 48 | 4 |
Histopathological Diagnosis of Malignant Lesion
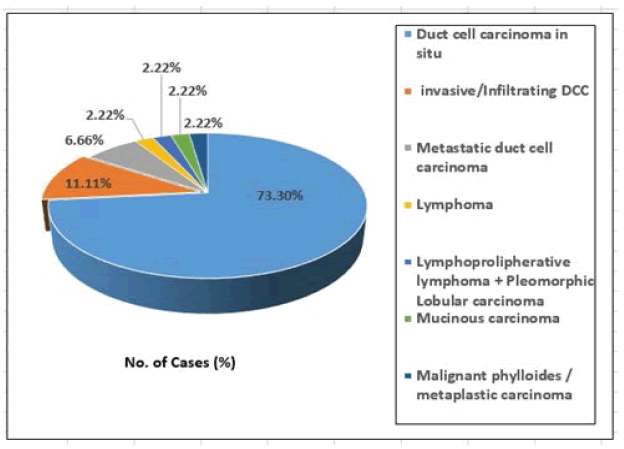
The pathological findings of malignant lesions revealed the majority to be duct cell carcinoma in situ (33/45), followed by invasive/infiltrating (5/45), metastatic duct cell carcinoma (3/45), and one each of lymphoma, lymphoproliferative lymphoma and pleomorphic lobular carcinoma, mucinous carcinoma, malignant phyllodes/metaplastic carcinoma (Figure 5).
Mammography findings were correlated with USG and DBT in all cases and assigned BI-RADS grade based on a combined modality approach. All the malignant (BI-RADS 4 and BI-RADS 5) and upgraded probably benign cases (BI-RADS 3) after reassessment/Reclassification were sent for histopathology. The results are tabulated in Table 6.
| Breast imaging by FFDM/DBT/USG | Histo-pathology | ||||
|---|---|---|---|---|---|
| Findings | On screening mammography | On diagnostic mammography | Total cases | Malignant | Benign |
| Malignant BI-RADS 4 and 5 | 1 | 44 | 45 | 45 (true positive) | 0 (false positive) |
| Probably benign BI-RADS3 (suspicious After reassessment) | 8 | 0 | 8 | 4 (false negative) | 4 (true negative) |
Table 6 shows the correlation of combined modality diagnosis with histopathology. Using this data, the sensitivity, specificity, positive predictive value, and negative predictive value, and diagnostic accuracy were calculated, the values were 91.83%, 100%, 100%, 50%, and 92.85% respectively.
Few benign lesions (case 1-case 9) and few malignant lesions (case 10-case 20) that are diagnosed by our combined approach are represented with figures below.
Case Studies
Benign breast lesions:
1. Case 1: FCC: a 48-year-old woman came for evaluation of pain (Figure 6).
Figure 6. Digital Mammography (DM): Breast composition-Heterogeneously dense breasts-Category C (Cat. C). An isodense lesion with a hypodense rim whose margins are obscured by adjacent fibroglandular tissue was noted in the upper outer quadrant of the right breast. USG: A well-defined clear cystic lesion with posterior acoustic enhancement. Few small fibrocystic changes are also seen in both breasts. BI-RADS 3. USG guided aspiration: FCC
2. Case 2: Solitary Fibroadenoma: 45-year-old female came with a lump in the right breast (Figure 7).
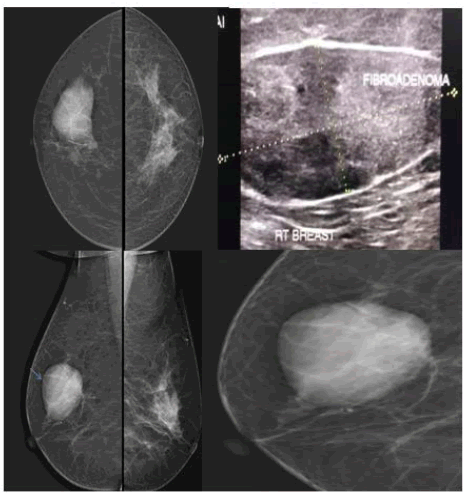
Figure 7. DM: breast composition-scattered fibroglandular tissue (Category B). A Well circumscribed dense oval solitary mass lesion in the upper outer quadrant of Rt breast. USG: Well defined, large oval isoechoic solid lesion wider than tall with thick echogenic pseudocapsule seen in outer quadrant at 9 o’clock position on USG s/o Fibroadenoma-BI-RADS3
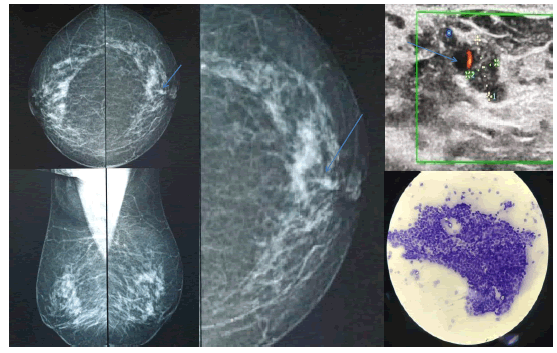
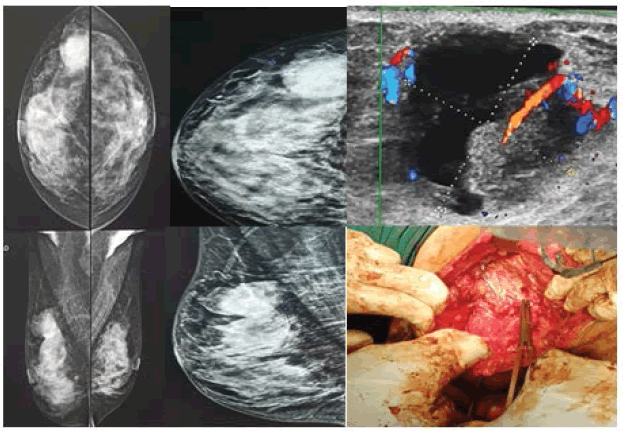
3. Case 3: Giant fibroadenoma: 36-year-old female came with a lump in the right breast (Figure 8).
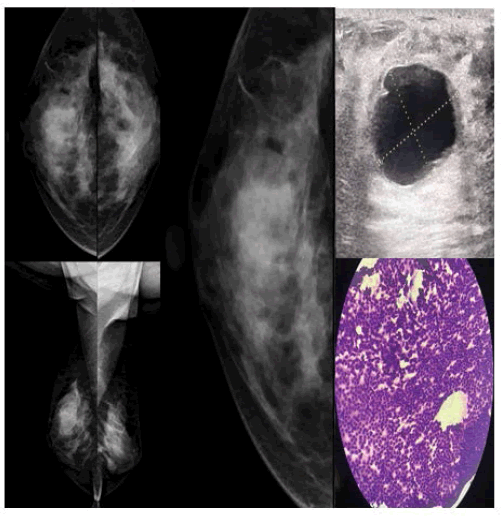
Figure 8. Digital Mammography (DM): Breast composition-Dense breast (cat D). Showing Large (5.5 cm × 3.4 cm in size) well-circumscribed, round iso to a hyperdense mass lesion in the lower outer quadrant in the mid and posterior portion of Right breast. USG: well-defined hypoechoic lesion with more peripheral vascularity on colour Doppler-BI-RADS 3. After reassessment, Upgraded to BI-RADS 4a and proceeded for biopsy. Histopathology revealed Giant Fibroadenoma
4. Case 4: Central solitary duct papilloma: 68-year-old female came with left nipple discharge (Figure 9).
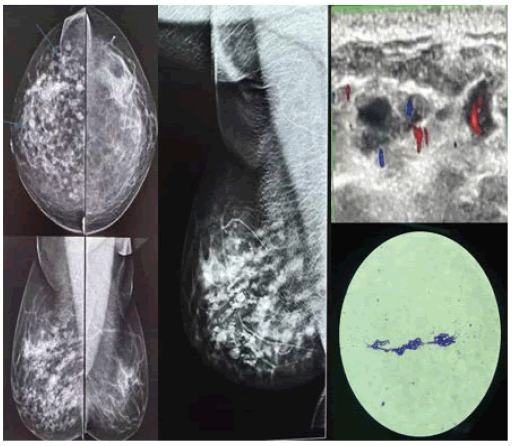
5. Case 5: Unilateral Duct ectasia with multiple papillomas: 45-year-old female presented with pain and nipple discharge (Figure 10).
Figure 10. Digital Mammography (DM): Breast composition-Cat B. Right breast showing dilated ducts with nodular appearance- Unilateral Duct ectasia. USG: Multiple duct ectasia with inspissated secretions within and colour Doppler showing vascular pedicle-BI-RADS-3. Microdochectomy did and sent for cytopathology: Duct ectasia with papillomas
6. Case 6: 53-year-old. k/c/o ca cervix post-chemotherapy post-RT Mastitis and its follow up (Figure 11).
7. Case 7: Breast abscess: 33yr old female came with a lump in the left breast and pain (Figure 12).
Figure 12. Digital Mammography (DM): Heterogeneously dense breast showing ill-defined dense lesion predominantly in the retro areolar region in the mid and anterior portion of the left breast with few enlarged axillary lymph nodes. USG of left breast showing ill-defined hypoechoic area with thick moving internal echoes within. U/S guided aspiration confirmed breast abscess- BI-RADS 2
8. Case 8 and 9: Oedema and axillary hematoma (Figure 13).
Malignant Breast Lesions
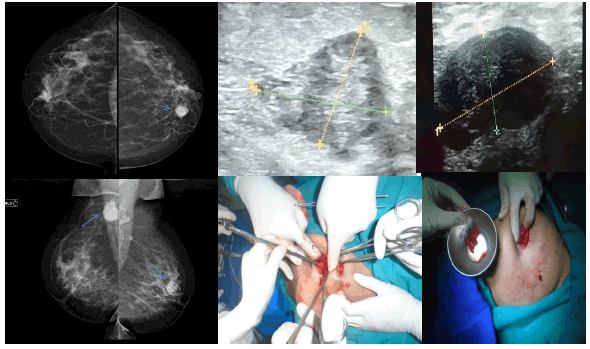
9. Case 10: Complex cyst: 39-year-old female came with a c/o lump and pain in her right breast (Figure 14).
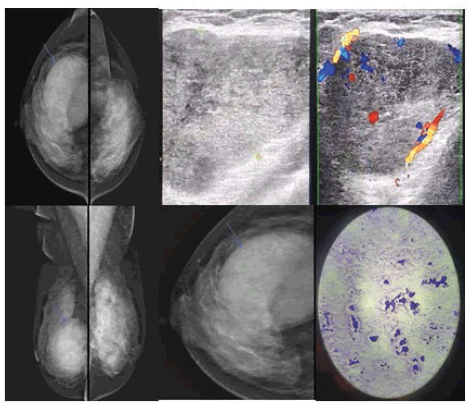
Figure 14. Digital Mammography (DM): Breast composition-Cat C. Right breast showing well-circumscribed dense mass lesion in the posterior portion of the upper outer quadrant with partially obscured margins but on tomosynthesis margins are well delineated and in USG appearing as a complex cystic mass lesion with mural nodule showing colour uptake on doppler study-BI-RADS 4c. Histopathology revealed Fibroadenosis with DCC
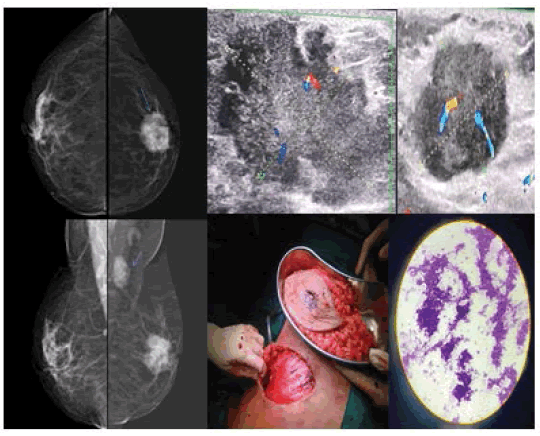
10. Case 11: Duct cell carcinoma: 55-year-old female came with a lump in her left breast (Figure 15).
Figure 15. DM: Breast composition-Cat B. Left breast showing irregular large micro lobulated dense mass lesion in the retro areolar region associated with architectural distortion, adjacent skin thickening, nipple retraction, and significantly enlarged left axillary lymph nodes. USG showing irregular large lobulated solid hypoechoic lesion with central vascularity on Doppler and enlarged left axillary lymph nodes of same morphology. BI-RADS 5 Histopathology-DCC
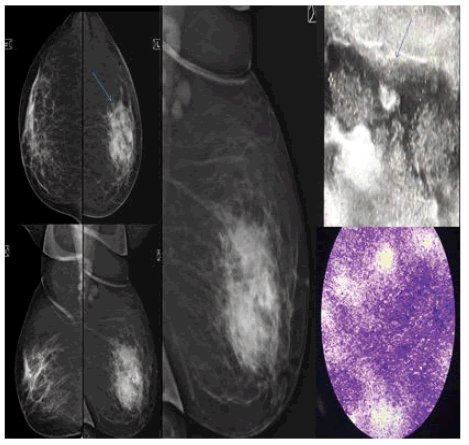
11. Case 12: Mucinous Carcinoma: 59-year-old female came with a lump in her left breast (Figure 16).
Figure 16. Digital Mammography (DM): Breast composition-cat B. Left breast showing an irregular dense mass lesion with indistinct margins noted in the upper inner quadrant in anterior portion with significant B/L axillary lymph nodes largest seen in the right axilla. USG: showing small relatively well-defined lobulated hypo to an isoechoic mass lesion in the left breast with well-defined enlarged hypoechoic largest lymph node in right axilla-BI-RADS 5. Histopathology- Mucinous
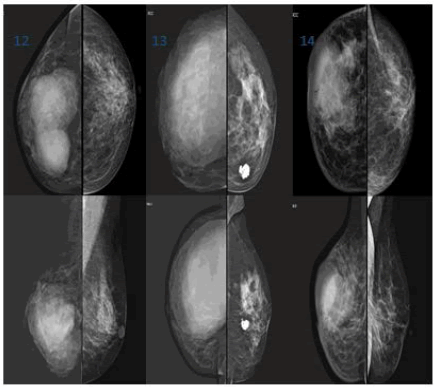
12. Case 13-15: NHL/Phylloides/Metastasis (Figure 17).
Figure 17. Case 12: Lymphoma.Well circumscribed lobulated dense mass lesion with obscured margins in the inner lower quadrant of right breast, non-calcified and node-negative; Case 13: Malignant phyllodes. Large well-circumscribed dense probably cystic mass lesion noted in upper outer quadrant involving almost entire right breast-sparing the inner quadrant (on USG large complex cyst with a solid component) and left breast showing popcorn calcification/involuting calcified fibroadenoma; Case 14: Metastatic DCC. Irregular/ill-defined dense mass lesion with obscured margins in upper outer quadrant of the right breast with, associated features like skin thickening and nipple retraction. Node negative mass with micro-calcifications which are pleomorphic
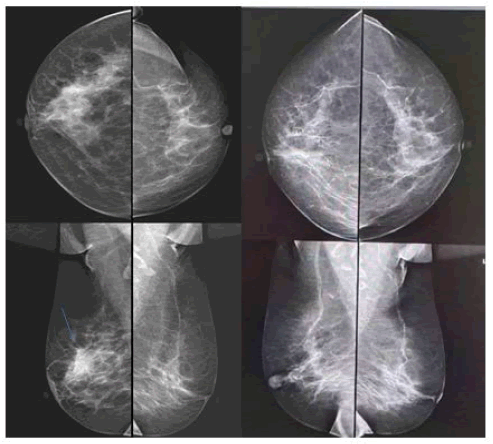
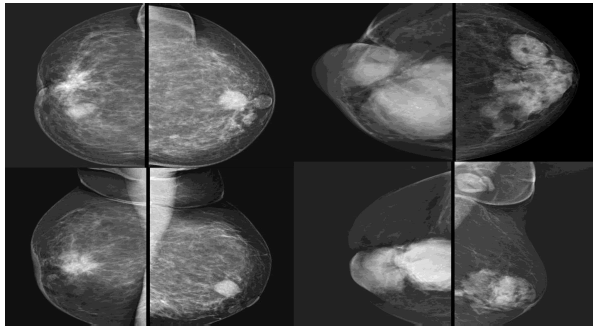
13. Case 16 and 17: Multiple lesions (Figure 18).
Figure 18. Case15: Right breast showing suspicious /probably benign lesion adjacent to the irregular spiculated breast mass lesion (DCC on histopathology) with associated features. The left breast shows a small probably benign lesion in the retro areolar region. Case16: Right breast showing well-circumscribed lesions one overlapping the other (DCC on histopathology) with associated features and left breast showing sclerosing adenosis with significant enlarged left axillary lymph nodes
14. Case 18-20: Malignant calcifications (Figure 19).
Discussion
Mammography screening is the only method currently considered suitable for mass screening of asymptomatic women. It is the best modality for screening in fatty breasts and elderly women. It is accurate in picking up microcalcifications before the development of a mass lesion. However, mammography in standalone settings in dense breasts has disadvantages like low sensitivity and high false-positive rates. Additionally, DBT offers several merits like minimizing the effect of tissue overlap, provides better visualization, improves tissue contrast, margin visibility, and provides image details. In preoperative local staging, USG is a better predictor of tumour size compared to mammography as it aids to detect intraductal tumour extension and satellite foci. Because USG is easily available, cost-effective, and present in all the centres where FFDM is available, the advantage of a combination of mammography along with USG and DBT is considered in diagnosis and screening.
Even though the combination of DBT with an FFDM increases the risk of radiation, this risk is within the acceptable limits set by U.S. Food and Drug Administration (FDA) [11,12]. In diagnostic settings, DBT compared to FFDM provides superior quality images especially in dense breasts and there is a significant fall in recall rates with the combined approach of diagnosis with DBT, FFDM [13-16].
USG is of prominence in characterizing lesions detected by mammography, especially the features associated with malignancy like multicentricity or multifocality of lesions, ductal dilatation, and features inaccessible to mammography like lymph nodes and in differentiating solid from cystic lesion. USG is safe in pregnant and lactating women. In Sonomammography, certain features have high predictive values for malignancy like irregular shape, contour, extensive hypoechogenicity, surrounding echogenic halo, central vascularity, and distortion of surrounding tissue [17].
Early screening and diagnosis of breast lesions and categorization into different groups using BIRADS is helpful inaccurate management of the breast lesions. In our study on screening mammography and diagnostic mammography, we diagnosed one early occult malignant lesion out of 630 screening cases and differentiated 45 malignant lesions from benign. We also found that the Management of BI-RADS 3 is challenging which needs complete diagnostic workup with reassessment/reclassification and further follow-up in case of suspicion.
In our study, it was found that combined evaluation of malignant masses with mammography and sonomammography improved the diagnostic accuracy. The combined role of two modalities has been described to be superior in differentiating benign from malignant lesions by many authors earlier [18,19]. Several reports have suggested the high sensitivity of combined mammographic and USG in the diagnosis of symptomatic patients and screening of asymptomatic women with sensitivity ranging from 87%-100% [20-22]. Their findings are comparable with our study. We found that FFDM along with DBT when combined with USG yielded significant improvement in sensitivity and specificity with values of 91.83% and 100%, respectively.
The factors that influence the early diagnosis of breast cancer in Indian women, to note a few are the socio-economic status, literacy, geographic distribution, and access to medical care. So, as health care professionals at a tertiary care hospital, we could able to make use of the opportunity to screen the asymptomatic women and also to investigate all the symptomatic women by combined modality approach which significantly increased cancer detection rate.
The limitation of the study was a very short period of follow-up.
Conclusion
Digital mammography, tomosynthesis, and sonomammography are complementary to each other in the evaluation of breast lesions and are not substitutes to each other. They have their individual advantages in characterizing various signs of malignancy and put together, increase the diagnostic accuracy. This combined modality approach is of utmost importance in the early diagnosis of smaller lesions especially in dense breasts which helps in prompt management and a significant reduction in breast cancer-related morbidity and mortality.
Declarations
Acknowledgements
My special acknowledgements to Dr P Bujjibabu MD, Professor and HOD of Radiodiagnosis, Andhra Medical College, Visakhapatnam, and to Dr M. Umamaheswar Rao MD, Professor and HOD of Radiodiagnosis, AMC, Visakhapatnam.
My sincere thanks to all the women who participated and cooperated with us while taking both screening and diagnostic Mammography.
References
- Mathur, Prashant, et al. "Cancer statistics, 2020: Report from national cancer registry programme, India." JCO Global Oncology, Vol. 6, 2020, pp. 1063-75.
- Adam, Andy, et al. "Allison’s Diagnostic Radiology." Churchill Livingstone: Edinburgh, Scotland, Vol. 5th ed. 2008.
- Nikolova, Natalia K. "Microwave imaging for breast cancer." IEEE Microwave Magazine, Vol. 12, No. 7, 2011, pp. 78-94.
- Autier, Philippe, and Mathieu Boniol. "Mammography screening: A major issue in medicine." European Journal of Cancer, Vol. 90, 2018, pp. 34-62.
- Shtern, F. "Digital mammography and related technologies: A perspective from the National Cancer Institute." Radiology, Vol. 183, No. 3, 1992, pp. 629-30.
- Rafferty, Elizabeth A. "Digital mammography: Novel applications." Radiologic Clinics of North America, Vol. 45, No. 5, 2007, pp. 831-43.
- Lewin, John M., and Loren Niklason. "Advanced applications of digital mammography: Tomosynthesis and contrast-enhanced digital mammography." Seminars in Roentgenology, Vol. 42, No. 4, 2007, pp. 243-52.
- Morrow, Monica, Janet Waters, and Elizabeth Morris. "MRI for breast cancer screening, diagnosis, and treatment." The Lancet, Vol. 378, No. 9805, 2011, pp. 1804-11.
- Chae, Eun Young, et al. "Evaluation of screening whole‐breast sonography as a supplemental tool in conjunction with mammography in women with dense breasts." Journal of Ultrasound in Medicine, Vol. 32, No. 9, 2013, pp. 1573-78.
- Taori, Kishor, et al. "Evaluation of breast masses using mammography and sonography as first line investigations." Vol. 3, No. 1, 2013.
- Uematsu, Takayoshi. "The emerging role of breast tomosynthesis." Breast Cancer, Vol. 20, No. 3, 2013, pp. 204-12.
- Feng, Steve Si Jia, and Ioannis Sechopoulos. "Clinical digital breast tomosynthesis system: Dosimetric characterization." Radiology, Vol. 263, No. 1, 2012, pp. 35-42.
- Andersson, Ingvar, et al. "Breast tomosynthesis and digital mammography: A comparison of breast cancer visibility and BIRADS classification in a population of cancers with subtle mammographic findings." European Radiology, Vol. 18, No. 12, 2008, pp. 2817-25.
- Gur, David, et al. "Digital breast tomosynthesis: observer performance study." American Journal of Roentgenology, Vol. 193, No. 2, 2009, pp. 586-91.
- Hakim, Christiane M., et al. "Digital breast tomosynthesis in the diagnostic environment: A subjective side-by-side review." American Journal of Roentgenology, Vol. 195, No. 2, 2010, pp. W172-76.
- Noroozian, Mitra, et al. "Digital breast tomosynthesis is comparable to mammographic spot views for mass characterization." Radiology, Vol. 262, No. 1, 2012, pp. 61-68.
- Chen, S‐C., et al. "Analysis of sonographic features for the differentiation of benign and malignant breast tumors of different sizes." Ultrasound in Obstetrics and Gynecology: The Official Journal of the International Society of Ultrasound in Obstetrics and Gynecology, Vol. 23, No. 2, 2004, pp. 188-93.
- Sudharani, B, et al. "Correlation between sonomammography and mammography in the evaluation of breast lesions." IOSR Journal of Dental and Medical Sciences, Vol. 15, No. 4, 2016, pp. 13-20.
- Beerappa, Jaipal R., S. Balu, and N. L. D. Kumar. "Mammographic and sonomammographic evaluation of breast masses with pathological correlation: A prospective original study." International Journal of Anatomy, Radiology and Surgery, Vol. 5, No. 3, 2016, pp. 9-12.
- Moss, Hilary A., et al. "How reliable is modern breast imaging in differentiating benign from malignant breast lesions in the symptomatic population?" Clinical Radiology, Vol. 54, No. 10, 1999, pp. 676-82.
- Shetty, Mahesh K., Yogesh P. Shah, and Ralph S. Sharman. "Prospective evaluation of the value of combined mammographic and sonographic assessment in patients with palpable abnormalities of the breast." Journal of Ultrasound in Medicine, Vol. 22, No. 3, 2003, pp. 263-68.
- Barlow, William E., et al. "Performance of diagnostic mammography for women with signs or symptoms of breast cancer." Journal of the National Cancer Institute, Vol. 94, No. 15, 2002, pp. 1151-59.