Research - International Journal of Medical Research & Health Sciences ( 2022) Volume 11, Issue 12
Predicting Urinary Tract Infection in Jaundiced Newborns by Phototherapy Response
Fatma Simsek1, S. Umit Sarici1, Demet Soylu1*, Muhittin A. Serdar2, Murat Ozcan3 and Dilek Sarici42Department of Biochemistry and Clinical Biochemistry, Acıbadem, University Faculty of Medicine, Ankara, Turkey
3Department of Pediatrics, Sereflikochisar State Hospital, Ankara, Turkey
4Division of Neonatology, Department of Pediatrics, Health Sciences University, Kecioren, Education and Research Hospital, Ankara, Turkey
Demet Soylu, Division of Neonatology, Department of Pediatrics, Ufuk University Faculty of Medicine, Ank, Turkey, Email: drdemetsoylu@gmail.com
Received: 26-Aug-2022, Manuscript No. ijmrhs-22-84189; Editor assigned: 30-Aug-2022, Pre QC No. ijmrhs-22-84189 (PQ)_; Reviewed: 10-Sep-2022, QC No. ijmrhs-22-84189 (Q); Revised: 10-Dec-2022, Manuscript No. ijmrhs-22-84189 (R); Published: 23-Dec-2022
Abstract
Objective: This study aimed to compare the post-phototherapy decrease in Serum Total Bilirubin (STB) levels of newborns diagnosed to have idiopathic pathologic hyperbilirubinemia with and without Urinary Tract Infection (UTI) and to determine a critical cut-off value of percent decrease in STB with phototherapy in predicting the diagnosis of UTI. Methods: Urine samples for microscopic examination and bacteriologic culture were obtained in 381 newborns of whom all other possible etiologic causes of neonatal hyperbilirubinemia were excluded. Newborns with and without positive urine culture (Groups I and II) were compared concerning demographic findings and laboratory data. The Receiver Operating Characteristic (ROC) curve was constituted. Results: Post-phototherapy STB level was significantly higher (P=0.0002) and the decrease in STB level with phototherapy was significantly lower (P<0.0001) in Group I when compared to Group II. The critical cut-off value of STB decrease in predicting UTI was 47.9%. Conclusions: A relatively inadequate phototherapy response (STB decrease of <47.9%) should raise the suspicion of UTI, and further urine examinations should be performed considering that 40% of newborns with a decrease of <47.9% in STB despite phototherapy may have UTI and 90% of those with a decrease of ≥ 47.9% do not have UTI
Keywords
Hyperbilirubinemia, Newborn, Phototherapy, Urinary Tract Infection (UTI)
Introduction
Neonatal jaundice resulting from the accumulation of unconjugated bilirubin in the skin is encountered in 60% to 80% of newborns in the first week of life. This type of jaundice may reportedly be the first sign of a serious bacterial infection, and Urinary Tract Infection (UTI) [1,2]. The physiopathological relationship between UTI and neonatal jaundice has been investigated in a limited number of studies. These studies have rather focused on late (≥ 10 days), prolonged, or conjugated neonatal jaundice [3-7]. However, this relationship has been investigated in very few studies including newborns with early (<10 days) neonatal jaundice [2,8-10]. On the other hand, international reputable organizations like the American Academy of Pediatrics (AAP) do not routinely recommend urine examinations such as urinalysis or urine culture in the evaluation of early neonatal jaundice [11]. In some studies, it has been reported that post-phototherapy Serum Total Bilirubin (STB) levels were higher in jaundiced newborns with UTI in comparison to those without UTI [8,10]. In one other study, however, post-phototherapy STB levels did not differ between the jaundiced newborns with and without UTI.
However parameters aiming to detect the critical STB decrease (with phototherapy) which could be useful predicting the jaundiced newborns with UTI have, to our knowledge, not been investigated in any of these studies. In our particular observation, we noticed that an adequate phototherapy response could not be obtained despite intensive phototherapy in some babies with significant hyperbilirubinemia, prolonged jaundice woul develop and even UTI would be detected later in progress in these babies in whom UTI was not investigated at the onset. Starting from this point of observation we prospectively aimed to compare newborns with UTI plus significant hyperbilirubinemia versus those with only significant hyperbilirubinemia based on response phototherapy (as a percent decrease in STB after phototherapy). We thus aimed to investigate if a probable inadequate phototherapy response could be used to predict the UTI in a newborn with significant hyperbilirubinemia and to determine the critical cut-off value of percent decrease in STB with phototherapy that could be useful in predicting the UTI in a newborn with significant Hyperbilirubinemia.
Key Notes
• UTI may play role in the Etiology/Pathophysiology of significant neonatal hyperbilirubinemia.
• There is not a reported critical cut-off value of STB decrease after a 24-hour high-intensity phototherapy to be used in predicting the presence of a UTI.
• A relatively inadequate phototherapy response (STB decrease of <47.9%) should raise the suspicion of a simultaneous UTI, which should be further searched for
Methods
Study Design and Patients
The study was conducted at the Division of Neonatology, Department of Pediatrics, Ufuk University Faculty of Medicine, Ankara, Turkey between January 2016 and November 2019. The study was approved by the Ethics Committee of the Ufuk University Faculty of Medicine with approval number 20191216/1.
During the study period, all newborns with a gestational age of ≥ 35 weeks who were diagnosed to have significant hyperbilirubinemia and who would undergo phototherapy treatment were included in the study. Urine samples for urine culture and microscopic examination were obtained with urine bags from all newborns to determine if the cause of pathologic jaundice was UTI. If there were findings suggestive of UTI such as leukocyte esterase positivity, nitrite positivity, presence of at least 10 leukocytes in centrifuged urine sediment in each field at 40 magnification under the microscope, or growth of a single bacterium in urine culture with a CFU of ≥ 105, urine culture was repeated with aseptic bladder catheterization technique after written and/or verbal informed consent was obtained. The diagnosis of UTI was established if a single bacterium of a CFU of 103 was isolated with this technique [12]. Newborns diagnosed to have UTI as the etiologic factor of significant hyperbilirubinemia constituted Group I, and those without UTI in the etiologic evaluation of significant hyperbilirubinemia constituted Group II. The diagnosis of significant hyperbilirubinemia was established based on STB values versus postnatal age and risk status of the newborns [11,13].
As our primary aim was to compare newborns with significant hyperbilirubinemia plus UTI and those with significant hyperbilirubinemia but without UTI, newborns with the other causes of hyperbilirubinemia which may interfere with the rate of bilirubin decline with phototherapy such as prematurity (<35 gestational weeks), late (≥ 10 days) Neonatal Hyperbilirubinemia, Neonatal Sepsis, is an immune Hemolytic disease (ABO, Rh or subgroup incompatibility), Nonimmune Hemolytic Disease (Erythrocyte enzyme or membrane defects), enclosed hemorrhage (Cephalohematoma, surreal, hepatic or intracranial hemorrhage, severe bruising), hypothyroidism, congenital malformations, and respiratory distress resulting in the late initiation of oral feedings were excluded from the study. In all the cases in the study gender, gestational age as weeks, route of birth, birth weight, weight loss as percent in comparison to birth weight on admission, postnatal age on admission, maternal age, blood groups of mother and newborn pairs, reticulocyte count, the result of direct Coombs test, hemoglobin, hematocrit, free T4, TSH, serum direct bilirubin levels on admission, STB levels on admission and 24 hours after initiation of phototherapy, the decline in STB levels as percent after 24 hours of phototherapy, whether there is the growth of any bacteria in urine cultures, type and amount of bacteria growing in the culture (if there is), results of microscopic urine examinations, and the presence of any genitourinary abnormality detected by ultrasonographic examination were recorded.
Interventions
Intensive phototherapy was given with a high-intensity special blue light LED phototherapy device (EO Baby Led Force (110-240 VAC, Max. 0,3 A., 50/60 Hz., Tip B, class 2) emitting special blue light with LED light source. Spectral irradiance of the devices used was periodically (weekly) measured during the study period with a radiometer (Minolta Air-Shields Vickers Fluoro-Lite Meter 451) measuring irradiance between 400 nm to 500 nm, recorded regularly, and sources of LED light were changed with new ones if mean spectral irradiance decreased below 80 µw/cm²/nm. The mean spectral irradiance measured during the study period was 101.2 µw/cm²/nm ± 5.4 µw/cm²/nm. The eye mask was routinely used during phototherapy. Phototherapy was performed on the whole body except for the areas of the eye mask and gonad-saving diaper. Phototherapy was performed under the plexiglass of the incubator from a 45 cm distance with changes of the torso (Prone/supine) of the baby every 2 hours. Phototherapy was continued for at least 24 hours except for short breaks for feeding or diaper changing.
Urine collection for urine samples with a urine bag was performed after cleaning the genital area from the center (Urethral meatus) to the periphery three times with a 10% povidone-iodine solution and sticking a sterile genderappropriate urine bag. Bladder catheterization was performed using a 4 or 6-F feeding catheter with an aseptic technique after feeding and fixation of the infant. The urine sample for standard examination was tested with Multistix 10 (Bayer, Germany), and the sample for microscopic examination was centrifuged at 2000 rpm for 5 minutes before microscopic evaluation. Urine samples for culture were sent immediately to the microbiology laboratory for standard quantitative culture, and the growth of single-type microorganisms on a culture medium with an amount of at least 1000 CFU/mL was accepted as UTI [12].
Hematologic and biochemical laboratory tests were performed with Beckman Coulter Gen-S automatic autoanalyzer, and STB and direct bilirubin levels were measured with the colorimetric method (Diazotized sulfanilic acid reaction; Roche Diagnostics GmbH, Mannheim, Germany).
During the study period, all newborns underwent a routine abdominal and urinary ultrasonographic examination to show a possible enclosed hemorrhage or urinary system abnormality, and the results of the ultrasonographic examinations were recorded.
Statistical Analysis
Study groups (Groups I and II) compared demographic data, laboratory findings, and results of ultrasonographic investigations. SPSS 18.0 program was used in the statistical analysis of the data. The Shapiro-Wilk test was used in determining normal distribution. Of continuously variable parameters, maternal age, gestational age, birth weight, age on admission, weight on admission and weight loss in comparison to birth weight, serum direct bilirubin levels, levels of STB before and after phototherapy, hemoglobin levels and rate of decrease in STB levels with phototherapy at 24th hour calculated as percent were compared with independent sample t-test. Values before and after phototherapy were compared with paired t-tests. Nominal values, such as sex, route of birth, presence or absence of maternal genitourinary infection in antenatal history, and presence of ultrasonographic genitourinary abnormality were compared with the χ2 test. Receiver Operating Characteristic (ROC) curve analysis was used to determine the optimal (Cut-off value) rate of decrease in STB level with phototherapy at the 24th hour to predict the newborns with both UTI and significant hyperbilirubinemia among all the newborns with significant hyperbilirubinemia, and diagnostic performance of rate of decrease in STB level in discriminating jaundiced newborns with and without UTI was determined by calculating the area under the ROC curve (AUC). These calculations were made using MedCalc version 15.8. Values were given as mean ± SD and median 25%-75% range. A p-value of ≤ 05 was considered statistically significant.
Results
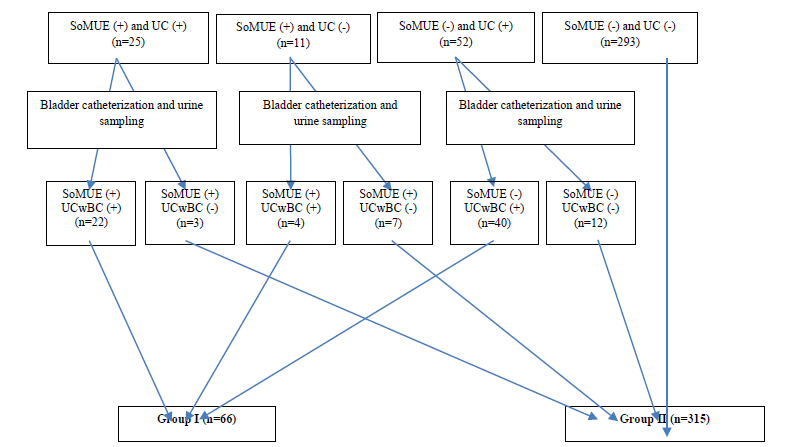
A total of 481 newborns with significant hyperbilirubinemia were initially included in the study. Of these, 91 cases were excluded from the study because of the following exclusion criteria: Gestational age <34 weeks; n=16, is an immune hemolytic disease; n=34, jaundice which is not early (>10 days) or prolonged (>14 days); n=13, failure to start oral/enteral feeding in the first 24 hours due to respiratory distress; n=4, enclosed hemorrhage; n=8, congenital hypothyroidism; n=2, sepsis; n=9, congenital anomaly; n=5. Urine samples were obtained via urine bags from the remaining 390 cases. Nine cases in which bacterial growth was detected in their urine cultures were further excluded as their parents did not give consent for bladder catheterization. Of the remaining 381 cases, 293 did not have any positivity on standard or microscopic urine examination and had no bacterial growth on urine culture. Urine samples for culture were obtained via bladder catheterization in 25 cases in whom there were both standard or microscopic urine examination and urine culture positivity, in 11 cases in whom there were standard or microscopic urine examination positivity but urine culture negativity and in 52 cases in whom there were standard or microscopic urine examination negativity but urine culture positivity with urine bag samples.
There was urine culture positivity with bladder catheterization in 22 out of 25 cases with both standard or microscopic urine examination and urine culture positivity. There was urine culture positivity with bladder catheterization in 4 out of 11 cases with standard or microscopic urine examination positivity but urine culture negativity, and there was urine culture positivity with bladder catheterization in 40 out of 52 cases with standard or microscopic urine examination negativity but urine culture positivity with urine samples obtained via urine bag. Cases with bacterial growth in their urine samples obtained via bladder catheterization constituted Group I (n=66), whereas cases with no bacterial growth and normal standard or microscopic urine examination in their urine samples obtained via urine bag (n=293) and cases with no bacterial growth in their urine samples obtained via bladder catheterization (n=22) constituted Group II (Totally, n=315). A flow diagram of the distribution of cases according to the characteristics of urine examination results is given in Figure 1.

A comparison of the cases in two groups concerning demographic data and laboratory parameters is given in Table 1.
| Parameter | Group I (n=66) | Group II (n=315) | p-value |
|---|---|---|---|
| Gender (Male/Female)* | 56/10 | 159/156 | <0.0001 |
| Route of birth (Cesarean/Vaginal)* | 28/38 | 169/146 | 0.097 |
| Maternal genitourinary infection in antenatal history (Yes/No)* | 21/45 | 114/201 | 0.4995 |
| Gestational age (Days)** | 265.45 ± 11.27 | 263.22 ± 10.49 | 0.1222 |
| Maternal age (Years)** | 29.54 ± 6.10 | 29.19 ± 5.43 | 0.6402 |
| Age on admission (Days)** | 6.37 ± 1.82 | 6.01 ± 1.74 | 0.1286 |
| Birth weight (Gr)** | 3144.24 ± 499.84 | 3047.56 ± 471.65 | 0.1349 |
| Weight loss on admission (%)** | 5.74 ± 4.31 | 5.95 ± 3.80 | 0.6818 |
| Hemoglobin (g/dl)** | 17.11 ± 1.92 | 17.18 ± 1.69 | 0.7541 |
| Serum direct bilirubin level (mg/dl)** | 0.6694 ± 0.1345 | 0.6252 ± 0.1556 | 0.0328 |
| Presence of ultrasonographic genitourinary abnormality (Yes/No)* | 22/44 | 6/309 | <0.0001 |
|
*: Parameters were compared with the Chi-square test. |
|||
|
**: Values were given as mean ± standard deviation and compared with the t-test. |
|||
There were no statistically significant differences between the two groups regarding parameters such as route of birth, presence of maternal genitourinary infection in antenatal history, gestational age, maternal age, age on admission, birth weight, weight loss on admission, and hemoglobin level. The number of male newborns was higher (56/10 versus 159/156, p<0.0001), and serum direct bilirubin levels were higher (0.6694 ± 0.1345 mg/dl versus 0.6252 ± 0.1556 mg/dl, p=0.0328) in Group I when compared to Group II. The presence of any genitourinary abnormality was higher in Group I when compared to Group II (22/44 versus 6/309) (p<0.0001). There were bilaterally grade I pelviectasis (n=4), unilaterally grade I pelviectasis (n=12), bilaterally grade II pelviectasis (n=2), unilaterally grade II pelviectasis (n=2), left renal hydronephrosis (n=1) and unilateral stenosis in the ureteropelvic junction (n=1) in Group I. There were bilaterally grade I pelviectasis (n=1), unilaterally grade I pelviectasis (n=3), and nephrocalcinosis (n=2) in Group II.
In Group I Gram (-) and (+) bacteria grew in bacteriologic culture in 48 and 18 newborns, respectively. Gram (-) microorganisms were Klebsiella spp. (23/66=34.8%), Escherichia Coli (24/66=36.3%) and Serratia species (1/66=1.51%), and Gram (+) microorganisms were Enterococcus (7/66=10.6%), coagulase-negative Staphylococcus (2/66=3.03%), Staphylococcus Aureus (4/66=6.06%), Staphylococcus Epidermidis (4/66=6.06%) and group A β hemolytic Streptococcus (1/66=1.51%). The mean number of CFU was 85606 ± 27519.4 in Group I. Pyuria was detected in 26 newborns (26/66; 39%), and in 10 newborns (10/315; 3.17%) in Groups I and II, respectively, however, bacteriologic culture was not positive in any of the cases in the latter group.
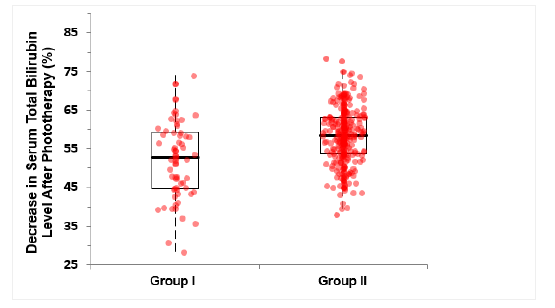
A comparison of the responses of the newborns in the study groups to 24-hour phototherapy treatment is given in Table 2. Post-phototherapy STB levels were significantly higher in Group I in comparison to Group II (p=0.0002), whereas STB levels before phototherapy were not significantly different between the groups (p=0.2322). The decline in STB levels as a percent after 24 hours of phototherapy was significantly lower in Group I when compared to Group II (p<0.0001) (Table 2) (Figure 2).
| Parameter | Group I (n=66) | Group II (n=315) | p-value |
|---|---|---|---|
| Serum total bilirubin before phototherapy (mg/dl)* | 19.90 ± 2.83 | 20.39 ± 3.06 | 0.2322 |
| Serum total bilirubin after phototherapy (mg/dl)* | 9.52 ± 2.53 | 8.49 ± 1.92 | 0.0002 |
| Rate of decrease in serum total bilirubin level with phototherapy at 24th hour* | 52.38 ± 9.99 | 58.37 ± 7.35 | <0.0001 |
|
*: Values are given as mean ± standard deviation and compared with the t-test. |
|||
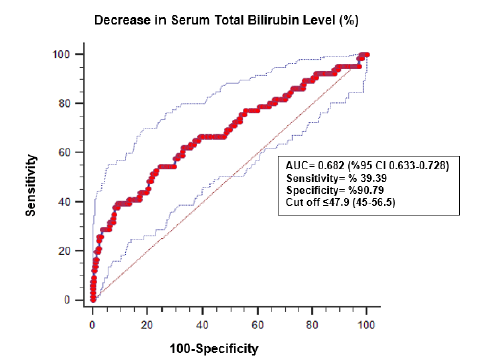
According to the results of the ROC analysis performed to determine those newborns with both significant hyperbilirubinemia and UTI among all newborns with significant hyperbilirubinemia, cut-off values and their confidence intervals determined based on high sensitivity and specificity values are given in Table 3 and 4.
| Sensitivity | Specificity | 95% Confidence interval | Cut off value |
|---|---|---|---|
| 80 | 35.62 | 19.75%-50.53% | ≤ 60.98 |
| 90 | 19.56 | 2.22%-30.48% | ≤ 64.44 |
| 95 | 10.48 | 1.57%-25.46% | ≤ 68.07 |
| 97.5 | 2.86 | 0.95%-20.96% | ≤ 71.86 |
| 99 | 1.9 | 0.32%-3.81% | ≤ 73.80 |
| Specificity | Sensitivity | 95% Confidence interval | Cut off value |
|---|---|---|---|
| 80 | 44.7 | 28.98%-57.58% | ≤ 51.95 |
| 90 | 39.39 | 28.79%-53.03% | ≤ 48.25 |
| 95 | 28.79 | 18.18%-41.77 | ≤ 45.47 |
| 97.5 | 21.21 | 0.00%-0.00% | ≤ 44.16 |
| 99 | 13.64 | 0.00%-0.00% | ≤ 40.56 |
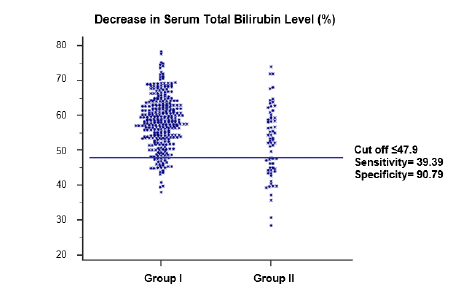
Cut off the value of decline in STB level as percent in predicting UTI in newborns with significant hyperbilirubinemia was determined as the most ideal point of sum of sensitivity and specificity using Youden Index J in ROC analysis, and the cut-off value was calculated as 47.9%. At this cut-off point sensitivity and specificity were 39.39% and 90.79%, respectively, and AUC was 0.682. Data of Youden Index J are given in Table 5. A comparison of the study groups according to the cut-off values and ROC curve is given in Figures 3 and 4.
| “Youden Index J” | 0.3019 |
|---|---|
| 95% Confidence interval | 0.1715-0.3864 |
| Sensitivity (%) | 39.39 |
| Specificity (%) | 90.79 |
Results of the overall analysis show that 40% of newborns with significant hyperbilirubinemia in whom phototherapy is administered and less than 47% decline in STB level is achieved may simultaneously have UTI, and 90% of newborns with a ≥ 47.9% decline in STB level with phototherapy do not have UTI.
Discussion
Although the relationship between neonatal jaundice and UTI has not been elucidated, some recent studies claimed that UTI may be responsible for the etiology of idiopathic unexplained hyperbilirubinemia [14-20].
Indirect hyperbilirubinemia is suggested to occur due to hemolysis caused by E. coli and other gram-negative bacteria. Conjugated hyperbilirubinemia related to UTI is, however, suggested to be associated with cholestasis. Although how UTI causes cholestasis is not exactly known, disorders of hepatic microcirculation and direct bacterial or endotoxin-mediated products are suggested responsible for the etiology [14].
endotoxin-mediated products are suggested responsible for the etiology [14]. In studies investigating the relationship between UTI and neonatal jaundice, the frequency of UTI has been reported to be between 5.5% and 21.1% [10,15,16]. In the present study, the frequency of UTI of 17.3% in 381 newborns in whom all other causes of neonatal jaundice have been excluded is in concordance with the findings of those other studies.
The role of UTI in the etiology of prolonged jaundice has been emphasized before, however, its role in idiopathic indirect hyperbilirubinemia with unexplained etiology has been studied in a limited number of studies. Garcia, ve Nager reported that most of the jaundiced newborns in whom hyperbilirubinemia began after 8 days of life had UTI, and Pashapour et al claimed that jaundiced newborns with 2 weeks to 4 weeks old had very likely UTI [6]. In the present study, newborns with an age of ≥ 10 days were excluded, and thus, the role of UTI in the etiology of significant hyperbilirubinemia was investigated in newborns with early-type jaundice only.
In several studies investigating the relationship between neonatal jaundice and UTI, UTI has been reported predominantly in male newborns. The male gender predominance in our study (56 in 66; 84.8%) following the published studies.
Garcia and Nager, in their series of 160 newborns, have detected UTI in all of the cases with conjugated hyperbilirubinemia. Higher serum direct bilirubin levels in newborns with UTI in comparison to those without UTI. In their series of 50 newborns with UTI and jaundice, Lee et al have reported much more cases of UTI caused by E.coli in comparison to those caused by other bacteria in newborns with conjugated hyperbilirubinemia [18]. Emamghorashi et al have reported an increased risk of UTI in newborns with a direct bilirubin level of >1.6 mg/dl [19]. Although we did not detect any case with conjugated hyperbilirubinemia in this study, newborns with UTI had higher serum direct bilirubin levels when compared to those without UTI
Various studies reported varying rates of genitourinary abnormality in newborns with UTI and neonatal jaundice [2,4,5,8-10,20]. In the present study, abdominal ultrasonography was performed in all cases which were not performed routinely in similar studies, and the rate of genitourinary abnormality was significantly higher in Group I when compared to Group II (22 in 66 versus 6 in 315; p<0.0001). This high (33.3%) rate of ultrasonographic genitourinary abnormality confirms the necessity of performing an ultrasonographic examination in newborns with UTIs. In the present study the rate of ultrasonographic genitourinary abnormality across all the newborns with significant hyperbilirubinemia was 7.34% (26 in 381), and the necessity of performing an abdominal ultrasonographic examination in the routine evaluation of newborns with significant Hyperbilirubinemia may be considered.
There are various reports about the types of bacterial pathogens causing UTI in newborns with both UTI and jaundice. In some studies, E.coli was the predominant pathogen [5-8, 15-17,19,20]. Whereas Klebsiella Pneumonia was in some others [4,9,10]. In the present study Gram (-) bacteria were isolated in 48 of the 66 cases, respectively, and E.coli was the most frequently isolated bacterium (36.3%).
In various studies, pyuria was reported in 11% to 85% of jaundiced newborns with UTI. In the present study the frequency of pyuria was 39.3%. This wide range of pyuria in different studies (11%-85%) suggests that it is not a very reliable parameter in the diagnosis of UTI, and urine culture should be ordered in newborns suspected to have UTI. Thus pyuria is not necessarily required in the diagnosis of UTI in newborns and the gold standard in diagnosis is urine culture positivity [12].
There have been no significant differences between the jaundiced newborns with and without UTI regarding STB levels before phototherapy in most of the studies. However pre-phototherapy STB levels in newborns with UTI were lower than that of newborns without UTI and those were higher in newborns with UTI in comparison to newborns without UTI [10]. The latter researchers reported not only pre-phototherapy but also post-phototherapy higher STB levels in jaundiced newborns with UTI in comparison to those without UTI [10]. In this study, however, postphototherapy STB levels were significantly higher in newborns with UTI when compared to newborns without UTI although pre-phototherapy STB levels were not significantly different between the two groups of newborns. Similarly, Mutlu et al reported higher rebound STB levels in jaundiced newborns with UTI when compared to those without UTI despite not having significantly different pre-phototherapy STB levels [8]. Ozcan et al reported a significantly lower phototherapy response in newborns with UTI and jaundice in comparison to newborns with jaundice only after a 24-hour phototherapy treatment. In the present study also decrease in STB levels with a 24- hour phototherapy treatment was lower in newborns with UTI and jaundice.
Conclusion
In the present study we configured on our observation that UTI decreased phototherapy response in newborns with jaundice, we detected the most ideal STB decrease as percent (Cut off value) to determine the newborns with UTI among newborns with jaundice. This cut-off value was determined as the point where the sum of sensitivity and specificity has the most ideal value and it was 47.9%. According to this value newborns who have an STB decrease of less than 47.9% after a 24-hour high-intensity phototherapy treatment may have simultaneously a UTI in addition to neonatal jaundice with a 40% probability, and those who have an STB decrease of more than 47.9% do not have a simultaneous UTI with a 90% probability. It should be remembered in mind that UTI may have a role in etiology in newborns presenting with significant hyperbilirubinemia requiring phototherapy treatment and no other investigated and demonstrated cause of neonatal indirect hyperbilirubinemia in the first 10 days of life. An STB decrease of <47.9% after a 24-hour high-intensity phototherapy treatment in newborns with significant hyperbilirubinemia should be considered an insufficient phototherapy response and further urine examinations including especially urine culture should be performed concerning the presence of UTI.
Declarations
Conflict of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Linder, N., et al. "Unexplained neonatal jaundice as an early diagnostic sign of septicemia in the newborn." Journal of Perinatology: Official Journal of the California Perinatal Association, Vol. 8, Vol. 4, 1988, pp. 325-27.
Google Scholar - Bilgen, Hulya, et al. "Urinary tract infection and hyperbilirubinemia." Turkish Journal of Pediatrics, Vol. 48, No. 1, 2006, p. 51.
Google Scholar Crossref - Nickavar, Azar, and Kambiz Sotoudeh. "Treatment and prophylaxis in pediatric urinary tract infection." International journal of preventive medicine, Vol. 2, No. 1, 2011, p. 4.
Google Scholar - Omar, Chamdine, Shadi Hamza, and Rajab Mariam. "Urinary tract infection and indirect hyperbilirubinemia in newborns." North American journal of medical sciences, Vol. 3, No. 12, 2011, p. 544.
Google Scholar Crossref - Garcia, Francisco J., and Alan L. Nager. "Jaundice as an early diagnostic sign of urinary tract infection in infancy." Pediatrics, Vol. 109, No. 5, 2002, pp. 846-51.
Google Scholar Crossref - Nader, Pashapour, Nikibahksh A. Ali, and Golmohammadlou Sariyeh. "Urinary tract infection in term neonates with prolonged Jaundice." 2007, pp. 91-94.
Google Scholar Crossref - Ghaemi, Sedigheh, Reyhaneh J. Fesharaki, and Roya Kelishadi. "Late onset jaundice and urinary tract infection in neonates." The Indian Journal of Pediatrics, Vol. 74, No. 2, 2007, pp. 139-41.
Google Scholar Crossref - Mutlu, Mehmet, Yasemin Cayır, and Yakup Aslan. "Urinary tract infections in neonates with jaundice in their first two weeks of life." World journal of pediatrics, Vol. 10, No. 2, 2014, pp. 164-67.
Google Scholar Crossref - Shahian, Mozhgan, Parisa Rashtian, and Mehdi Kalani. "Unexplained neonatal jaundice as an early diagnostic sign of urinary tract infection." International Journal of Infectious Diseases, Vol. 16, No. 7, 2012, pp. e487-e490.
Google Scholar Crossref - Ozzcan, Murat, et al. "Association between early idiopathic neonatal jaundice and urinary tract infections." Clinical Medicine Insights: Pediatrics, Vol. 11, 2017.
Google Scholar Crossref - American Academy of Pediatrics Subcommittee on Hyperbilirubinemia. "Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation." Pediatrics, Vol. 114, No. 1, 2004, pp. 297-16.
Google Scholar Crossref - Stein, Raimund, et al. "Urinary tract infections in children: EAU/ESPU guidelines." European urology, Vol. 67, No. 3, 2015, pp. 546-58.
Google Scholar Crossref - Maisels, M. Jeffrey, et al. "Hyperbilirubinemia in the newborn infant ≥ 35 weeks’ gestation: an update with clarifications." Pediatrics, Vol. 124, No. 4, 2009, pp. 1193-98.
Google Scholar Crossref - Kasap, B., A. Soylu, and S. Kavukcu. "Relation between hyperbilirubinemia and urinary tract infections in the neonatal period." Journal of Nephrology and Therapeutics, Vol. 11, 2014, p. 009.
Google Scholar - Chen, Hung-Ta, et al. "Hyperbilirubinemia with urinary tract infection in infants younger than eight weeks old." Journal of the Chinese Medical Association, Vol. 74, No. 4, 2011, pp. 159-63.
Google Scholar Crossref - Malla, T., et al. "Urinary tract infection in asymptomatic newborns with prolonged unconjugated hyperbilirubunemia: a hospital based observational study from Western Region of Nepal." Kathmandu University Medical Journal, Vol. 14, No. 53, 2016, pp. 41-46.
Google Scholar - Rashed, Y. K., A. A. Khtaband, and A. M. Alhalaby. "Hyperbilirubinemia with urinary tract infection in infants younger than eight weeks old." Journal of Pediatrics & Neonatal Care, Vol. 1, No. 6, 2014, p. 36.
Google Scholar Crossref - Lee, Hung-Chang, et al. "Urinary tract infections in infants: comparison between those with conjugated vs unconjugated hyperbilirubinaemia." Annals of tropical paediatrics, Vol. 25, No. 4, 2005, pp. 277-82.
Google Scholar Crossref - Emamghorashi, Fatemeh, et al. "Evaluation of urinary tract infection in newborns with jaundice in South of Iran." Iranian Journal of Medical Sciences, Vol. 33, No. 1, 2008, pp. 17-21.
Google Scholar - Nickavar, Azar, Nastaran Khosravi, and Mahdiye Doaei. "Early prediction of urinary tract infection in neonates with hyperbilirubinemia." Journal of Renal Injury Prevention, Vol. 4, No. 3, 2015, p. 92.
Google Scholar Crossref