Research Article - International Journal of Medical Research & Health Sciences ( 2023) Volume 12, Issue 2
Pulmonary Radiological Findings in COVID-19 Patients
Sander Kola1, Irena Kola2*, Erinda Frroku1 and Erjona Abazaj32Rheumatology Service University Hospital "Mother Teresa", Tirana, Albania
3Institute of Public Health, Tirana, Albania
Irena Kola, Rheumatology Service University Hospital "Mother Teresa", Tirana, Albania, Email: irena.kola@hotmail.com
Received: 20-Jan-2023, Manuscript No. ijmrhs-23-87513; Editor assigned: 23-Jan-2023, Pre QC No. ijmrhs-23-87513(PQ); Reviewed: 28-Jan-2023, QC No. ijmrhs-23-87513(Q); Revised: 05-Feb-2023, Manuscript No. ijmrhs-23-87513(R); Published: 28-Feb-2023
Abstract
Background: COVID-19 is a pandemic infectious disease causing an increase in deaths. The clinical spectrum of this disease ranges from asymptomatic to mild clinical upper respiratory infection, which can progress to an acute respiratory distress syndrome in critically ill patients. Reverse Transcription Polymerase Chain Reaction (RT-PCR) and Computed Tomography (CT) have played important roles in diagnosing the disease. The study aimed to evaluate the damage to lungs during the COVID-19 pandemic by imagery diagnostic methods like CT and x-ray with the suggested objective that imaging plays an important role in the clinical work-up of suspected or confirmed COVID-19 patients. Methods: This is a retrospective and observational study, including the collection and assessment of demographic, laboratory, and clinical data of patients with and without a confirmed diagnosis of Covid-19 infection by RT-PCR, who underwent chest x-ray and CT at the hospital between November 2020 to January 2021. X-ray and CT scans were viewed and analyzed by two blinded consultant radiologists, and were classified as positive or negative and also assessed the clinical severity of patients. The software SPSS version 20.0 were used for analyzing data. A p-value less than 0.05 was considered statically significant. Results: Overall 225 patients, the positivity of COVID-19 by RT-PCR resulted at 85.3%. Males were the most predominant gender and patients over 61 years old appeared the higher number at 47.1%. The fever was the most frequent symptom 82.6% compared to other symptoms of COVID-19. About 36% of patients referred have sputum production 67.5% shortness of breath, and 34% pleuritic pain. The maximum of lungs involved peaked approximately 11 days from the onset of initial symptoms, p<0.03. Related to the comorbidities, 31.1% referred that they suffer from arterial hypertension. The radiological images of most of the patients resulted in ground-glass opacities and consolidations and peripherical distribution in 67.1%, 56.9%, and 60% respectively radiological investigations indicate that among the 254 patients, 51% had features on both lungs; 9% on the left lung; and 11% on the right lung. The predominantly affected lobe was the right lower lobe 67.5%. Conclusions: RT-PCR test continues to be considered the initial step for diagnosing COVID-19, even though the publications studies reported many false-negative cases for many reasons. Chest X-ray and CT remains the primary imaging modality in patients with all types of respiratory infections, especially during the different wave of COVID-19 in Albania. Moreover, a chest CT demonstrates lower respiratory tract affection. The CT findings in patients confirmed or not confirmed with COVID-19 can help to predict the course of the disease. This can help to manage the patients, and plan the resources more effectively, especially for the use of hospitalization beds in ICU wards, and also, will decrease the spread of disease by providing early time to intervene to isolate patients.
Keywords
COVID-19, Radiological image, Pulmonary impairment
Introduction
COVID-19 is caused by a single-stranded RNA virus named severe acute respiratory syndrome coronavirus. It was named Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) by the International Committee on Taxonomy of Viruses based on phylogeny, taxonomy, and established practice [1,2]. On January 30, 2020, WHO emerged COVID-19 as a pandemic leading to a global public health crisis of unprecedented mortality and morbidity [3]. SARS-CoV-2 is highly contagious and transmissible from person to person [4]. COVID-19 infection results in multiorgan systemic disease, which affects the brain, Gastrointestinal System, heart, and kidneys, either directly or indirectly through the host’s inflammatory response and a hypercoagulable state [5]. Although COVID-19 is most well-known for causing substantial respiratory pathology, it can also result in several extrapulmonary manifestations [6].
The clinical spectrum of this disease ranges from asymptomatic to mild clinical upper respiratory infection, which can progress to an acute respiratory distress syndrome in critically ill patients [7]. In addition, endothelial damage, thrombus inflammation, and dysregulated immune response also contribute to the extrapulmonary manifestations of the disease [8]. Multiple studies have described the chest radiology findings of COVID-19 [9,10]. The sensitivity of chest Computed Tomography (CT), was reported up to 97% [11,12]. During COVID-19, Chest Radiography, and CT, had an important role in the care of patients with COVID-19. In most cases, the positive COVID-19 diagnosis is confirmed by Reverse Transcriptase-Polymerase Chain Reaction (RT-PCR). Chest imaging in patients with moderate or severe clinical symptoms of COVID-19 and a positive RT-PCR test result is been used to evaluate the baseline severity of any lung disease [5]. While imaging in patients with a negative RT-PCR test result can be used as an alternative to evaluating diagnoses despite a persisting clinical suspicion of COVID-19.
In Albania, CT imaging played a significant role, especially in patients with clinical symptoms but gained importance, particularly in patients with false-negative RT-PCR results. The study aimed to evaluate the damage to lungs during the COVID-19 pandemic by imagery diagnostic methods like CT and x-ray with the suggested objective that imaging plays an important role in the clinical work-up of suspected or confirmed COVID-19 patients.
Methods
In this retrospective, observational study, we describe the clinical finding of COVID-19 patients in Hospital University Centre “Mother Theresa”, Tirana, Albania, who were either imaged with a standard chest x-ray, chest CT, or both imagery methods. This study was conducted during the period November 2020 to January 2021, and a total of 225 patients suspected and confirmed of COVID-19 were involved. We have presented the epidemiological, and social-demographic data of included patients who were examined for COVID-19 by RT-PCR method and an illustrative of x-ray and CT findings and a schematic description of typical COVID-19 imaging features.
Patients suspected of having COVID-19 infection who were referred to our hospital were evaluated by the medical physician and referred to the imagery department for evaluation of the chest by CT and x-ray.
RT-PCR was performed with nasal and nasopharyngeal sampling in patients whose clinical symptoms were indicative of COVID-19 infection, and those who had contact with COVID-19 patients.
The chest x-ray was performed using Siemens equipment (90 Kv, time of exposition 0.4 mAs). Chest CT images were with and without contrast and performed during inspiratory breath-hold at the supine position using a 16- detector-row CT scanner (the following series number 66090 Somatom definition AS+CT 2012B FFS). To minimize motion artifacts, patients were instructed on breath-holding; CT images were then acquired during a single breath-hold. All patients’ imaging was reconstructed with a slice thickness of 3.0 mm.
Interpretation of chest images for confirming the suspected cases of COVID-19 and severity assessment of the disease based on imaging findings were assessed blindly by two radiologists with more than ten years of experience in chest CT interpretation. Classification of CT findings was done under the Radiology Society of North America consensus statement on Reporting Chest CT findings Related to COVID-19 [13]. The inclusion criteria included suspected COVID-19 patients with typical symptoms (cough, fever, shortness of breath, myalgia/arthralgia, and headache), and oxygen saturation below 94%. The exclusion criteria consisted of patients having non-viral pneumonia, tuberculosis, asthma, chronic obstructive pulmonary disease, and pulmonary edema.
Study Objectives
The objective of the study is to verify which CT diagnostic method or x-ray examination has the highest effectiveness in the diagnosis of COVID-19 patients.
Admission Criteria
Inclusion criteria patients with and without a confirmed diagnosis of Covid-19 infection by RT-PCR who underwent chest radiography and CT in the hospital.
Exclusion Criteria
Exclusion criteria were patients with lung tumor disease or pulmonary trauma.
Results
In the imagery department for three months are exanimated about 225 patients were with x-ray and CT scans for COVID-19. The demographic data, symptoms, and comorbidities of patients are presented in Table 1. The most predominant gender was male 65.3% (147/225) compared to females 34.7% (78/225). Patients over 61 years old appeared the higher in number 47.1% (106/225), in contrast with other ages. So, the patients 41 years ≤ 60 years old presented in 40.9% (92/225) and patients ≤ 40 years old 12% (27/225). This infection manifested a lot of signs and symptoms. In this study, fever was the most frequent symptom compared to other symptoms of COVID-19. About 82.6% (186/225) of cases referred presence of fever during the first days of infection.
| Variables | Patients (number/%) |
|---|---|
| Gender | |
| Female | 34.7% (78) |
| Male | 65.3% (147) |
| Age | |
| ≤ 40 years old | 12% (27) |
| 41 years ≤ 60 years old | 40.9% (92) |
| >61 years old | 47.1% (106) |
| Symptoms | |
| Fever | 82.6% (186) |
| Cough | 72% (162) |
| Fatigue | 67.1% (151) |
| Headache | 35.5% (80) |
| Sore throat | 18.2% (41) |
| Chills | 33.3% (75) |
| Myalgia/Arthralgia | 44% (99) |
| Diarrhea | 36.9% (83) |
| Sputum production | 36% (81) |
| Shortness of breath | 67.5% (152) |
| Pleuritic pain | 34% (77) |
| Comorbidities | |
| Arterial hypertension | 31.1% (70) |
| Diabetes | 24% (54) |
| Cardiovascular disease | 18.7% (42) |
| Chronic kidney disease | 12% (27) |
| Others | 14.2% (32) |
Cough was referred by 72% (16/225) of patients, fatigue was referred by 67.1% (151/225) of patients, headache by 35.5% (80/225) of patients, sore throat by 18.2% (41/225), chills by 33.3%, and myalgia/arthralgia by 44% (99/225) of patients. Meanwhile, some of the patients have problems with their lungs. Almost of the patients 36% (81/225) referred that have sputum production, more than half of the patients referred 67.5% (152/225) shortness of breath, and 34% (77) referred pleuritic pain. The maximum of lungs involved peaked approximately 11 days from the onset of initial symptoms, p<0.03.
Related to the comorbidities, 31.1% (70/225) of patients referred that they suffer from arterial hypertension, 24% (54/225) suffer from diabetes, 18.7% (42/225) suffer from cardiovascular disease and 12% (27/225) suffer from chronic diseases. Meanwhile, in the category of other, 14.2% of cases we have included all patients with high BMI, patients that suffer from Asthma, and patients with Chronic Obstructive Pulmonary Disease (COPD) (Table 1).
Time interval in days from first symptoms to baseline chest x-ray or CT resulted from 3 days to 10 days with an average of 6.41 ± 2.5 Std. Overall, 225 suspected patients tested for SARS-Cov-2 resulted positive in 85.3% (192/225) of cases and negative in 14.7% (33/225) of cases tested for COVID-19 by RT-PCR. Patients with positive RT-PCR for COVID-19 but negative CT and x-ray resulted in 28.9% (65/225) of patients (24.9% with CT negative and 4% with X-ray negative). While confirming the suspected cases of COVID-19 and severity assessment of the disease based on imaging findings resulted in 71.1% (160/225) of patients. Patients with negative RT-PCR but positive CT were 9.7% and positive x-ray was 4.9%. Patients confirmed positive for COVID-19 by RT-PCR and CT were 65.3% and 5.8% with x-ray positive. All patients did the laboratory tests, resulting in Lymphopenia in 71% of them (<1.0 Giga/l), and 89.3% of them with CRP (>5 mg/l), increased ferritin (>400 µg/l) and prothrombin time (ÃÂ??70%) was seen in 28.8% and 20.9% respectively. Increased LDH (>480 U/l) appeared in more than half of the patients 52.4% (Table 2).
| Variables | Patients (number/%) |
|---|---|
| RT-PCR testing and CT and x-ray | |
| RT-PCR positive | 85.3 (192) |
| RT-PCR negative | 14.7 (33) |
| RT-PCR positive, CT negative | 24.9 (56) |
| RT-PCR positive x-ray negative | 4 (9) |
| RT-PCR negative, CT positive | 9.7 (22) |
| RT-PCR negative, x-ray positive | 4.9 (11) |
| RT-PCR positive, CT positive | 65.3 (147) |
| RT-PCR positive x-ray positive | 5.8 (13) |
| Laboratory test results | |
| Lymphopenia (<1.0 Giga/l) | 71% (160) |
| CRP (>5 mg/l) | 89.3% (201) |
| D-dimer (measured later) (>500 ng/l) | 49.8% (112) |
| Increased ferritin (>400 µg/l) | 28.8% (65) |
| Increased prothrombin time (<70%) | 20.9% (47) |
| Increased LDH (>480 U/l) | 52.4% (118) |
Table 3 shows the CT findings of patients based on the RT-PCR result test. According to the method of examination they have used, most of them are examined by CT in 81.8% of cases. Only 10.7% are examined by x-ray and 7.5% have used both examination methods x-ray and CT. Chest CT images were assessed for the presence of GroundGlass Opacities (GGOs), consolidation, peribronchial vascular distribution, peripherical distribution, per lobular thickening, reticular pattern, and pleural/pericardial effusion.
| Examination | RT-PCR total | RT-PCR negative | RT-PCR positive | p-value |
|---|---|---|---|---|
| %/N | %/N | %/N | ||
| Methods | 225% | 33 | 192 | |
| x-ray | 10.7% (24) | 15.16% (5) | 9.9% (19) | 0.08 |
| CT | 81.8% (184) | 60.6% (20) | 85.4% (164) | 0.002 |
| Both | 7.5% (17) | 24.24% (8) | 4.7% (9) | |
| Imagery findings | ||||
| Ground Glass Opacities (GGO) | 67.1% (151) | 7.9% (12) | 92.1% (159) | 0.04 |
| Consolidation | 56.9% (128) | 21.1% (27) | 78.9% (101) | 0.036 |
| Peribroncho vascular distribution | 33% (74) | 9.5% (7) | 90.5% (67) | 0.03 |
| Peripherical distribution | 60% (135) | - | 60% (135) | 0.004 |
| Perilobular thickening | 10.2% (23) | - | 10.2% (23) | 0.01 |
| Pleural/pericardial effusion | 25% (56) | 1.8% (1) | 98.2% (55) | 0.02 |
| Reticular pattern | 3.1% (7) | - | 100% (7) | 0.6 |
| Pulmonary impairment | ||||
| Right lung | 11% (25) | 36% (9) | 64% (16) | 0.007 |
| Left lung | 9% (20) | 35% (7) | 65% (13) | 0.03 |
| Both lung | 51% (115) | 14.8% (17) | 85.2% (98) | 0.003 |
| Right lower lobe | 67.5% (108) | 13% (14) | 87% (90) | 0.038 |
| Right upper lobe | 51.2% (82) | 13.4% (11) | 86.6% (71) | 0.04 |
| Left lower lobe | 55.6% (89) | 20.2% (18) | 79.8% (71) | 0.041 |
| Left upper lobe | 46.2% (74) | 21.6% (16) | 78.4% (58) | 0.045 |
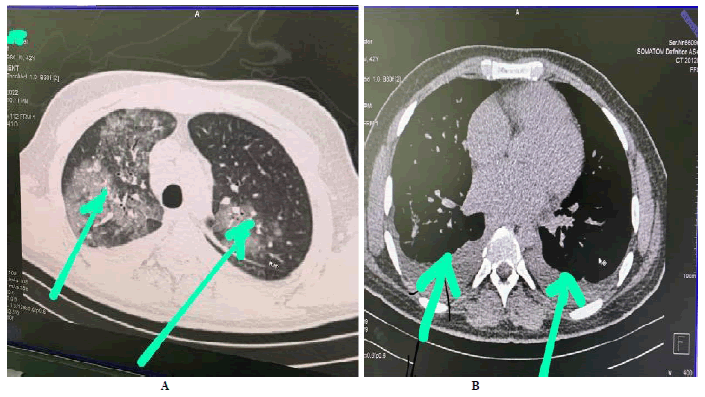
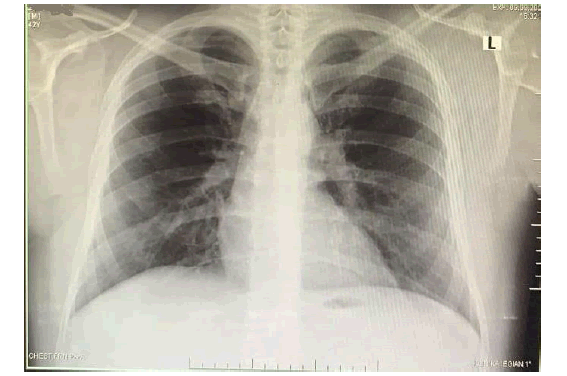
Overall 254 patients confirmed and non-confirmed infected by COVID-19 by RT-PCR showed pneumonia with GGO at 67.1%, consolidation at 56.9%, peribronchial vascular distribution at 33%, peripherical distribution at 60%, per lobular thickening at 10.2%, Pleural/pericardial effusion in 25%, and reticular pattern in 3.1%. Regarding the pulmonary impairment of 225 patient participants in this study, 71.1% (115/225) had implications on both lungs; 9% (20/225) on the left lung; and 11% (25/225) on the right lung. Among the 160 patients confirmed by RT-PCR and CT-positive for COVID-19, the right lower lobe appears to be more damaged at 67.5% (Table 3). We found a significant association in almost all imagery findings except the reticular pattern for the patients with RT-PCR positive and negative with a p-value less than 0.05. Also, the pulmonary impairment of the right-left or both lungs was found a significant association value of less than 0.05 (Figure 1-4)
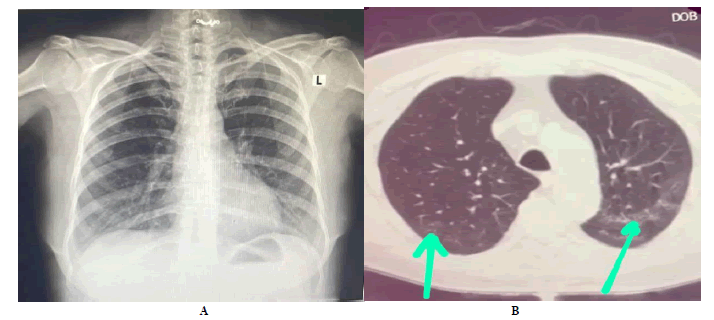
Figure 3. Chest X-ray and CT images. A male 58-year-old with signs and symptoms, and confirmed with COVID-19 by RT-PCR. A) xray was done 6 days after infection. It shows minimal bilateral broncho-pneumonic changes without specific interstitial lesions. B) the same patient. Chest CT scan image appears GGO grade 1-2. The scan was done on day 7 after the infection
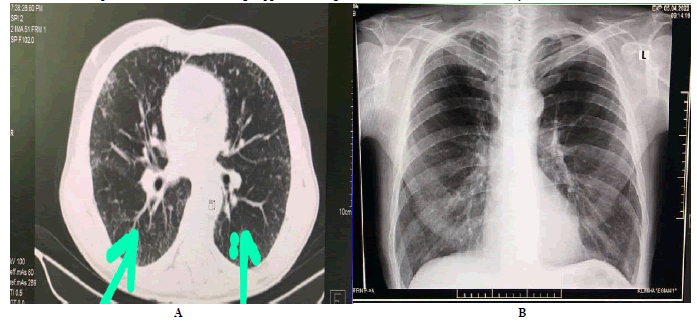
Figure 4. Chest CT and X-ray images. A male 62-year-old with signs and symptoms, and confirmed with COVID-19 by RT-PCR. A) Chest CT scan image appears GGO grade 2 with involvement in both lungs. The scan was done on day 9 after the infection. B) In the same patient, the x-ray was done 7 days after infection. X-Ray shows minimal bilateral broncho-pneumonic changes without specific interstitial lesions
Discussion
The findings of this study appeared that the most predictive patient-related factors of adverse outcomes were age and the presence of significant comorbidity. Male was the most predominant gender affected by covid-19 and patients over 61 years old appeared the higher in number 47.1% in contrast with other ages. Regarding demographic data, gender and age significantly influence clinical severity and this was relevant to other recent publications [14-16]. Patients over 61 years of age had a higher risk of increased clinical severity upon admission compared to other ages (p<0.0001). Related to infection manifested signs and symptoms, fever was the most frequent symptom compared to other symptoms of COVID-19 in 82.6% of cases.
Cough and fatigue were also more referred among our patients. In addition to the lung impairment, most of the patients 36% referred that have sputum production, more than half of the patients referred to 67.5% shortness of breath, and 34% referred to pleuritic pain. These findings were following another study conducted in Albania by Petri et al, on suspected cases of COVID-19 [17].
The maximum of lungs involved peaked approximately 11 days from the onset of initial symptoms, p=0.03. Recent publications have observed that patients with chronic diseases are more susceptible to respiratory failure and death from Covid-19 [18-20]. In this study, arterial hypertension was the most predominant comorbidity among our patients with 31.1% with a significant association of p=0.02. A combination of clinical sing and symptoms with laboratory findings and CT findings can provide valuable information to direct toward a correct diagnosis while waiting for positive or negative confirmation of COVID-19 results by RT-PCR.
Radiographs are usually one of the first investigations performed on suspected pulmonary diseases. They have minimal radiation exposure making repeated imaging relatively safe. Due to the relatively low testing sensitivity of real-time reverse transcription-polymerase chain reaction (RT-PCR) tests (60%-70%) and the global shortage of resources, an increase in medical imaging strategies was needed to detect and diagnose patients with COVID-19 [14]. Fang et al, have reported false-negative RT-PCR tests in patients with CT findings of COVID-19 who eventually tested positive with serial sampling [21]. In addition to this, some studies have listed some essential reasons why radiologic imaging came to aid in the diagnosis of COVID-19. Some of those reasons are; limited testing capacity due to insufficient specimen collection kits, laboratory test supplies, and testing equipment that precluded early widespread testing. On the other hand, all of this is believed to have contributed to the rapid and unchecked transmission of infection within communities by undetected individuals with milder, limited, or no symptoms [12,22]. During the COVID-19 pandemic, chest radiographs and Computed Tomography (CT) were the most common thoracic imaging modality performed and probably the most useful [23]. Chest X-ray is generally the first-line imaging test in patients with suspected or confirmed COVID-19 due to its usefulness, availability, and low cost, though it is less sensitive than Computed Tomography (CT) [24]. The optimal chest X-ray includes Posteroanterior (PA) and lateral projections with the patient standing [25]. On the other hand, chest CT is a more effective test for early detection of COVID-19 pneumonia. CT is easy to perform, fast, readily available and has a high sensitivity. It can provide valuable information for further diagnosis as well as prevention and control of COVID-19 [8].
In this study, we have evaluated the aid of imagery in pulmonary damaging findings during the COVID-19 pandemic, with the suggested objective that imaging plays an important role in the clinical work-up of suspected or confirmed COVID-19 patients.
The positivity of Sars-Cov-2 diagnosis by RT-PCR on 225 suspected patients recruited in this study resulted in 85.3% (192/225). As we mentioned before the time interval in days from first symptoms to baseline chest x-ray or CT resulted from 3 until to 10 days with an average of 6.41 ± 2.5. Patients with positive RT-PCR for COVID-19 but negative CT and x-ray appeared in 28.9% (65/225) of patients (24.9% with CT negative and 4% with x-ray negative). Meanwhile, patients with negative RT-PCR but positive CT results were 9.7%, and those with positive x-ray results were 4.9%. While confirming the suspected cases of COVID-19 and severity assessment of the disease based on imaging findings appears in 71.1% (160/225) of patients. Confirmation of COVID-19 by CT in our study resulted higher compared to another study conducted on the cruise ship “Diamond Princess” where CT screening of 82 asymptomatic patients shows the presence of pneumonia in 54% of tourists [26]. CT was the most significant equipment used in detecting and diagnosing SARS-CoV-2. Some studies have demonstrated a high sensitivity of CT in diagnosing COVID-19 in patients with respiratory symptoms, then RT-PCR tests [11,27-31]. Even though differentiating other viral pneumonia from COVID-19 pneumonia with Computed Tomography (CT) is challenging and complex, CT imaging had a sensitivity of 97% and was considered an essential early detection modality. This was particularly true for patients suffering from persistent clinical suspicions of COVID-19, despite a negative RT-PCR test [32,33]. Some studies have investigated the correlation between pulmonary involvement in Covid-19 infection and clinical severity upon admission [16]. Infections of the lung are very common and can present in different ways. These range from peribronchial nodules and ground-glass opacities to dense consolidation involving the entire lobe. One literature review performed by Lomoro et al found an association between lung ultrasound features and CT findings for GGOs and consolidation in confirmed COVID-19 patients. This could aid the rapid diagnosis and management of COVID-19 pneumonia [34,35]. In general, the clinical and imaging features were concordant with the current literature reports of COVID-19 viral pneumonia [36]. According to the severity of pneumonia, the radiology chest images in this study were focused on the lesion distribution: both lungs, left or right lung; lobes involved: upper, middle, and lower. Based on findings, most of the patients resulted with ground-glass opacities and consolidations and peripheral distribution in 67.1%, 56.9%, and 60% respectively. Also, the imagery findings resulted in peribronchial vascular distribution (33%) per lobular thickening (10.2%), pleural/pericardial effusion (25%), and reticular pattern in 3.1%. In general, the lesions in the lung are usually bilateral, the lower lobes are more commonly affected, and the right middle lobe is the least involved one. Among the 225 patients, 51% had features on both lungs; 11% on the right lung; and only 9% on the left lung. Furthermore, the most affected lobe was the right lower lobe with 67.5%, and also, the left lower lobe resulted with 55.6%. Similar findings were found in some other articles [37,38].
Conclusion
RT-PCR test continues to be considered the initial step for diagnosing COVID-19, even though the publications studies reported many false-negative cases, due to many reasons. The findings of this study show the importance of chest imaging because the RT-PCR test is limited to the upper respiratory tract, and the lack of test kits during the infectious wave prompted medical staff to look into alternative diagnostic methods, such as clinical imaging. Chest X-ray and CT remains the primary imaging modality in patients with all types of respiratory infections, especially during the pandemic wave of COVID-19 in Albania. Moreover, a chest CT demonstrates the lower respiratory tract. The CT findings in patients confirmed or not confirmed with COVID-19 can help to predict the course of the disease. This can help to manage the patients, and plan the resources more effectively, especially for the use of hospitalization beds in ICU wards, and also, will decrease the spread of disease by providing early time to intervene to isolate patients.
Abbreviations
COVID-19Coronavirus disease 2019; CT: computed tomography; RT-PCR: Reverse transcription-polymerase chain reaction; SARS-CoV-2: Severe acute respiratory syndrome coronavirus 2; CRP: C-reactive protein; LDH: lactate dehydrogenase; GGO: Ground-glass opacities;
Acknowledgments
The authors would like to thank the Radiology ward and Medical for providing help during the research
Declarations
Conflict of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Authors’ Contributions
KS and FE designed the study, reviewed the literature, and wrote the article. KI made critical revisions. AE analyzed the data (Statistical Analyses) and made critical revisions. All the authors read and approved the final manuscript.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Competing interests
All authors declare they have no competing interests to be declared.
Ethics Approval and Consent to Participate
This work received Institution approval and informed consent regarding the disclosure of personal data was obtained from all individuals.
References
- Aljondi, Rowa, and Salem Alghamdi. "Diagnostic value of imaging modalities for COVID-19: scoping review." Journal of medical Internet research, Vol. 22, No. 8, 2020. p.19673.
Google Scholar Crossref - Gorbalenya, Alexander E., et al. "The species Severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2." Nature Microbiology, Vol. 5, No. 4, 2020, pp. 536-544.
Google Scholar Crossref - Varadarajan, Vinithra, et al. "Role of imaging in diagnosis and management of COVID-19: a multiorgan multimodality imaging review." Frontiers in Medicine, 2021.
Google Scholar Crossref - Grillet, Franck, et al. "Acute pulmonary embolism associated with COVID-19 pneumonia detected with pulmonary CT angiography." Radiology, Vol. 296, No. 3, 2020, pp. 186-188.
Google Scholar Crossref - Ko, Jane P., et al. "Pulmonary COVID-19: Multimodality Imaging Examples." RadioGraphics, Vol. 40, No. 7, 2020, pp 1893-94.
Google Scholar Crossref - Gupta, Aakriti, et al. "Extrapulmonary manifestations of COVID-19." Nature medicine, Vol. 26, No. 7, 2020, pp. 1017-32.
Google Scholar Crossref - Wu, Zunyou, and Jennifer M. McGoogan. "Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention." JAMA, Vol. 323, No. 13, 2020, pp. 1239-42.
Google Scholar Crossref - Manna, Sayan, et al. "COVID-19: a multimodality review of radiologic techniques, clinical utility, and imaging features." Radiology: Cardiothoracic Imaging, Vol. 2, No. 3, 2020, p. e200210.
Google Scholar Crossref - Kim, Hyungjin, Hyunsook Hong, and Soon H. Yoon. "Diagnostic performance of CT and reverse transcriptase polymerase chain reaction for coronavirus disease 2019: a meta-analysis." Radiology, Vol. 296, No. 3, 2020, pp. E145-E55.
Google Scholar Crossref - Rubin, Geoffrey D., et al. "The role of chest imaging in patient management during the COVID-19 pandemic: a multinational consensus statement from the Fleischner Society." Radiology, Vol. 296, No. 1, 2020, pp. 172-80.
Google Scholar Crossref - Ai, Tao, et al. "Correlation of chest CT and RT-PCR testing for coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases." Radiology, Vol. 296, No. 2, 2020, pp. E32-E40.
Google Scholar Crossref - Fang, Yicheng, et al. "Sensitivity of chest CT for COVID-19: comparison to RT-PCR." Radiology, Vol. 296, No. 2, 2020, pp. E115-E17.
Google Scholar Crossref - Simpson, Scott, et al. "Radiological Society of North America expert consensus document on reporting chest CT findings related to COVID-19: endorsed by the Society of Thoracic Radiology, the American College of Radiology, and RSNA." Radiology: Cardiothoracic Imaging, Vol. 2, No. 2, 2020, p. e200152.
Google Scholar Crossref - Yang, Ran, et al. "Chest CT severity score: an imaging tool for assessing severe COVID-19." Radiology: Cardiothoracic Imaging, Vol. 2, No. 2, 2020, p. e200047.
Google Scholar Crossref - Richardson, Safiya, et al. "Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area." Jama, Vol. 323, No. 20, 2020, pp. 2052-59.
Google Scholar Crossref - Ribeiro, Tatiana FG., et al. "Tomographic score (RAD-Covid Score) to assess the clinical severity of the novel coronavirus infection." Brazilian Journal of Infectious Diseases, Vol. 25, 2021.
Google Scholar Crossref - Petri, Oltiana, et al. "The Epidemiological Situation and Clinical Characteristic Aspect Cause by COVID-19 in Suspected Cases in Albania." Open Access Macedonian Journal of Medical Sciences, Vol. 10, 2022, pp. 1062-67.
Google Scholar Crossref - Bai, Harrison X., et al. "Performance of radiologists in differentiating COVID-19 from non-COVID-19 viral pneumonia at chest CT." Radiology, Vol. 296, No. 2, 2020, pp. 46-54.
Google Scholar Crossref - Chen, Nanshan, et al. "Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study." The Lancet, Vol. 395, No. 10223, 2020, pp. 507-513.
Google Scholar Crossref - Wang, Dawei, et al. "Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China." Jama, Vol. 323, No. 11, 2020, pp. 1061-69.
Google Scholar Crossref - Alhasan, Mustafa, and Mohamed Hasaneen. "The Role and Challenges of Clinical Imaging During COVID-19 Outbreak." Journal of Diagnostic Medical Sonography, Vol. 38, No. 1, 2022, pp. 72-84.
Google Scholar Crossref - Li, Ruiyun, et al. "Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV-2)." Science, Vol. 368, No. 6490, 2020, pp. 489-93.
Google Scholar Crossref - Rothe, Camilla, et al. "Transmission of 2019-nCoV infection from an asymptomatic contact in Germany." New England journal of medicine, Vol. 382, No. 10, 2020, pp. 970-71.
Google Scholar Crossref - Gulati, Aishwarya, and Rashmi Balasubramanya. "Lung Imaging." StatPearls Publishing, 2022.
Google Scholar - Wong, Ho Yuen Frank, et al. "Frequency and distribution of chest radiographic findings in patients positive for COVID-19." Radiology, Vol. 296, No. 2, 2020, pp. E72-E78.
Google Scholar Crossref - Gandhi, Darshan, et al. "Current role of imaging in COVID-19 infection with recent recommendations of point of care ultrasound in the contagion: a narrative review." Annals of Translational Medicine, Vol. 8, No. 17, 2020.
Google Scholar Crossref - Inui, Shohei, et al. "Chest CT findings in cases from the cruise ship diamond princess with coronavirus disease (COVID-19)." Radiology: Cardiothoracic Imaging, Vol. 2, No. 2, 2020, p. e200110.
Google Scholar Crossref - Caruso, Damiano, et al. "Chest CT features of COVID-19 in Rome, Italy." Radiology, Vol. 296, No. 2, 2020, pp. E79-E85.
Google Scholar Crossref - Yu, Zekuan, et al. "Rapid identification of COVID-19 severity in CT scans through classification of deep features." Biomedical engineering online, Vol. 19, No. 1, 2020, pp. 1-13.
Google Scholar Crossref - Guillo, Enora, et al. "COVID-19 pneumonia: diagnostic and prognostic role of CT based on a retrospective analysis of 214 consecutive patients from Paris, France." European Journal of Radiology, Vol. 131, 2020.
Google Scholar Crossref - Naguib, Michael, et al. "The use of radiological imaging alongside reverse transcriptase PCR in diagnosing novel coronavirus disease 2019: a narrative review." Future Microbiology, Vol. 15, No. 10, 2020, pp. 897-903.
Google Scholar Crossref - Gietema, Hester A., et al. "CT in relation to RT-PCR in diagnosing COVID-19 in The Netherlands: A prospective study." PloS one, Vol. 15, No. 7, 2020, p. e0235844.
Google Scholar Crossref - Feng, Hao, et al. "A case report of COVID-19 with false negative RT-PCR test: necessity of chest CT." Japanese journal of radiology, Vol. 38, No. 5, 2020, pp. 409-10.
Google Scholar Crossref - Fechner, Carsten, et al. "COVID-19 and the role of imaging: early experiences in Central Switzerland." Swiss Medical Weekly, Vol. 150, 2020.
Google Scholar Crossref - Lomoro, Pascal, et al. "COVID-19 pneumonia manifestations at the admission on chest ultrasound, radiographs, and CT: single-center study and comprehensive radiologic literature review." European journal of radiology open, Vol. 7, 2020.
Google Scholar Crossref - Peng, Qian Y., Xiao T. Wang, and Li N. Zhang. "Chinese Critical Care Ultrasound Study Group (CCUSG). Findings of lung ultrasonography of novel coronavirus pneumonia during the 2019-2020 epidemic." Intensive Care Med, Vol. 46, No. 5, 2020, pp. 849-50.
Google Scholar - Alzahrani, Ali, Md A. Bhuiyan, and Fahima Akhter. "Detecting COVID-19 Pneumonia over Fuzzy Image Enhancement on Computed Tomography Images." Computational and mathematical methods in medicine, 2022, pp. 1-12.
Google Scholar Crossref - Matos, João, et al. "Evaluation of novel coronavirus disease (COVID-19) using quantitative lung CT and clinical data: prediction of short-term outcome." European radiology experimental, Vol. 4, 2020, pp. 1-10.
Google Scholar Crossref