Research - International Journal of Medical Research & Health Sciences ( 2020) Volume 9, Issue 10
Prevalence and Severity of Plaque-Induced Gingivitis among Saudi Adult Population in Jeddah Region
Hani A. Qataberi, Iffat Mirza Ahmed*, Hadeel Alrifaie, Deemah Albrahimi, Hanan Al Somaly, Fajor Almansouri, Maria Wali, Dana Barabea, Abeer Mansoor and Sherooq HarakaIffat Mirza Ahmed, Oral and Maxillofacial Surgery Department, AlFarabi Colleges, Jeddah, Saudi Arabia, Email: iffatahmd.ams@fpc.edu.sa
Received: 09-Sep-2020 Accepted Date: Oct 15, 2020 ; Published: 22-Oct-2020
Abstract
Objective: To evaluate the prevalence and severity of plaque-induced Gingival inflammation (GI) among Saudi adult population in Jeddah region.
Method: One hundred and ninety-seven eligible participants in this cross-sectional study were recruited from routine dental patients attending the Oral Diagnosis Clinic at AlFarabi College in Jeddah, Saudi Arabia from Nov 2019 to May 2020. A clinical examination was performed by 2 dentists to measure the gingival and plaque indices of Loe and Silness for each participant.
Results: The prevalence of gingivitis was 100% among adult subjects aged between 20-50 years old. Moreover, both the male and female groups with generalized Gingival inflammation (GI) had significantly higher mean scores of plaque index. In addition, females with generalized GI showed a significantly higher plaque index % compared to males (p<0.05). Bleeding on probing (BOP) of generalized GI was higher in females than males. In fact a significant and positive correlation was observed between plaque index % and BOP % in both male and female localized GI groups. This shows that the plaque index and BOP are dependent on each other. However, females were more affected with localized gingivitis than males (p=0.0001).
Conclusion: The results of this study show that plaque accumulation is strongly associated with high prevalence of generalized and localized gingivitis among Saudi subjects.
Keywords
Plaque, Gingivitis, Saudi population, Adult gingivitis, Periodontology, Prevalence
Introduction
Dental plaque biofilm-induced gingivitis is the most common form of periodontal disease [1], after dental caries. Affecting more than 75% of the population worldwide [2,3]. In general, gingivitis begins in early childhood, and becomes more prevalent and severe with age [4,5]. Dental plaque biofilm-induced gingivitis is defined at the site level as “an inflammatory lesion resulting from interactions between the dental plaque biofilm and the host’s immuneinflammatory response, which remains contained within the gingiva and does not extend to the periodontal attachment (cementum, periodontal ligament and alveolar bone). Such inflammation remains confined to the gingiva and does not extend beyond the mucogingival junction and is reversible by reducing levels of dental plaque at and apical to the gingival margin” [6].
The earliest clinical sign of inflammation is the transudation of gingival fluid. This thin and almost a cellular transudate is gradually superseded by a fluid consisting of serum plus leucocytes, the redness of the gingival margin arises partly from the aggregation and enlargement of blood vessels in the immediate sub epithelial connective tissue and the loss of keratinization of the facial aspects of gingiva. Swelling and loss of texture of the free gingiva reflect the loss of fibrous connective tissue and the semi liquidity-of the interfibrillar substance. Individually and collectively, the clinical symptoms of chronic gingivitis are rather vague, and usually painless. These features leave most patients tuna-ware of the disease and are generally underestimated by the dental practitioners. Chronic gingivitis rarely showsspontaneous bleeding. The fact that the gingival tissues can be provoked to bleed just by touching the gingival margin with a blunt instrument) as during tooth brushing or in assessing-the Gingival index (GI) suggests that the epithelial changes and the vascular transfigurments are quite conspicuous [7].
The classification of dental plaque Biofilm induced gingivitis defining the severity of gingivitis as a patient communication tool, but there are no objective clinical criteria for defining severity. Thus, in this context alone, the extent of gingivitis can be used to communicate “mild, moderate, and severe” gingivitis. Moreover, emerging evidence suggests that the contained gingivitis lesion may have systemic inflammatory consequences [8,9]. There is no robust evidence to clearly differentiate mild, moderate, and severe gingivitis, and definitions remain a matter of professional opinion. Methods of defining gingivitis may include: Defining percentages (e.g. mild ≤ 10%, moderate=10%-30%, severe ≥ 30% sites) Grading (e.g. grade 1 to 5 in 20% quintiles for % sites bleeding on probing).
Materials and Methods
One hundred and ninety-seven eligible participants in this cross-sectional study will be recruited from the routine dental patients who attended the oral diagnosis clinic at the dental hospital of Al-Farabi College in Jeddah, Saudi Arabia, from Nov 2019 to May 2020. The medical history of each subject will be recorded at the time of examination in a special recording form. Subjects who’s wearing fixed or removable prosthesis, or with orthodontic appliances, subjects under current periodontal treatment, tobacco smokers, female subjects who’s pregnant or using oral contraceptives, or subjects with any other systemic conditions that are known to predispose, or exaggerate gingival inflammation were not included. In addition, any subject who’s on antibiotics, antifungals. A minimum of 20 permanent teeth had to be present for inclusion in the study. The study is ethically approved by the Institutional Review Board of Al-Farabi College. All subjects will be asked to sign a consent form, and all procedures were undertaken in supervision of Dr.Hani Qataberi.
Results
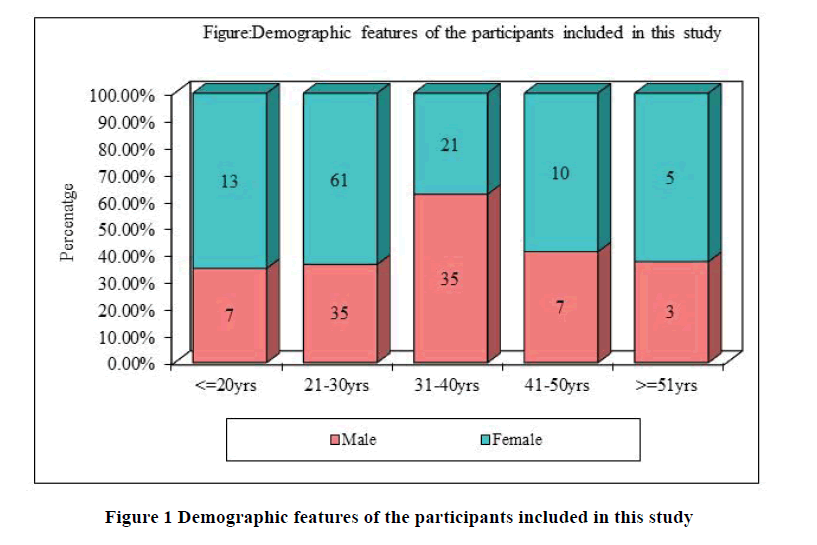
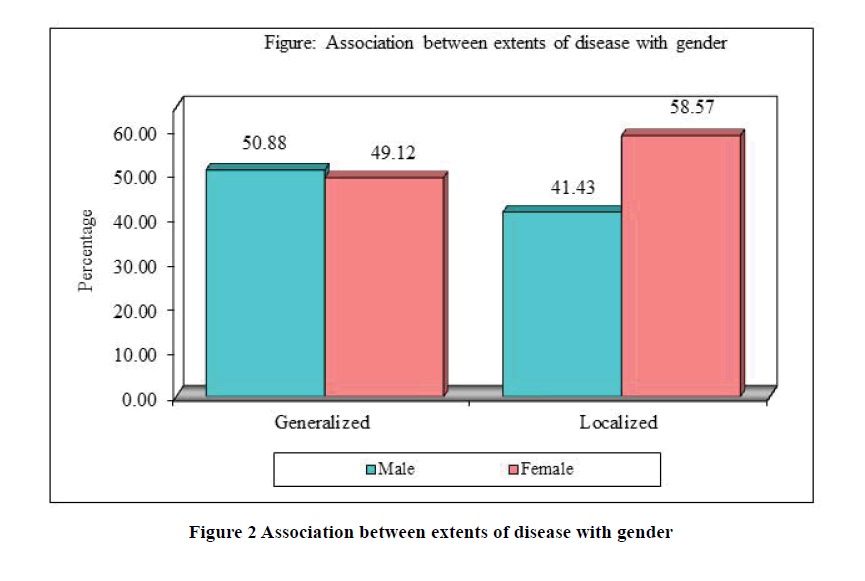
The study included 197 adult dentate subjects, 87 males (44.16%), and 110 females (55.84%), age ranging between ≤ 20 and ≥ 50 years (Figure 1). No significant association was found between extents of disease and gender (Chisquare= 1.4672; p=0.2260) (Figure 2 and Table 1).
| Gender | Generalized | % | Localized | % | Total | % |
|---|---|---|---|---|---|---|
| Male | 29 | 50.88% | 58 | 41.43% | 87 | 44.16% |
| Female | 28 | 49.12% | 82 | 58.57% | 110 | 55.84% |
| Total | 57 | 100% | 140 | 100% | 197 | 100% |
Chi-square=1.4672; p=0.2260
The results of the study showed that 100% of all participants had some form of Gingival inflammation (GI) according to bleeding on probing and plaque index tests. As shown in Table 2 the mean for bleeding on probing in male patients with generalized GI was 40.84 and localized GI was 13.54. While in female patients it was 41.43 for the generalized GI and 13.03 for the localized GI. The mean Plaque index (PI) for all subjects with generalized GI was 35.49 and 18.81 for the localized GI The mean PI for males was 31.9 in the generalized GI cases and 19.81 in the localized GI cases, whereas for females it was 39.21 generalized GI and 18.09 localized GI. A significant difference (p-value 0.0001) was observed between generalized and localized GI in terms of plaque index % and BOP % in total samples (males and females). It means that, the generalized group has significant higher mean scores of plaque index % and BOP % in total samples (males and females) as compared to localized group of total samples (Table 2).
| Gender | Variable | Extent of disease | Mean | SD | SE | t-value | p-value |
|---|---|---|---|---|---|---|---|
| Total | Plaque index % | Generalized | 35.49 | 15.82 | 2.1 | 6.56 | 0.0001,S |
| Localized | 18.81 | 16.33 | 1.38 | ||||
| BOP % | Generalized | 41.13 | 11.74 | 1.56 | 20.0182 | 0.0001,S | |
| Localized | 13.24 | 7.4 | 0.63 | ||||
| Male | Plaque index % | Generalized | 31.9 | 14.52 | 2.7 | 3.2235 | 0.0018,S |
| Localized | 19.81 | 17.37 | 2.28 | ||||
| BOP % | Generalized | 40.84 | 11.5 | 2.14 | 13.4042 | 0.0001,S | |
| Localized | 13.54 | 7.39 | 0.97 | ||||
| Female | Plaque index % | Generalized | 39.21 | 16.5 | 3.12 | 6.0863 | 0.0001,S |
| Localized | 18.09 | 15.63 | 1.73 | ||||
| BOP % | Generalized | 41.43 | 12.2 | 2.31 | 14.6248 | 0.0001,S | |
| Localized | 13.03 | 7.44 | 0.82 |
Comparison of male and females with plaque index % and BOP % in Generalized and localized was done by independent t test (Table 3). A non-significant difference was observed between male and female patients with plaque index % and BOP % in total samples, generalized group and localized group. It means that, the male and females have similar plaque index % and BOP % mean scores in total samples, generalized group and localized group.
| Samples | Variable | Gender | Mean | SD | SE | t-value | p-value |
|---|---|---|---|---|---|---|---|
| Total | Plaque index % | Male | 23.84 | 17.36 | 1.86 | 0.1446 | 0.8852 |
| Female | 23.47 | 18.29 | 1.74 | ||||
| BOP % | Male | 22.64 | 15.71 | 1.68 | 1.0735 | 0.2844 | |
| Female | 20.26 | 15.25 | 1.45 | ||||
| Generalized | Plaque index % | Male | 31.9 | 14.52 | 2.7 | -1.7791 | 0.0807 |
| Female | 39.21 | 16.5 | 3.12 | ||||
| BOP % | Male | 40.84 | 11.5 | 2.14 | -0.1871 | 0.8523 | |
| Female | 41.43 | 12.2 | 2.31 | ||||
| Localized | Plaque index % | Male | 19.81 | 17.37 | 2.28 | 0.6121 | 0.5415 |
| Female | 18.09 | 15.63 | 1.73 | ||||
| BOP % | Male | 13.54 | 7.39 | 0.97 | 0.3986 | 0.6908 | |
| Female | 13.03 | 7.44 | 0.82 |
A significant and higher plaque index % was observed in females of generalized group and minimum in females of localized group followed by males of generalized group males of localized group (Table 4).
| Interactions | Males in Generalized | Males in Localized | Females in Generalized | Females in Localized |
|---|---|---|---|---|
| Mean | 31.9 | 19.81 | 39.21 | 18.09 |
| SD | 14.52 | 17.37 | 16.5 | 15.63 |
| Males in generalized | - | |||
| Males in localized | p=0.0008* | - | ||
| Females in generalized | p=0.0422* | p=0.0001* | - | |
| Females in localized | p=0.0004* | p=0.6331 | p=0.0001* | - |
| *p<0.05 |
A significant and higher BOP % was observed in females of generalized group and minimum in females of localized group followed by males of generalized group males of localized group (Table 5).
| Interactions | Males in Generalized | Males in Localized | Females in Generalized | Females in Localized |
|---|---|---|---|---|
| Mean | 40.84 | 13.54 | 41.43 | 13.03 |
| SD | 11.5 | 7.39 | 12.2 | 7.44 |
| Males in generalized | - | |||
| Males in localized | p=0.0001* | - | ||
| Females in generalized | p=0.7678 | p=0.0001* | - | |
| Females in localized | p=0.0001* | p=0.7986 | p=0.0001* | - |
*p<0.05
A significant and positive correlation was observed between plaque index % and BOP % in total, localized group, male and female samples. It means the plaque index % and BOP % are dependent on each other in total, localized group, male and female samples (Table 6).
| Samples | Correlation between plaque index % and BOP % in | ||
|---|---|---|---|
| r-value | t-value | p-value | |
| Total | 0.80646 | 10.115 | 0.0001* |
| Generalized | 0.196706 | 1.4879 | 0.1425 |
| Localized | 0.603296 | 5.6101 | 0.0001* |
| Male | 0.473561 | 3.9875 | 0.0002* |
| Female | 0.752943 | 8.4852 | 0.0001* |
*p<0.05
Discussion
The studies on the prevalence of plaque-induced gingivitis in different populations are useful as it is a risk factor for periodontitis, which will help in early preventive efforts. The Chinese before 3500 years first described gingivitis and it is often difficult to estimate the worldwide prevalence due to differences in study populations, definitions, diet, genetic, and other ecological factors [10,11]. Thus, this study aimed to evaluate the prevalence and severity of plaqueinduced gingivitis among the Saudi population residing in the city of Jeddah.
Epidemiological data shows that plaque-induced gingivitis is prevalent in all age groups of dentate populations, which is a common form of periodontal disease [12-15]. One of the peculiar features of plaque-induced gingivitis is the complete reversibility of the tissue alterations on the removal of the dental biofilm [16]. The findings of our study showed that the prevalence of generalized gingivitis was 28.93%, whereas localized gingivitis was seen in 71.06% thus all participants had some form of gingival inflammation. A 30-year trend (1973-2003) study conducted in an adult Swedish population showed a prevalence of 95% gingivitis [17]. In America, a study done by Oppermann, et al. reported a prevalence of 93.9% [18], and a prevalence of 97.9% was reported among the Chinese adult population in another study done by Zhang, et al. [14]. Our study findings were similar to a recent study done in the Riyadh province of Saudi Arabia, which showed a prevalence of 100% [19].
In our study, the Plaque index (PI) and Bleeding on probing (BOP) showed statistically significant higher scores in people with generalized gingivitis compared to localized gingivitis. It is well documented that Gram-positive bacteria such as Actinomyces viscosus, Parvimonas micra, Streptococcus species, and Gram-negative anaerobes like Campylobacter gracilis, Fusobacterium nucleatum, Prevotella intermedia, Veillonella parvula are associated with gingivitis [20]. Efforts taken by scientists to identify the difference in plaque microflora among people with different degrees of gingival inflammation failed to show significant differences [21]. According to the latest dental plaque hypothesis that is known as Keystone Pathogen Hypothesis (KPH), low-abundance microbial pathogens (keystone pathogen) such as Porphyromonas gingivalis can cause inflammatory disease by increasing the quantity of the normal microbiota and by changing its composition which will help them not only helps them to survive but also other bacteria to multiply [22].
The reason for this higher plaque index and its association with generalized gingivitis in our study findings could be explained based on this hypothesis. A study done by Sreenivasan, et al. demonstrated that plaque deposits and higher gingival inflammation were seen more in posterior regions compared to anterior regions [23].
Even though the findings of our study didn’t show statistically significant differences in both PI scores and BOP between two genders, it showed statistically significant higher PI scores in females with generalized gingivitis only when compared to males. The prevalence of BOP in our study didn’t show significant difference even though it was more in males (22.64%) compared to females (20.26%). This prevalence is lesser when compared to the study conducted by Idrees et al. in Riyadh that reported a BOP of 28.8%, which was also higher in males compared to females [19]. These findings of male predominance in higher Pl and BOP are supported by various studies done in many other countries [19,24-26]. The possible explanation for this higher prevalence could be explained by factors like poor attitude towards oral health behavior such as lesser dental visits, poor oral hygiene practices, and less grooming sense among males compared to females [27-29].
Conclusion
The current study demonstrated that higher plaque deposits were significantly associated with generalized gingivitis than localized gingivitis among the Saudi population in Jeddah. Oral health education including appropriate plaque control measures such as complaint brushing technique, use of chemical plaque control aids such as mouth rinses and utilization of dental services behavior modifications should be emphasized to people of all sectors to tackle this issue. A multicenter study that addresses the relationship of variables such as oral hygiene practices, utilization of dental services, dietary pattern, oral health educational level, use of medications, chronic diseases, and socioeconomic status involving a larger sample is suggested in this regard. Community preventive programs should be monitored and if necessary, should re-implemented on a large and effective scale.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Califano, Joseph V., and Science Research. "Position paper: Periodontal diseases of children and adolescents." Journal of Periodontology, Vol. 74, No. 11, 2003, p. 1696.
- Petersen, Poul Erik. "The World Oral Health Report 2003: continuous improvement of oral health in the 21st century-the approach of the WHO Global Oral Health Programme." Community Dentistry and Oral Epidemiology, Vol. 31, 2003, pp. 3-24.
- Papapanou, P. N. "Epidemiology of periodontal diseases: An update." Journal of the International Academy of Periodontology, Vol. 1, No. 4, 1999, p. 110.
- Stamm, John W. "Epidemiology of gingivitis." Journal of Clinical Periodontology, Vol. 13, No. 5, 1986, pp. 360-66.
- Russell, A. L. "The prevalence of periodontal disease in different populations during the circumpubertal period." Periodontal Disease Prevalence in Pubesce, Vol. 42, 1971, pp. 508-12.
- Chapple, Iain LC, et al. "Periodontal health and gingival diseases and conditions on an intact and a reduced periodontium: Consensus report of workgroup 1 of the 2017 World Workshop on the Classification of Periodontal and Peri‐Implant Diseases and Conditions." Journal of Periodontology, Vol. 89, 2018, pp. S74-84.
- Lang, Niklaus P., Marc A. Schätzle, and Harald Löe. "Gingivitis as a risk factor in periodontal disease." Journal of Clinical Periodontology, Vol. 36, No. 10, 2009, pp. 3-8.
- Wohlfeil, Martin, et al. "Degree of gingivitis correlates to systemic inflammation parameters." Clinica Chimica Acta, Vol. 401, No. 1, 2009, pp. 105-09.
- Eberhard, Jörg, et al. "Experimental gingivitis induces systemic inflammatory markers in young healthy individuals: A single-subject interventional study." PLoS One, Vol. 8, No. 2, 2013, p. e55265.
- Clerehugh, V. "The changing face of periodontal epidemiology." Community Dental Health, Vol. 10, 1993, p. 19.
- Trombelli, Leonardo, et al. "Plaque‐induced gingivitis: Case definition and diagnostic considerations." Journal of Clinical Periodontology, Vol. 45, No. 20, 2018, pp. S44-67.
- Ismail, A. I., et al. "Natural history of periodontal disease in adults: findings from the Tecumseh Periodontal Disease Study, 1959-87." Journal of Dental Research, Vol. 69, No. 2, 1990, pp. 430-5.
- Australian Research Centre for Population Oral Health. "Periodontal diseases in the Australian adult population." Australian Dental Journal, Vol. 54, No. 4, 2009, pp. 390-3.
- Zhang, Jincai, et al. "Severity and prevalence of plaque-induced gingivitis in the Chinese population." Compendium of Continuing Education in Dentistry, Vol. 31, No. 8, 2010, pp. 624-9.
- Kundu, Debabrata, Ritesh Mehta, and Shallu Rozra. "Periodontal status of a given population of West Bengal: An epidemiological study." Journal of Indian Society of Periodontology, Vol. 15, No. 2, 2011, p. 126.
- Lang, Niklaus P., Marc A. Schätzle, and Harald Loe. "Gingivitis as a risk factor in periodontal disease." Journal of Clinical Periodontology, Vol. 36, 2009, pp. 3-8.
- Hugoson A, Koch G. "Thirty year trends in the prevalence and distribution of dental caries in Swedish adults (1973-2003)." Swedish Dental Journal, Vol. 32, No. 2, 2008, pp. 57-67.
- Oppermann, Rui V., et al. "Epidemiology of periodontal diseases in adults from Latin America." Periodontology, Vol. 67, No. 1, 2015, pp. 13-33.
- Idrees, Majdy M., et al. "Prevalence and severity of plaque-induced gingivitis in a Saudi adult population." Saudi Medical Journal, Vol. 35, No. 11, 2014, p. 1373.
- Tatakis, Dimitris N., and Purnima S. Kumar. "Etiology and pathogenesis of periodontal diseases." Dental Clinics, Vol. 49, No. 3, 2005, pp. 491-516.
- Lie, M. A., et al. "Oral microbiota in subjects with a weak or strong response in experimental gingivitis." Journal of Clinical Periodontology, Vol. 22, No. 8, 1995, pp. 642-7.
- Hajishengallis, G., R. P. Darveau, and M. A. Curtis. "The keystone-pathogen hypothesis" Nature Reviews Microbiology, Vol. 10, No. 10, 2012, pp. 717-25.
- DeVizio, PK Sreenivasan W., et al. "Regional differences within the dentition for plaque, gingivitis, and anaerobic bacteria." The Journal of Clinical Dentistry, Vol. 21, No. 1, 2010, pp. 13-9.
- Mostafa, Basma, and Ibrahim El-Refai. "Prevalence of plaque-induced gingivitis in a sample of the adult Egyptian population." Open Access Macedonian Journal of Medical Sciences, Vol. 6, No. 3, 2018, p. 554.
- Ababneh, Khansa Taha, Zafer Mohammad Faisal Abu Hwaij, and Yousef S. Khader. "Prevalence and risk indicators of gingivitis and periodontitis in a multi-centre study in North Jordan: A cross sectional study." BMC Oral Health, Vol. 12, No. 1, 2012, p. 1.
- Li, Yiming, et al. "Prevalence and severity of gingivitis in American adults." American Journal of Dentistry, Vol. 23, No. 1, 2010, p. 9.
- AlGhamdi, Ali S., et al. "Gingival health and oral hygiene practices among high school children in Saudi Arabia." Annals of Saudi Medicine, Vol. 40, No. 2, 2020, pp. 126-35.
- Alasqah, Mohammed, et al. "The effect of gingival bleeding on oral home care practices in Saudi Arabia." Journal of Family Medicine and Primary Care, Vol. 8, No. 8, 2019, p. 2696.
- Farsi, J. M. A. "Dental visit patterns and periodontal treatment needs among Saudi students." EMHJ-Eastern Mediterranean Health Journal, Vol. 16, No. 7, 2010, pp. 801-6.