Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 1
Primary Epidural Lymphoblastic Lymphoma Presented with Unsteady Gait: A Case Report
Waleed Mohammed Awwad and Fahad Abdullah Al Shayhan*Fahad Abdullah Al Shayhan, Orthopaedic Surgery Department, King Saud University, Riyadh, Saudi Arabia, Email: Fahadshayhan@gmail.com
Received: 02-Dec-2020 Accepted Date: Jan 22, 2021 ; Published: 29-Jan-2021, DOI: O
Abstract
Background: Epidural involvement in non-Hodgkin’s lymphoma is not a classical presentation. Limited cases were reported with B-lineage Lymphoblastic Lymphoma (B-LBL). Patients develop an acute onset of neurological symptoms preceded by vague back pain. Case presentation: A 6 years old male presented with unsteady gait and bilateral foot numbness for 3 days. Acute onset of paraplegia was noticed after 2 days from admission. MRI showed large anterior paravertebral and posterior mediastinal soft tissue mass at thoracic spine causing severe spinal cord compression. The patient underwent decompressive laminectomy and received chemotherapy as per the protocol of AALL0232. Two months follow up patient exhibited partial neurological recovery. Conclusion: Vague back pain or gait disturbance, hence posterior spinal column functional disturbance, full neurological examination, and medical imaging must be carried on without delay. Once a space occupation lesion with a progressive neurological deficit is identified, urgent surgical management must be undertaken to preserve remaining function and aid for the best functional recovery.
Keywords
Lymphoblastic lymphoma, Non-Hodgkin lymphoma, Incomplete spinal cord injury, Primary spinal
Introduction
Lymphoblastic Lymphoma (LBL) is a subtype of Non-Hodgkin’s lymphoma (NHL) and represents 2% among the other types [1]. It originates from either the precursor of B cell from bone marrow or thymic T cell [1]. B-Lineage Lymphoblastic Lymphoma (B-LBL) is a rare entity and constitutes 10% of all Lymphoblastic Lymphoma (LBL) [1,2]. Mostly it affects children, but also it can occur in adulthood [1]. Primary presentation of epidural Non-Hodgkin’s lymphoma (NHL) is rare 9% of all epidural masses and specifically primary presentation with epidural Lymphoblastic Lymphoma (LBL) is very rare [3,4]. Epidural involvement is thought to be from the distant source through the lymphatic system or direct invasion from vertebral bodies [5]. In this article, we describe a case of 6 years old child who presented with an unsteady gait due to epidural Lymphoblastic lymphoma.
Case Representation
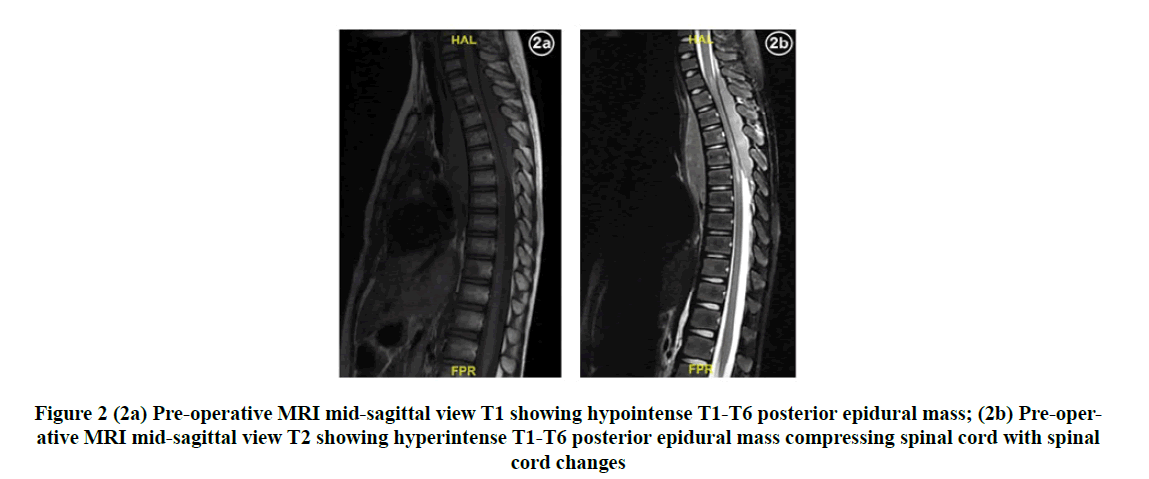
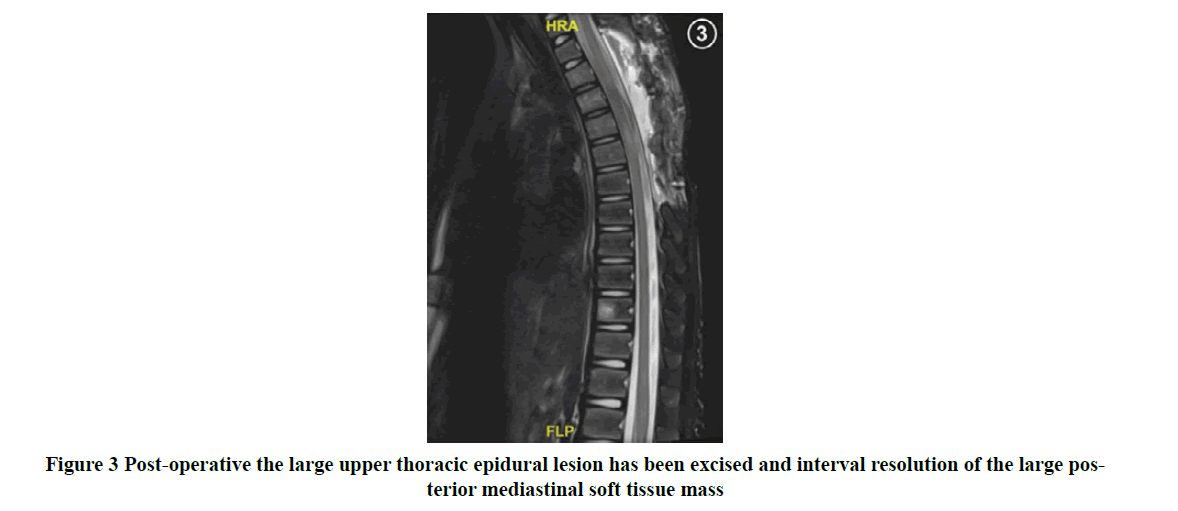
A 6 years old male not known to have any illness, presented to the emergency department with a history of unsteady gait and bilateral foot numbness for 3 days. The patient’s mother reported a history of minor direct back trauma and denied a history of back pain, saddle paresthesia, urinary or bowel incontinence, fever, night sweat, or history of fall. Patient admitted under pediatric service for investigations. The neurological examination upon presentation for upper and lower extremities revealed intact sensation, power 5/5, deep tendon reflexes including biceps, triceps, brachioradialis, knee, and ankle reflexes +2 with no signs of myelopathy. Plain Computed Tomography (CT) of the whole spine showed upper thoracic posterior mediastinal soft tissue mass with posterior epidural component causing severe spinal canal stenosis (Figure 1). Two days later, the mother reported 2 episodes of urinary incontinence with no history of back pain. Upon examination, the patient was found to have flaccid paraplegia. A spine surgery service was consulted. Urgent Magnetic Resonance Imaging (MRI) of the brain and whole spine revealed large anterior paravertebral and posterior mediastinal soft tissue mass at the upper thoracic spine, causing severe spinal canal stenosis and spinal cord compression (Figure 2). The patient underwent emergency T1-T6 decompressive laminectomy and removal of mass (Figure 3). Postoperatively patient received a high dose of dexamethasone.
Histopathology
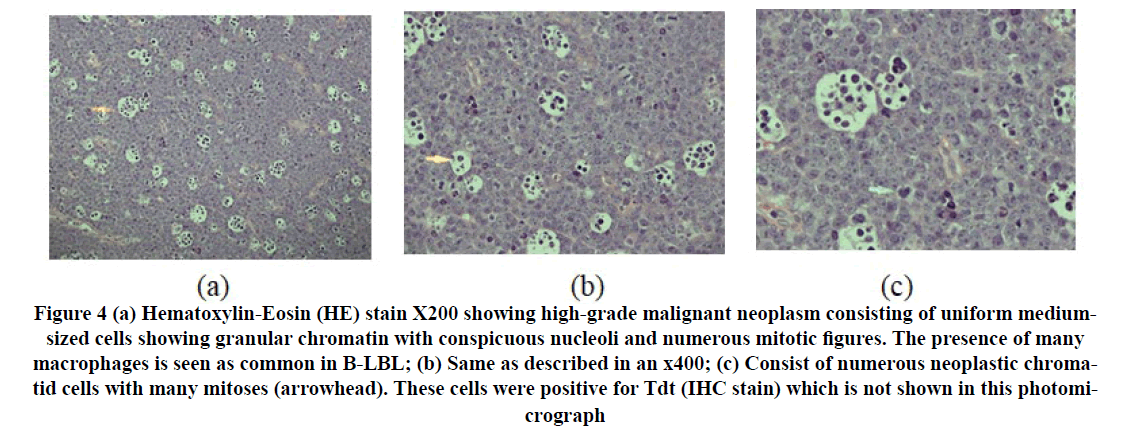
The final histopathology report showed Histological features consistent with lymphoblastic lymphoma of B cell type. This is based on the positive TdT, negative CD20, positive CD10, and negative BCL-6 and BCL-2 in addition to positive PAX5 and CD79A. CMYC was also strongly positive (Figure 4).
Figure 4. (a) Hematoxylin-Eosin (HE) stain X200 showing high-grade malignant neoplasm consisting of uniform medium - sized cells showing granular chromatin with conspicuous nucleoli and numerous mitotic figures. The presence of many macrophages is seen as common in B-LBL; (b) Same as described in an x400; (c) Consist of numerous neoplastic chromatid cells with many mitoses (arrowhead). These cells were positive for Tdt (IHC stain) which is not shown in this photomicrograph
Staging Investigations
Pediatric oncology service was consulted where they started staging investigations. Chest X-ray was unremarkable. Peripheral blood smear showed neutrophilia with toxic granulation, few large granular lymphocytes are noted as well as reactive/atypical looking lymphocytes. RBCs reflect microcytic blood picture with few ovalocytes. Computed Tomography (CT) chest abdomen and pelvis report no suspicious pulmonary nodules, no axillary lymphadenopathy, no obvious focal hepatic lesion, the solid abdominal organs are unremarkable, no size significant lymphadenopathy in abdomen and pelvis. Bone marrow aspiration revealed normocellular bone marrow with normal megakaryopoiesis and erythropoiesis and left-shifted myelopoiesis. No morphological and immunophenotypical evidence of lymphoma.
Chemotherapy
The patient was started on AALL0232 chemotherapy protocol as following: induction course (intrathecal Cytarabine, Vincristine, Daunorubicin, Prednisone, Pegaspargase, and intrathecal methotrexate) and extended induction course (intrathecal methotrexate, Prednisone, Vincristine, Daunorubicin, and Pegaspargase). The patient will continue in the coming day’s consolidation and maintenance courses [6].
Post-operative Neurological Course
During the post-operative course patient neurologically start to recover gradually, able to control the bowel and bladder. The patient started physical therapy exercises on the bed. MRI post-surgical decompression and after initial induction course is demonstrated in Figure 3. Up-to-date (2 months post-surgery) wound healed and neurological exam showed intact sensation, power bilaterally L2 (3/5), L3 (3/5), L4 (3/5), L5 (3/5), and S1 (4/5). Hyper-reflexia over knee-deep tendon reflex is noted bilaterally with bilateral positive Babinski and clonus tests.
Discussion
The usual presentation of Lymphoblastic Lymphoma (LBL) is acute leukemia or mediastinal mass [1]. Primary presentation of epidural Non-Hodgkin’s lymphoma (NHL) is considered rare and Lymphoblastic Lymphoma (LBL) furthermore is very rare with few cases reported [3,7]. Primary Spinal Epidural Lymphoma (PSEL) presentation is divided into two phases: the first phase where patients are complaining of localized back pain which may last for months. Second phase patients present with progressive neurological symptoms [4]. Commonly patients present with back pain localized over the epidural lesion level [5]. The most affected spinal segment is the thoracic vertebra, lumbar and cervical spine respectively [4]. The thoracic spine is thought to be most vulnerable to Primary Spinal Epidural Lymphoma (PSEL) due to the length of the segment compared to the cervical and lumbar spine or due to the abundance of venous plexus in the thoracic spine [5]. “B” symptoms including weight loss, night sweating, and fever are classically not found among patients who presented with PSEL, only a few patients were reported (5.7%) [5].
Up to the best of our knowledge, two reported cases of primary presentation of epidural B-lineage Lymphoblastic Lymphoma (B-LBL) [3,4]. The case described in this paper is 6 years old child who presented with an unsteady gait with progressive neurological compromise secondary to epidural lymphoblastic lymphoma.
Patients with early stages of Primary Spinal Epidural Lymphoma (PSEL) tend to have no symptoms [7]. Neurological deficit upon presentation associated with advanced disease [8]. Rakul et al. reported that the patient presented with a one-month history of back pain with worsening neurological condition within one week, while Hongyuan et al., reported that the patient presented with a one-week history of back pain with worsening neurological condition started within 4 days [3,4]. In our case patient presented with an unsteady gait with acute development of paraplegia and urinary retention.
Besides clinical history and physical examination, imaging is required to diagnose Primary Spinal Epidural Lymphoma (PSEL) [3]. Plain X-rays will be negative due to sparing of bone and CT scan is helpful in the staging process, but it lacks specificity to identify Primary Spinal Epidural Lymphoma (PSEL) [3,5]. MRI provides indirect suggestive evidence for the diagnosis of Primary Spinal Epidural Lymphoma (PSEL) which is visualized in T1 with hypointense to isointense, were in T2 isointense to hyperintense [9]. Children are less commonly complaining of low back pain, and advanced imaging should be considered to identify the probable pathology [10].
Histologically most common cause of PSEL is intermediate and high-grade lymphoma [11]. B-LBL is considered a high-grade subtype of non-Hodgkin lymphoma [12]. Patient survivorship is not significantly linked to histological classification [5].
Systematic staging is recommended to evaluate for the presence of distant involvement, and it includes CT CAP (chest, abdomen, and pelvis), bone marrow biopsy, bone scan, MRI brain, and whole spine, as well as Cerebrospinal Fluid (CSF) fluid examination [7]. Staging investigations for our patient revealed no pulmonary nodules, solid abdominal organ involvement, or lymphadenopathy in the abdomen and pelvis.
Treatment of B-lineage Lymphoblastic Lymphoma (B-LBL) includes surgery, chemotherapy, and radiation therapy [1]. No designed chemotherapeutic protocol specifically for B-lineage Lymphoblastic Lymphoma (B-LBL), but the most used for patients with B-lineage Lymphoblastic Lymphoma (B-LBL) is Non-Hodgkin Lymphoma (NHL) and Acute Lymphocytic Leukemia (ALL) protocols [1]. In addition to the surgical intervention, Acute Lymphocytic Leukemia (ALL) chemotherapy protocol carries improvement in survival rate when used in patients with lymphoblastic lymphoma [1]. Beside surgical intervention, AALL0232 chemotherapy protocol was carried out for this patient [6]. The patient didn’t receive radiation therapy.
Lymphoblastic leukemia is an aggressive disease, despite that the current treatment strategy the disease-free survival reaches 90% [1]. B-LBL carries a better prognosis when compared to T-LBL and Central Nervous System (CNS) involvement associated with the worst outcome [2]. The timing of surgical intervention is the most important determinant for neurological recovery [9]. Neurological outcome after Primary Spinal Epidural Lymphoma (PSEL) is variable even after a couple of months and it is mostly correlated with the timing of surgical intervention [1,7]. It was previously reported for a patient who presented with Primary Spinal Epidural Lymphoma (PSEL) and paraplegia is rarely discharged home walking independently [13]. In our case patient demonstrated partial recovery of neurological condition despite early surgical intervention within hours from the development of paraplegia.
Conclusion
Vague back pain or gait disturbance, hence posterior spinal column functional disturbance, full neurological examination, and medical imaging must be carried on without delay. Once a space occupation lesion with the progressive neurological deficit is identified, urgent surgical management must be undertaken to preserve the remaining function and aid for the best functional recovery.
References
- Cortelazzo, Sergio, et al. "Lymphoblastic lymphoma." Critical Reviews in Oncology/Hematology, Vol. 113, 2017, pp. 304-17.
- Soslow, Robert A., Rebecca N. Baergen, and Roger A. Warnke. "Bâ?lineage lymphoblastic lymphoma is a clinicopathologic entity distinct from other histologically similar aggressive lymphomas with blastic morphology." Cancer, Vol. 85, No. 12, 1999, pp. 2648-54.
- Liu, Hongyuan, et al. "Primary lumbar spinal epidural b-lymphoblastic lymphoma: A case report." Biomedical Research, Vol. 29, Issue 11, 2018.
- Nambiar, Rakul K., et al. "Primary spinal epidural B-lymphoblastic lymphoma." Baylor University Medical Center Proceedings, Vol. 30, No. 1, 2017.
- Cugati, Goutham, et al. "Primary spinal epidural lymphomas." Journal of Craniovertebral Junction and Spine, Vol. 2, No. 1, 2011, pp. 3-11.
- Larsen, Eric C., et al. "Dexamethasone and high-dose methotrexate improve outcome for children and young adults with high-risk B-acute lymphoblastic leukemia: a report from Children’s Oncology Group Study AALL0232." Journal of Clinical Oncology, Vol. 34, No. 20, 2016, pp. 2380-8.
- Monnard, Virginie, et al. "Primary spinal epidural lymphoma: patients’ profile, outcome, and prognostic factors: a multicenter Rare Cancer Network study." International Journal of Radiation Oncology Biology Physics, Vol. 65, No. 3, 2006, pp. 817-23.
- Daley, Matthew F., et al. "Primary epidural Burkitt lymphoma in a child: case presentation and literature review." Pediatric Hematology and Oncology, Vol. 20, No. 4, 2003, pp. 333-8.
- Zheng, J. S., et al. "Isolated primary non-hodgkin's lymphoma of the thoracic spine: a case report with a review of the literature." Journal of International Medical Research, Vol. 38, No. 4, 2010, pp. 1553-60.
- Rodriguez, D. P., and T. Y. Poussaint. "Imaging of back pain in children." American Journal of Neuroradiology, Vol. 31, No. 5, 2010, pp. 787-802.
- Barnard, Maja, et al. "Primary spinal epidural mantle cell lymphoma: case report." Neurosurgery, Vol. 47, No. 5, 2000, pp. 1239-42.
- Khalid, Imran, et al. "Case 2. Precursor B-cell lymphoblastic lymphoma presenting as spinal cord compression." Journal of Clinical Oncology, Vol. 22, No. 7, 2004, pp. 1331-3.
- Tsukada, Tetsuya, et al. "Primary epidural non-Hodgkin's lymphoma in clinical stage IEA presenting with paraplegia and showing complete recovery after combination therapy." Internal Medicine, Vol. 31, No. 4, 1992, pp. 513-5.