Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 10
Psychosocial Aspects of COVID-19 in Older Adults, Their Challenges and Responses: A Cross-Sectional Study, Jeddah, Kingdom of Saudi Arabia, 2020-2021
Samah M Alsafadi1* and Amal H Al Ghamdi22Consultant Preventive Medicine and Public Health, Ministry of Health, Public Health Administration, Saudi Board Preventive Medicine Joint Program, Jeddah, Kingdom of Saudi Arabia
Samah M Alsafadi, Resident at Saudi Board Preventive Medicine Joint Program, Ministry of Health, Public Health Administration, Jeddah, Kingdom of Saudi Arabia, Email: samahalsafadi123@gmail.com
Received: 28-Sep-2021 Accepted Date: Oct 22, 2021 ; Published: 29-Oct-2021, DOI: O
Abstract
Background: The inconstant effects and consequences of many pandemics, as well as the variety of public health emergencies of international concerns that occurred throughout history, affect all aspects of the population, especially the most vulnerable groups like the elderly. In this study, we highlighted the psychological effects in this special population and health care impacts during the COVID-19 pandemic and its preventive measures. Subjects and Methods: Through a cross-sectional study design, an interview-based questionnaire of a translated and culturally modified version of the Questionnaire for Assessing the Impact of COVID-19 Pandemic and Accompanying Mitigation Efforts on Older Adults (QAICPOA) was used on a sample of 394 participants who were recruited using a multistage stratified random sampling technique of older adults registered at Primary Health Care Centers (PHCC) in Jeddah, Kingdom of Saudi Arabia, who attended between April and July 2021. Since Clinical diseases of the elderly population vary by their age, we classified them based on their age to three main groups, the youngest-old, the middle-aged old, and the oldest old, to investigate the effect of the COVID-19 pandemic on their psychosocial health at various age groups to better understand their challenges and needs. Results: The mean age of participants was 74 years (SD ± 9.27), and 54% were males. Approximately two-thirds of the participants were concerned about the COVID-19 pandemic. Hence, 83% avoided public places and crowds, 66% ceased from visiting family and friends; ultimately 25% isolated themselves from family members of the same household. The majority, 75.4% (n=297) had extreme difficulties or were unable to obtain regular medical care and medication, in addition to facing other challenges related to communication, and life necessities. In response, some were resilient and even volunteered to help. Conclusion and recommendations: The majority of the study participants experienced social and psychological difficulties related to the COVID-19 pandemic; therefore, new comprehensive and sustainable preventative measures and health services are needed in the future to ensure healthy aging of this vulnerable group during emergencies.
Keywords
COVID-19, Older adults, Psychosocial, Challenges, Responses
Introduction
Coronavirus Disease 2019 (COVID-19) was declared a pandemic and a Public Health Emergency of International Concern on March 11, 2020, by the World Health Organization (WHO) and is still spreading actively even 2 years after, affecting more than 200 million cases worldwide [1].
Because of the fast-spreading and unclear natural history of the novel Severe Acute Respiratory Coronavirus-2 (SARSCoV- 2) disease, governments across the globe were forced to adopt abrupt and drastic population isolation measures such as social distancing, quarantine, business closures, social and public gatherings restrictions, and travel banding to reduce viral transmission and disease spread, especially among the most vulnerable population like the elderly and those with known chronic diseases, due to the proven higher severity and mortality of the disease when affecting them [2,3].
The socioeconomic and health care impacts of this unpredictable pandemic and its preventive measures not only threaten the older adult’s physical health but also affect their mental health. The distress stems from the constant fear of contracting the virus, losing loved ones to the illness which could be their only caretakers, and being socially isolated or quarantined with a shortage of basic needs, and medical care [4,5].
Early on at the start of the pandemic, most studies on the elderly population focused on the clinical and physical aspects of the COVID-19 disease on this vulnerable group. Further on into the pandemic the scientific community has come to realize the need for more studies that explore the other aspects of COVID-19 disease like its mental and psychological effects in this special population. These studies mostly looked at the geriatric population as one group, and mostly quantified the frequency of psychological disorders and functional or cognitive deterioration secondary to the COVID-19 disease pandemic health care shortages at long-term care facilities and old care residences. Little has been published on the psychosocial effects of the pandemic on the ambulatory geriatric population in the community. Because Clinical diseases of the elderly population vary by their age, so we believe are their psychosocial challenges and needs. Hence, classifying them into different groups based on their ages might be considered a new approach to better understand these challenges and needs. In this study we classified the older population based on their age into three main groups, the youngest-old, the middle-aged old, and the oldest old, to investigate the effect of the COVID-19 pandemic on their psychosocial health at various ages groups.
Materials and Methods
Study Design, Setting, and Participants
This is a cross-sectional study design, interview-based questionnaire of older adults 60 years and older who attended the ministry of health Primary Health Care Centers (PHCC) in Jeddah, Kingdom of Saudi Arabia between April and July 2021. All participants who were able to understand and answer the questionnaire were included. Those who suffered from advanced dementia or other mental disorders the affected their cognitive abilities were excluded. Jeddah is a city of approximately four million people, located on the coast of the Red Sea in western Saudi Arabia. In Jeddah, health care services are provided through two main health clusters, namely the north and the south clusters based on their geographical distribution. PHCCs are distributed in each cluster’s proportionality and geographically based on the population densities. Patients were recruited from governmental PHCCS from both clusters using a multistage stratified random sampling technique. First, PHCCs were selected proportionally to represent all districts from both clusters. Secondly, participants were recruited from these primary care centres using simple random sampling. Verbal consent was obtained from the participants themselves or their caretakers before conducting the interview-based questionnaire. Ethical approval was obtained from both the ethical committee of The Joint Program for the Saudi board for Preventive Medicine and the Directorate of Health Affairs research ethics committee in Jeddah. In addition Institutional ethical approval was obtained from each PHCC ethics department.
Data Collection Tools
A checklist developed by the principal researcher was used to reflect the demographic, health, and social factors of the participants including information about their: age, sex, marital status, education, occupation, monthly income, housing, past medical history, medications, and smoking status.
A translated and culturally modified version of the Questionnaire for Assessing the Impact of COVID-19 Pandemic and Accompanying Mitigation Efforts on Older Adults (QAICPOA) validated by Dr. Peggy Cawthan, University of California, San-Francisco, USA was used to assess the challenges and responses of the study population to COVID-19 preventative measures. The original form of the questionnaire was shared generously by the author with all the research community through an open-access website and permission for use was obtained before the study commences. The translation of the above questionnaire was performed by two bilingual professional translators, then back-translated into English and compared with its original version. The questionnaire content validity was then revised by two other consultants with consistency and similarity of >80% between the two English versions. The questionnaire included questions about the participant’s subjective feelings, and concerns with COVID-19 pandemic and its effect on their social communications and ability to obtain food, medical help, and medications. In addition, it collected information on their response to the various preventative measures related to the pandemic and social distancing and any other actions like volunteering or social assistance.
Data Analysis
Data were coded and analyzed using the IBM Statistical Package for Social Sciences (SPSS) for Windows, version 28 (IBM Corp., Armonk, N.Y., USA). Mean, standard deviation, and range were used to describe quantitative variables, while frequencies and proportions were used for categorical variables; bi and multivariate analyses were used as appropriate for further analyses.
The participants’ age was categorized into three main groups, the young mostly active older adults between ages 60 and 69 yrs., the middle age mixed responses older adults between ages 70 and 79 yrs., and the oldest mostly dependent older adults between ages 80 and 100 yrs. Logistic regression was used to predict the effect of the various demographic, health and social factors on participant increased concern with COVID-19 disease.
The sample size was calculated based on the parameter choices, for the desired power of 0.80 and a Type I error rate of 0.05, with a 95% confidence interval.
Results
In total 394 participants were included in the study, of whom 53.6% (n=211) were males. The mean age was 74 yrs (SD ± 9.27). Participants’ demographic, social, and health characteristics are presented in Table 1.
| Age 60-69 | Age 70-79 | Age 80-89 | Total | p-value | |
|---|---|---|---|---|---|
| 145 (36.8%) | 134 (34%) | 115 (29.2%) | 394 (%) | ||
| Sex | |||||
| Male | 75 (51.7%) | 78 (58.2%) | 58 (50.4%) | 211 (53.6%) | 0.4 |
| female | 70 (48.3%) | 56 (41.8%) | 57 (49.6%) | 183 (46.6%) | |
| Nationality | |||||
| Saudi | 119 (82%) | 109(81.3%) | 100 (87%) | 328 (83.2%) | 0.3 |
| Non Saudi | 26 (17.9%) | 25 (18.7%) | 15 (13 %) | 66 (16.8%) | |
| Marital status | |||||
| Never married | 9 (6.2%) | 1 (0.7%) | 0 (0%) | 10 (2.5%) | <0.001* |
| Married | 123 (84.8%) | 85 (63.4%) | 1 (0.9%) | 209 (53%) | |
| Divorced | 13 (9%) | 3 (2.2%) | 0 (0%) | 16 (4.1%) | |
| widowed | 0 (0%) | 45 (33.3%) | 114 (99.1%) | 159 (40.4%) | |
| Education | |||||
| Postgraduate | 32 (22.1%) | 0 (0%) | 0 (0%) | 32 (8.1%) | <0.001* |
| Graduate university or college | 94 (64.8%) | 49 (36.6%) | 2 (1.7%) | 145 (36.8%) | |
| High school or less | 19 (13.1%) | 85 (63.4%) | 113 (98.3%) | 217 (55.1%) | |
| Occupation | |||||
| Retired | 61 (42.1%) | 134 (100%) | 115 (100%) | 310 (78.7%) | <0.001* |
| Employed | 65 (44.8%) | - | - | 65 (16.5%) | |
| Self-employed | 19 (13.1%) | 19 (4.8%) | |||
| Monthly income | |||||
| <10,000 SRa | 86 (59.3%) | 132 (98.5%) | 115 (100%) | 333 (84.5%) | <0.001* |
| 10,000-19999 SR | 51 (35.2%) | 2 (1.5%) | 53 (13.5%) | ||
| ≥ 20,000 SR | 8 (5.5%) | 0 (0%) | 8 (2%) | ||
| District of Living | |||||
| North cluster | 79 (54.5%) | 44 (32.8%) | 56 (48.7%) | 179 (45.5%) | 0.06 |
| South cluster | 66 (45.5%) | 90 (67.2%) | 59(51.3%) | 215 (54.5%) | |
| Housing Ownership | |||||
| Own house | 63 (43.4%) | 1 (0.7%) | 0 (0%) | 64 (16.2%) | <0.001* |
| Rent house | 57 (39.3%) | 3 (2.2%) | 0 (0%) | 60 (15.2%) | |
| Live with relatives | 24 (16.6%) | 126 (94%) | 111 (96.5%) | 261 (66.2%) | |
| Government housing | 1 (0.7%) | 4 (3%) | 4 (3.5%) | 9 (2.3%) | |
| Number of Household Members | |||||
| Two or less | 41(28.3%) | 16 (11.9%) | 15 (13%) | 41 (18.3%) | <0.001* |
| Three to five | 60 (41.4%) | 116 (86.6%) | 100 (87%) | 276 (70.1%) | |
| Six or more | 44 (30.3%) | 2 (1.5%) | 0 | 46 (11.7%) | |
| House Hold Member Support | |||||
| Support provided | 112 (77.2%) | 122 (91%) | 115 (100%) | 349 (88.6%) | <0.001* |
| No support provided | 33 (22.7%) | 12 (9%) | 0 | 45 (11.4 %) | |
| Past Medical History | |||||
| No chronic disease | 4 (2.8%) | 4 (3%) | 0 (0%) | 8 (2%) | 0.042* |
| One chronic disease | 52 (35.9%) | 60 (44.8%) | 35 (30.4%) | 147 (37.3%) | |
| Two chronic diseases | 77 (53.1%) | 60 (44.8%) | 62 (53.9%) | 199 (50.5%) | |
| ≥ 3 chronic diseases | 12 (8.3%) | 10 (7.5%) | 18 (15.7%) | 40 (10.2%) | |
| Medications Numbers | |||||
| ≤ 2 medications | 20 (13.8%) | 29 (21.6%) | 14 (12.2%) | 63 (16 %) | 0.08 |
| ≥ 3 medication | 125 (86.2%) | 105 (78.4%) | 101 (87.8%) | 331 (84%) | |
| Smoking | |||||
| Non-smoker | 40 (17.6%) | 134 (100%) | 114 (99.1%) | 288 (73.1) | <0.001* |
| Quit | 59 (40.7%) | 1 (0.9%) | 60 (15.2%) | ||
| Current smoker | 46 (31.7%) | 0 (0%) | 46 (11.7%) | ||
| *: Statistical difference p<0.005, a: SR=Saudi Riyals, Saudi main currency, 1US$ =3.75 SR | |||||
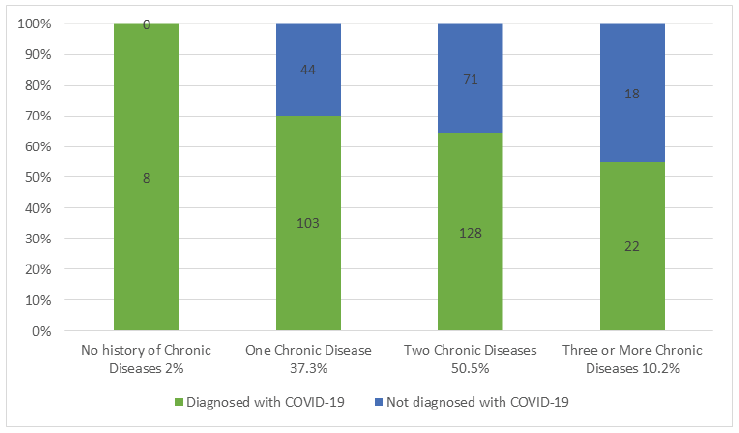
Approximately two-thirds of the participants 74% (n=291) were very concerned about the COVID-19 pandemic, stepwise multivariate logistic regression was performed trying to predict the factors associated with their increased concern. After adjusting for all the significant factors in the multivariate logistic model, past medical history of 2 or more chronic diseases (OR 4.59, p<0.001, 95% CI (2.59-8.12) and diagnosis with COVID-19 disease (OR 2.98, p<0.001, 95% CI 1.55-6.09) was significantly associated with increased concern with the pandemic. There was no significant difference observed between the number of chronic diseases and the diagnosis with COVID-19 disease. (p=0.054, Chi-X=7.6). Figure 1 summarizes the number of participants diagnosed with COVID- 19 diseases divided according to their past medical history.
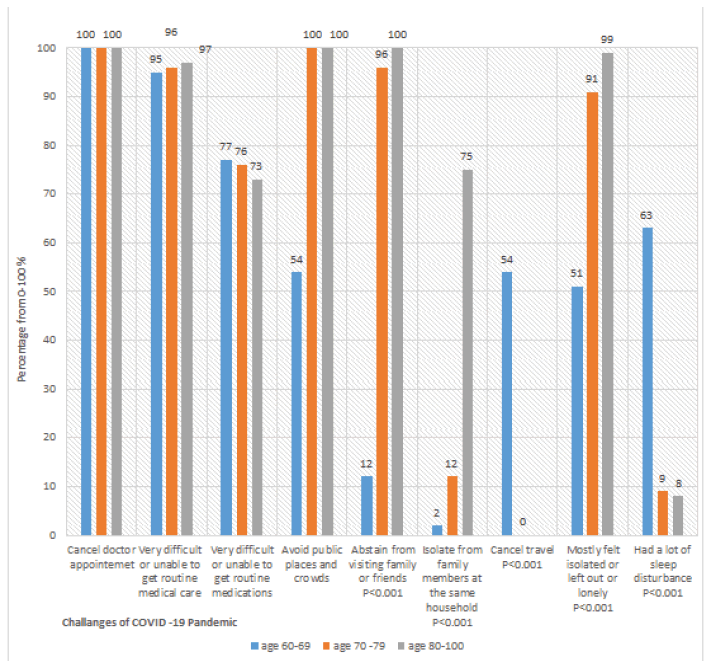
During the pandemic, the majority of the participants had their routine medical appointment canceled with 9% (n=36) having health checkups through telehealth. In addition, 95.4% (n=376) found it very difficult or were unable to get routine medical care, while 75.4% (n=297) had extreme difficulties or were unable to get routine medications.
Socially, 83% (n=327) avoided public places and crowds, 66% (n=261) abstained from visiting family or friends, and ultimately 25.4% (n=100) isolated themselves from members of the same household. As a result, 78.7% (n=310) felt mostly isolated with lack of companionship, and 26.4% (n=104), had a lot of sleep disturbance. Figure 2 summarizes the challenges faced by the study participants across different age groups during the COVID-19 pandemic.
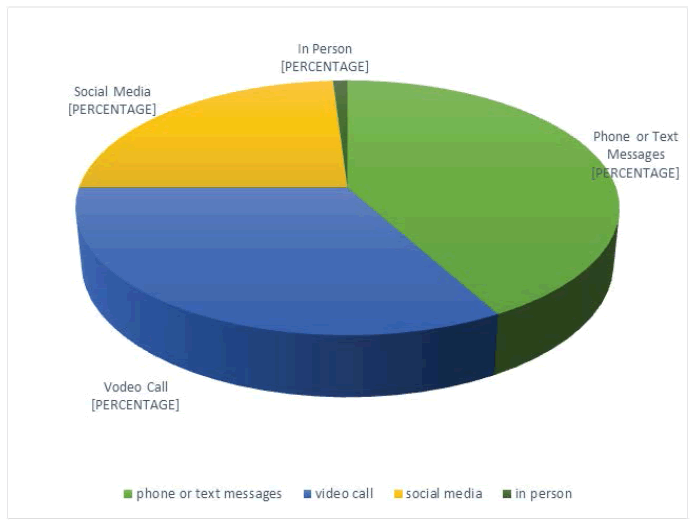
About two-thirds had decreased frequency of communication with their family or friends than before the pandemic, and 20% (n=78) had travel cancellation which was intended mostly for family visitation. Figure 3 illustrates the means of social communication used by the participants during the pandemic.
All study participants complied with wearing masks and using hand sanitizers at public places, despite that 66.2% (n=261) were diagnosed with COVID-19 and recovered of whom 83.2% (n=328) had a family member or a friend diagnosed with COVID-19.
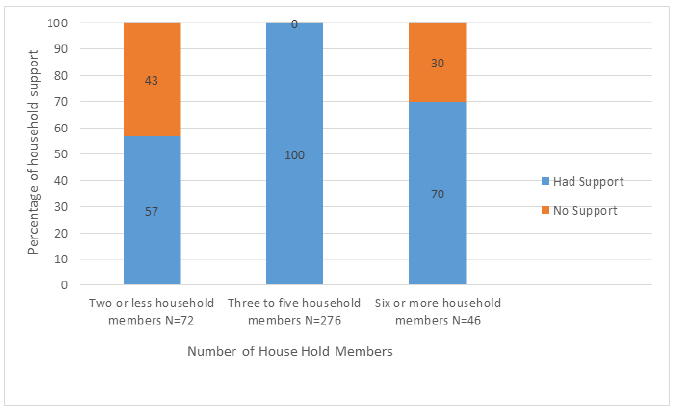
New actions were taken by some of the participants to help out their community including donating money 65.5% (n=258), food 46.4% (n=183), or blood 1.5% (n=6), and providing childcare 22.1% (n=87). In return, the majority of the study participants got support from their families or friends during the pandemic 88.6% (n=349), mostly from those they live with 76% (n=264), or only through social media 24% (n=85). The relationship between the number of household members and the percentage of social support was found to be statistically significant (p<0.001, Chi-X=9.69). Figure 4 shows the relation between the number of household members and the percentage of social support.
Discussion
Traditionally, the majority of studies on older adults tend to sum all older adults in one group constituting of those who are aged 65 or older, but the exponential global aging of the world population and the many gaps in the literature concerning the actual understanding of the aging process and its impacts at various levels on the aging population necessitated the adoption of a non-traditional approach to data collection and analysis to better enhance our understanding of the effects, the needs and the opportunities related to the growing older adults at different stages of their aging process. Hence, we have divided the study population into three different groups, the young older adults, the middle-aged older adults, and the oldest adults. Few other studies have also adopted a similar way of classifying its older population as our study with differences in the cutoff age of each group based on the demography of their older population [6]. In the aging, aged, and super-aged societies in which the people aged 65 or older constitute >7%, >14%, and >20% of the total population consecutively, they tend to classify older adults between 65 and 74 as youngest -old, those between 75 and 84 as middle- old and finally, those over 85 years as oldest-old. In contrast in a young aging society with an elderly population <7% like Saudi Arabia, with a percentage of older adults aged 65 or older around 2.4%, and a life expectancy of 75.7 years (General Authority for Statistics Saudi Arabia, 2019; UN World Population Prospects, 2019 Revision), older adults usually classified starting at age 60 yrs. and older [7].
Each age category, represented in this study with almost equal percentages helped reflect the pandemic effects across the entire geriatric age span. We observed a significant difference in most of the social and medical determinants between the three age groups, which in our opinion may explain the differences in their abilities to respond and cope with emerging and sudden changes in their environment. Lee, S. B, has also observed significant differences in the clinical characteristics of older adults attending the emergency department based on their old age group classification [8].
One of the challenges that faced the older population was their inability to obtain routine medical care, which is quite expected given the overwhelming of the health care services with the COVID-19 cases, which may affect their overall health and associated chronic diseases [9,10]. While the majority of health care systems were focused on how to stop the spread of the COVID-19 disease and treat those who are suffering its health consequences, secondary complications of existing diseases may arise if timely follow up were delayed [11]. Additionally, the social isolation and the lockdown with its associated stress may further affect their mental health [12].
Saudi Arabia, customs and traditions, place the elderly in a position of respect, appreciation, and care. Traditionally, Saudi families have taken care of their elder parents or relatives at their homes till they die, and it is considered a social stigma to place your elders in a special care home or government social services housing. Most of our study participants, especially the oldest adults have support from their younger household members but that might not be the case in other societies with less rigid family ties [13]. Even though the majority of the youngest older adults had support from family or friends through social media, but that might change in the future as the younger individuals’ assistance might be unavailable due to changing structure of the communications at a faster pace depending on technology communication with less emphasis on person gathering and companionship [14]. In addition, due to the possibilities of unpredicted pandemics and natural disasters that may occur in the future, government and non-government organizations may need to start planning for sustainable adequate measures and geriatrics health care facilities [15].
Residence-based services for the elderly, like running errands, acquiring and delivering food, medications, and other everyday life necessities should be thought off, planned, and executed through a solid system that will not be interrupted during emergencies [16,17].
Additionally, older people need to be familiarized with the new online technologies and services to obtain news, help, and social support no matter where they are [18]. Physical rather than social distancing should be practiced at times of pandemics. Knowledge of the various means of communication used by the elderly helps plan future programs using communication technology to provide health and mental counseling as well as updated news, information, and behavioral therapy, to maintain the mental and spiritual health of this greatly appreciated group [19,20]. In our study, the most used mean of communication among the participant was phone and text messages and one-third of the participants were already using video calls and social media which open up the floor for a new era of digitalized health of the elderly that we can build on [21-23].
“Resilience matters”, older people’s contributions to their societies are still greatly appreciated. Some through physical contributions like volunteering, donating food, money, and providing childcare, and others through sharing their vast wisdom, experience, knowledge, support, and encouragements with the younger generation [24].
The continuous scare from acquiring the disease and its continuous effect on their underlying comorbidities was found in our study to be the two main factors behind the participants’ increase concern with the pandemic and stress.
Limitations
The subjective opinion of the study participants’ challenges and responses were obtained and no objective measures are available to measure them.
The participant interviewed were mainly ambulatory subjects visiting the PHCCs from the community, results may vary in the population residing in acute or long-term care facilities. Finally, this is a cross-sectional study that is useful for establishing preliminary evidence but future long-term follow-up cohort studies are needed to further analyze the study results.
Conclusion
This study highlights the differences in challenges and responses between the various older age groups at the time of stress and inspires a new approach for designing a comprehensive age-friendly approach balancing their physical and psychosocial needs in planning their health and social services based on their various stages of aging.
For the older adults, understanding that the older population group abilities and needs are different across the entire geriatric population age span is the key step to a new approach for planning and building rigid but friendly health and social services that take into consideration the physical and cognitive abilities of the older population in addition to their medical needs.
Recommendations
Emphasis on the functional and cognitive status of older adults across different age groups should be taken into consideration when planning various geriatric health services to offer a more comprehensive care model for the older adults rather than the traditional disease-based model. Guidelines for preventative measures should take into consideration the variation in the physical ability and social connectivity across the aging population, so appropriate measures would be recommended that suit every one ability without compromising their safety. Older adults should be offered and trained in new tools like virtual primary care offices visits and automated medication refill systems that will enable access to greatly needed routine medical care under any emergencies.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Acknowledgment
We would like to acknowledge our elderly parents and relatives for giving us their insights and supports during the preparation of this research.
References
- World Health Organization, Coronavirus (COVID-19 Dashboard).https://covid19.who.int/
- Bedford, Juliet, et al. "COVID-19: Towards controlling of a pandemic." The Lancet, Vol. 395, No. 10229, 2020, pp. 1015-18.
- Wang, Dawei, et al. "Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China." JAMA, Vol. 323, No. 11, 2020, pp. 1061-69.
- Armitage, Richard, and Laura B. Nellums. "COVID-19 and the consequences of isolating the elderly." The Lancet Public Health, Vol. 5, No. 5, 2020, p. e256.
- Berger, Zackary D., et al. "COVID-19: Control measures must be equitable and inclusive." BMJ, 2020.
- Alterovitz, Sheyna Sears-Roberts, and Gerald A. Mendelsohn. "Partner preferences across the life span: Online dating by older adults." Psychology of Popular Media Culture, Vol. 1, 2011, pp. 89-95.
- General Authority for Statistics Kingdom of Saudi Arabia. https://www.stats.gov.sa/en/1006
- Lee, Sang Bum, et al. "Differences in youngest-old, middle-old, and oldest-old patients who visit the emergency department." Clinical and Experimental Emergency Medicine, Vol. 5, No. 4, 2018, pp. 249-55.
- Bobes-Bascarán, Teresa, et al. "Early psychological correlates associated with COVID-19 in a Spanish older adult sample." The American Journal of Geriatric Psychiatry, Vol. 28, No. 12, 2020, pp. 1287-98.
- Dhama, Kuldeep, et al. "Geriatric population during COVID-19 pandemic: Problems, considerations, exigencies and beyond head title: Geriatrics during COVID-19 pandemic." Frontiers in Public Health, Vol. 8, 2020, p. 562.
- Shahid, Zainab, et al. "COVID‐19 and older adults: What we know." Journal of the American Geriatrics Society, Vol. 68, No. 5, 2020, pp. 926-29.
- Banerjee, Debanjan. "The impact of COVID‐19 pandemic on elderly mental health." International Journal of Geriatric Psychiatry, Vol. 35, No. 12, 2020, pp. 1466-67.
- Lloyd-Sherlock, Peter, et al. "Bearing the brunt of COVID-19: Older people in low and middle income countries." BMJ, 2020.
- Fraser, Sarah, et al. "Ageism and COVID-19: What does our society’s response say about us?" Age and Ageing, Vol. 49, No. 5, 2020, pp. 692-95.
- Fischer, Florian, et al. "COVID-19 and the elderly: Who cares?" Frontiers in Public Health, Vol. 8, 2020, p. 151.
- Lloyd-Sherlock, Peter G., et al. "WHO must prioritise the needs of older people in its response to the COVID-19 pandemic." BMJ, 2020.
- Steinman, Michael A., Laura Perry, and Carla M. Perissinotto. "Meeting the care needs of older adults isolated at home during the COVID-19 pandemic." JAMA Internal Medicine, Vol. 180, No. 6, 2020, pp. 819-20.
- Finn, C. "How tech is helping elderly fight coronavirus lockdown loneliness." Al Jazeera, 2020.
- Kall, Anton, et al. "Internet-based cognitive behavior therapy for loneliness: A pilot randomized controlled trial." Behavior Therapy, Vol. 51, No. 1, 2020, pp. 54-68.
- Yang, Yuan, et al. "Mental health services for older adults in China during the COVID-19 outbreak." The Lancet Psychiatry, Vol. 7, No. 4, 2020, p. e19.
- Van den Berg, Neeltje, et al. "Telemedicine and telecare for older patients-A systematic review." Maturitas, Vol. 73, No. 2, 2012, pp. 94-114.
- Morrow-Howell, Nancy, Natalie Galucia, and Emma Swinford. "Recovering from the COVID-19 pandemic: A focus on older adults." Journal of Aging & Social Policy, Vol. 32, No. 4-5, 2020, pp. 526-35.
- Kuwahara, Keisuke, Ai Kuroda, and Yoshiharu Fukuda. "COVID-19: Active measures to support community-dwelling older adults." Travel Medicine and Infectious Disease, Vol. 36, 2020, p. 101638.
- Chen, Liang-Kung. "Older adults and COVID-19 pandemic: Resilience matters." Archives of Gerontology and Geriatrics, Vol. 89, 2020, p. 104124.