Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 6
Perceived Risk of Colorectal Cancer and Barriers to Screening among Adult Saudi: A Population-Based Study
Thamer H. Alghamdi1*, Abuobaida E. E. Abukhelaif2, Naif Abdullah M.Alzahrani2 and Turki Abdullah A. Alzahrani22Pathology Department, Faculty of Medicine, Albaha University, Kingdom of Saudi Arabia
Thamer H. Alghamdi, Department of General Surgery, Faculty of Medicine, Albaha University, Kingdom of Saudi Arabia, Email: thamerhg@hotmail.com
Received: 13-May-2021 Accepted Date: Jun 22, 2021 ; Published: 30-Jun-2021, DOI: o
Abstract
Objectives: Aimed to assess the level of awareness and the perceived factors about CRC screening among adult Saudi. Methodology: A Population-based, cross-sectional study. Participants: Adult Saudi general population. Results: Among 1612 respondents 1568 eligible were included. Neither gender (p=0.51), level of education (p=0.72), income (p=0.22), nor marital status (p=0.88) were found to be statistically associated with willingness to undergo CRC screening. With regards to the awareness related to CRC incidence and risk such as “leading cause death due to CRC” “increased age is associated with increased risk of developing CRC” “both men and women are at risk for getting CRC” “People with a family history of CRC are at higher risk” and” most CRCs begin as a growth in the colon or rectum” was found to be 29.5%, 31.5%, 37.7%, 28.8%, and 22.5% respectively. 12.7% of the respondents were agreed to be routinely screened for CRC at age 45, 22.4% can identify the required frequency of CRC screening. Those who had not heard about CRC screening methods were female and were young (p=0.003); with low educational level (p<0.001). (61%) were ready to undergo CRC screening if recommended by their medical doctor while 16% of them said they would never think of doing CRC screening (p<0.0001). Regarding CRC screening options, 53% select FOBT and 39% preferred colonoscopy (p<0.0001). (57.0%) revealed that their “Fear of finding cancer “was a barrier to screening. Conclusion: Majority of our respondents shows insufficient awareness regarding CRC screening guideline and CRC screening methods.
Keywords
Colorectal cancer, Saudi, Risk factors, Screening
Introduction
Colorectal Cancer (CRC) is considered one of the prevalent, lethal, and avoidable kinds of cancer [1]. It is the highest occurring malignancy among the five major gastrointestinal cancers and ranks as the third most common cancer in both sexes worldwide, constituting about 8.2% and 8.8% of all new cancer cases and deaths respectively. According to the Surveillance, Epidemiology, and End Results (SEER) Program Cancer statistics 2020 and according to ICAR, WHO, GLOBOCON 2018, Saudi Arabia was reported to be the second among gulf countries with the highest Age- Standardized Incidence Rates (ASIRs) due to CRC in both sexes with 3,564 (14.6%) new cases [2-6]. Among Saudi males, colorectal cancer is the top most common cancer with 2,405 (19.6%) new cases for all ages, whereas it the third most common cancer among Saudi females with 1,159 (9.5%) new cases for all ages [7].
Screening and early discovery of CRC using methods and modalities like Fecal Occult Blood Test (FOBT), colonoscopy, flexible sigmoidoscopy, and CT colonography were considered as essential preventive approaches and has been confirmed to be operational in improving, thus decreasing the death and morbidity among individuals with CRC especially those aged 50-75 years, and the awareness of the screening programs among the general population is significant. In addition, it was described that the consumption of green tea can lead to the inactivation of colon cancer cells by re-activate genes in carcinogen-induced rodent models of colon cancer, which eventually led to the defeat of intestinal tumor genesis [8-13]. Several studies have looked at the awareness, perception, and screening utilization regarding CRC had been done in various countries including Saudi Arabia with resultant that there is a low level of awareness [14-29]. Furthermore, certain difficulties to carry out CRC screening have been described, such as fear of the test results, absence of awareness of symptoms, and not recommend by a doctor. Hence, our study aimed to assess the level of awareness and the perceived factors about CRC screening among the Saudi general public.
Materials and Methods
Study Design, Setting, and Population
A population-based, cross-sectional study was conducted during the period from April to 30 May 2020. Participants were randomly selected and recruited from the adult Saudi general population targeting those who were older than 18 years. Participants were voluntarily enrolled in the study. The inclusion criteria included Saudi males and females aged ≥ 18 years. Those with a current or previous diagnosis of CRC, those with any large bowel disease, and those who did not give consent were excluded from our study.
Data Collection
A convenience sampling technique was used to obtain our study population who were randomly selected. A selfadministered survey was used to collect data, the survey was designed by the principal author, and all questions were adapted from previous validated published studies and intended to collect the information from participants using Arabic language to make it easy for the respondents. Awareness among our study group regarding CRC risk factors and their perception and barriers towards screening modalities were explored. The simplicity of the questions was checked and the reliability of the instrument was tested through a pilot study of 30 adults Saudi. The purpose of the study was explained to all participants after giving consent to be included in the study.
Study Tool
The questionnaire used for data collection from our respondents was designed to include the following data.
Socio-demographics: Gender, age in years, residence, family income and educational status, and Health insurance.
Personal information relevant to CRC: CRC awareness, CRC among family and relatives.
Items related to awareness of incidence, risk factors, and importance of CRC screening and items related to awareness of barriers they perceived towards CRC screening (fecal occult blood test, flexible sigmoidoscopy, and colonoscopy). The study questionnaire followed the constructions of the Health Belief Model as a guide for validity [30].
Data Analysis
Data were analyzed using Statistical Software Package (SPSS), version 16.0. Z-test was used to compare the results among the two groups. p-value less than 0.05 will be considered as statistical significance to compare the effect of categorical data between the two groups.
Results
A total of 1612 questionnaires were filled by our respondents, 44 of them were excluded and 1568 eligible respondents were included in the study and analyzed. Our study sample constitutes 1568 Saudi adults consisted of 797 males and 771 females with the age range of 18 to 88 years (mean=55, SD=10.9). Socio-demographic characteristics of the study participants are shown in Table 1 which shows almost half (50.8%) of respondents were male, with a mean age of 41.0 ± 10.7 (Range=18-75) years, and (83.8%) of the respondents were between the ages group of 18-45years and (69.7%) were married. Most (62.7%) of the participants live in the Albaha area. Of the surveyed 80.6% had completed university or postgraduate studies and about half of participants (54.6%) reported enough income and minority (18.5%) of participants lacked health insurance? Most participants reported no family history of CRC (87.2%). The majority of the respondents had heard about CRC (81.6%). Only 3.6% reported a history of CRC in a first-degree relative. Neither gender (p=0.51), level of education (p=0.72), income (p=0.22), nor marital status (p=0.88) were found to be statistically associated with willingness to undergo CRC screening.
| Characteristics | Male (n=797; 61.7%) | Female (n=771; 38.3%) | Total (N=1568) | p-value |
|---|---|---|---|---|
| Age (mean age 41.0 ± 10.7) | ||||
| Up to 44 years | 657 (82.4%) | 634 (82.2%) | 1291 (82.3%) | 0.032 |
| 45 years and more | 140 (17.6%) | 137 (17.8%) | 277 (17.7%) | |
| Marital Status | ||||
| Married | 619 (77.7%) | 474 (61.5%) | 1093 (69.7%) | <0.0001 |
| Single | 178 (22.3%) | 297 (38.5%) | 475 (30.3 %) | |
| Educational Level | ||||
| Up to Diploma | 151 (19.0%) | 153 (19.8%) | 304 (19.4%) | 0.002 |
| University and above | 646 (81%) | 618 (80.2%) | 1264 (80.6%) | |
| Income | ||||
| Low | 169 (10.5%) | <0.0001 | ||
| Intermediate | 880 (54.6%) | |||
| High | 643 (39.9%) | |||
| Health insurance | ||||
| Yes | 1314 (81.6%) | <0.0001 | ||
| No | 298 (18.5%) | |||
| Aware of CRC | 619 (62.2%) | 380 (61.2%) | 999 (61.9%) | >0.05 |
| Family history of CRC | 136 (13.7) | 70 (11.3%) | 206 (12.8%) | <0.0001 |
Awareness of Incidence and Risk Factors of CRC
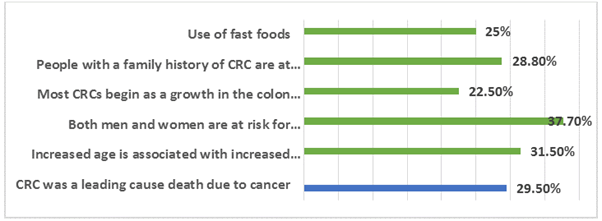
With regards to the awareness of our respondents related to CRC incidence and risk such as “CRC was a leading cause death due to cancer” “increased age is associated with increased risk of developing CRC” “use of fast foods” “both men and women are at risk for getting CRC” “People with a family history of CRC are at higher risk” and “most CRCs begin as a growth in the colon or rectum” was found to be 29.5%, 31.5%, 37.7%, 28.8%, and 22.5% respectively as shown in Figure 1. Those showing a correct answer for the above-mentioned items had significantly higher levels of educational achievement as matched to those providing a wrong answer (p<0.001, p<0.001, p=0.009, p=0.34, and p<0.001, respectively).
Awareness of the Necessity and Importance of CRC Screening
Only 12.7% of the respondents were familiar that adults should be routinely screened for colorectal cancer starting at Only 12.7% of the respondents were familiar that adults should be routinely screened for colorectal cancer starting at heard about CRC screening methods were likely to be female and were young (p=0.003); with low educational level (p<0.001).
Furthermore, most of our respondents (61%) were ready to undergo CRC screening if recommended by their medical doctor while 16% of them said they would never think of doing CRC screening (p<0.0001).
Among those who were ready to undergo CRC screening were questioned on their awareness of screening options, 53% of them select FOBT as their preferred method of screening, and 39% preferred colonoscopy (p<0.0001). And according to the reasons that might prevent respondents from having the required tests, a significant proportion (57.0%) revealed that their “Fear of finding cancer “was a barrier for screening, while the “screening procedure is not effective” or a feeling of “embarrassment if I was screened” was the least barrier revealed by our respondents (p=0.002) as shown in Table 2.
| Item | Percentage | p-value |
|---|---|---|
| Willing to have a screening test for the bowel cancer | ||
| Yes | 61.00% | p<0.0001 |
| No | 16.00% | |
| Not sure | 23.00% | |
| Preferred Colorectal Cancer screening method if willing for screening | ||
| Faecal blood test | 53.00% | p<0.0001 |
| Sigmoidoscopy and Colonoscopy | 39.00% | |
| Others | 8.00% | |
| Barriers | ||
| Fear of finding cancer (result) | 57.00% | p=0.002 |
| Embarrassment/anxiety | 8.20% | |
| High cost and lack of coverage | 8.30% | |
| Lack of knowledge about colorectal cancer guidelines | 7.30% | |
| Not recommended by my doctor | 14.20% | |
| Others | 5.00% | |
Discussion
Colorectal screening is widely available in Saudi Arabia, but there is still no population-based screening program. Setting up and implementing an effective national colorectal cancer screening program, it is vital to have a real and clear background about the depth of information among the public regarding this disorder and their choice and barriers towards the screening program. To our knowledge, there are scarce studies in this regard especially among the population of Albaha Saudi Arabia toward CRC screening, which reveals that the overall awareness was found to be relatively unsatisfactory. This is idea was constructed on the low percentage of the awareness of our respondents related to CRC incidence and risk such as “CRC was a leading cause death due to cancer” “increased age is associated with increased risk of developing CRC” “both men and women are at risk for getting CRC” “People with a family history of CRC are at higher risk” and” most CRCs begin as a growth in the colon or rectum” was found to be 29.5%, 31.5%, 37.7%, 28.8%, and 22.5% respectively. These findings were similar to previous Saudi studies conducted in different parts of Saudi such as study report from Makkah, Alahsa, and western region and other areas of Saudi Arabia which all reveal a lack in the awareness about CRC screening among the study population [25,27,31-35]. In addition, our findings are consistent with studies from surrounding countries as studies from Jordanian and East Iran and international studies in which study populations reveal inadequate and low levels of awareness about CRC and screening tests [30,36-54].
Our study reveals that only 12.7% of the respondents were familiar with that adults should be routinely screened for colorectal cancer starting at age 45 as recommended, 22.4% of them can identify the required frequency of CRC screening.
Our study reveals that most of our respondents (61%) were ready to undergo CRC screening if recommended by their medical doctor while 16% of them said they would never think of doing CRC screening. Accordingly, recommendations from medical doctors have their influence on the community concerning health plans. This puts the burden on medical doctors to make their judgment on health-related orders and discuss it with their clients putting into consideration patients’ feelings and their socio-cultural background when giving recommendations [45]. This makes medical doctors in the challenge of increasing their competence for the sake of their clients, especially on preventive healthcare.
Our study population recognized several barriers that prevent them to do CRC screening such as their “Fear of finding cancer”, while the “screening procedure is not effective” or a feeling of “embarrassment if I was screened” was the least barrier revealed by our respondents. These findings reveal the poor level of awareness and education among our study respondents. Our findings are consistent with other studies locally, nationally, and internationally [46-54].
Among those who were ready to undergo CRC screening were questioned on their awareness of screening options. 53% of them select FOBT as their preferred method of screening and 39% preferred colonoscopy. These findings were the same choices for the study population in other studies [46,49,54-59]. All revealed barriers were due to general community awareness and attitude which can be overcome and changed to better by using health promotions and awareness activities.
Conclusion
Majority of our respondents shows insufficient awareness regarding CRC screening guideline and CRC screening methods. This deficiency of information can result in a low rate of contribution in CRC screenings since adequate knowledge is important for participation. Furthermore, a lack of physician recommendation was identified as the most common barrier to CRC screening in general. Fear of finding cancer “was a barrier for screening” was the most common specific barrier to screening among our respondents. It is recommended to report the observed barriers to CRC screening recognized in our study beforehand carry out a screening program at the national level. Additional studies are necessary to discover more specific barriers among the population in the area.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
Consent
All participants provided informed, written consent before enrolment.
Funding
No external funding was sought or provided, for this study.
Ethical Approval
The study was approved by the Scientific Research & Ethics Committee (REC): Albaha University; Faculty of Medicine (REC/SUR/BU-FM/2020/0000).
Data Sharing
No additional data are available.
Acknowledgments
The authors thank students of the Albaha Faculty of Medicine for their invaluable contributions to the overall efforts in data collections. The authors also thank colleagues in the community medicine department for their ongoing support.
Contributors
Dr. Thamer wrote the paper. Dr. Abuobaida guided qualitative data collection and assisted with data analysis. Naif Abdullah M.Alzahrani and Turki Abdullah A. Alzahrani conducted all the interviews. All authors edited and critically revised the paper and approved the manuscript.
References
- Brandt, Heather M., et al. "Relationship of colorectal cancer awareness and knowledge with colorectal cancer screening." Colorectal Cancer, Vol. 1, No. 5, 2012, pp. 383-96.
- Howlader, N., et al. "SEER cancer statistics review, 1975-2017." National Cancer Institute, 2020.
- Ferlay, Jacques, et al. "Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods." International Journal of Cancer, Vol. 144, No. 8, 2019, pp. 1941-53.
- Haggar, Fatima A., and Robin P. Boushey. "Colorectal cancer epidemiology: Incidence, mortality, survival, and risk factors." Clinics in Colon and Rectal Surgery, Vol. 22, No. 4, 2009, pp. 191-97.
- Ferlay, Jacques, et al. "Global cancer observatory: Cancer today." Lyon, France: International Agency for Research on Cancer, 2018.
- Arnold, Melina, et al. "Global burden of 5 major types of gastrointestinal cancer." Gastroenterology, Vol. 159, No. 1, 2020, pp. 335-49.
- Chaudhri, Eman, et al. "The increasing trends in cases of the most common cancers in Saudi Arabia." Journal of Epidemiology and Global Health, Vol. 10, No. 4, 2020, pp. 258-62.
- World Health Organization. "Saudi Arabia; Source: Globocan 2020" International Agency for Research on Cancer. https://gco.iarc.fr/today/data/factsheets/populations/682-saudi-arabia-fact-sheets.pdf
- Almadi, Majid A., and Faisal Alghamdi. "The gap between knowledge and undergoing colorectal cancer screening using the Health Belief Model: A national survey." Saudi Journal of Gastroenterology: Official Journal of the Saudi Gastroenterology Association, Vol. 25, No. 1, 2019, pp. 27-39.
- Doubeni, Chyke A., et al. "Effectiveness of screening colonoscopy in reducing the risk of death from right and left colon cancer: A large community-based study." Gut, Vol. 67, No. 2, 2018, pp. 291-98.
- Wolf, Andrew MD, et al. "Colorectal cancer screening for average‐risk adults: 2018 guideline update from the American Cancer Society." CA: A Cancer Journal for Clinicians, Vol. 68, No. 4, 2018, pp. 250-81.
- Sung, J. J. Y., et al. "An updated Asia Pacific Consensus Recommendations on colorectal cancer screening." Gut, Vol. 64, No. 1, 2015, pp. 121-32.
- Volate, Suresh R., et al. "Epigenetic modulation of the retinoid X receptor α by green tea in the azoxymethane‐ApcMin/+ mouse model of intestinal cancer." Molecular Carcinogenesis: Published in cooperation with the University of Texas MD Anderson Cancer Center, Vol. 48, No. 10, 2009, pp. 920-33.
- Almadi, Majid A., et al. "Findings during screening colonoscopies in a Middle Eastern cohort." Saudi Journal of Gastroenterology: Official Journal of the Saudi Gastroenterology Association, Vol. 25, No. 1, 2019, pp. 20-26.
- Ramos, Maria, et al. "Knowledge and attitudes of primary healthcare patients regarding population-based screening for colorectal cancer." BMC Cancer, Vol. 11, No. 1, 2011, pp. 1-11.
- Sung, Joseph JY, et al. "Obstacles to colorectal cancer screening in Chinese: A study based on the health belief model." American Journal of Gastroenterology, Vol. 103, No. 4, 2008, pp. 974-81.
- Alsanea, Nasser, et al. "National Guidelines for Colorectal Cancer Screening in Saudi Arabia with strength of recommendations and quality of evidence: Tripartite Task Force from Saudi Society of Colon & Rectal Surgery, Saudi Gastroenterology Association and Saudi Oncology Society." Annals of Saudi Medicine, Vol. 35, No. 3, 2015, pp. 189-95.
- Berkowitz, Zahava, et al. "Beliefs, risk perceptions, and gaps in knowledge as barriers to colorectal cancer screening in older adults." Journal of the American Geriatrics Society, Vol. 56, No. 2, 2008, pp. 307-14.
- Von Wagner, Christian, et al. "Health literacy and health actions: A review and a framework from health psychology." Health Education & Behavior, Vol. 36, No. 5, 2009, pp. 860-77.
- Cooke, Richard, and David P. French. "How well do the theory of reasoned action and theory of planned behaviour predict intentions and attendance at screening programmes? A meta-analysis." Psychology and Health, Vol. 23, No. 7, 2008, pp. 745-65.
- Yeoh, Khay-Guan, et al. "The Asia-Pacific Colorectal Screening score: A validated tool that stratifies risk for colorectal advanced neoplasia in asymptomatic Asian subjects." Gut, Vol. 60, No. 9, 2011, pp. 1236-41.
- Wong, Martin CS, et al. "Targeted screening for colorectal cancer in high-risk individuals." Best Practice & Research Clinical Gastroenterology, Vol. 29, No. 6, 2015, pp. 941-51.
- Omran, Suha, and Ahmad Abedalkareem Ismail. "Knowledge and beliefs of Jordanians toward colorectal cancer screening." Cancer Nursing, Vol. 33, No. 2, 2010, pp. 141-48.
- Khayyat, Yasir Mohammed, and Ezzeldin Mostafa Ibrahim. "Public awareness of colon cancer screening among the general population: A study from the Western Region of Saudi Arabia." Qatar Medical Journal, Vol. 2014, No. 1, 2014, pp. 1-8.
- Alzahrani, IbrahimAhmed et al. "Public awareness of risk factors and screening for colorectal cancer among Saudi Arabia population, 2016." International Journal of Advanced Research, Vol. 4, No. 12, 2016, pp. 2039-54.
- Ali, Gihan Yousef, et al. "Awareness and perception of colorectal cancer risk factors among Saudis in Eastern Province, Saudi Arabia." International Journal of Healthcare Sciences, Vol. 3, No. 2, 2015, pp. 234-38.
- Othmani, M. A. A., et al. "Awareness of colorectal cancer in Tabuk City, Saudi Arabia." International Journal of Medical Research, Vol. 3, No. 1, 2017, pp. 112-15.
- Alnuwaysir, Mohammed, Nirmal Baral, and Hussain Alhadhari. "Colorectal cancer awareness and attitude among adult, Al-Dammam, Saudi Arabia." Advances in Cancer Prevention, Vol. 2016, 2016.
- Gimeno-Garcia, A. Z., et al. "Public awareness of colorectal cancer and screening in a Spanish population." Public Health, Vol. 125, No. 9, 2011, pp. 609-15.
- Glanz, Karen, Barbara K. Rimer, and Kasisomayajula Viswanath, eds. "Health behavior and health education: theory, research, and practice." John Wiley & Sons, 2008.
- Barasheed, Osamah Abdullah A., et al. "Public awareness of colorectal cancer screening in Makkah, Saudi Arabia." International Journal of Medicine in Developing Countries, Vol. 4, No. 1, 2020, pp. 001-006.
- Al Eid, Z. M., et al. "Knowledge of Colorectal Cancer Screening among men in AlAhsa, Saudi Arabia." International Journal of Scientific & Engineering Research, Vol. 8, No. 9, 2017, pp. 264-68.
- Zubaidi, Ahmad M., et al. "Public awareness of colorectal cancer in Saudi Arabia: A survey of 1070 participants in Riyadh." Saudi Journal of Gastroenterology: Official Journal of the Saudi Gastroenterology Association, Vol. 21, No. 2, 2015, pp. 78-83.
- Al Wutayd, Osama, et al. "Colorectal cancer risk factors: a study of knowledge, attitude, and practice among adults in Riyadh, Saudi Arabia." Cancer Research Journal, Vol. 3, No. 5, 2015, pp. 94-99.
- Aljumah, Abdulrahman A., and Abdulrahman M. Aljebreen. "Policy of screening for colorectal cancer in Saudi Arabia: A prospective analysis." Saudi Journal of Gastroenterology: Official Journal of the Saudi Gastroenterology Association, Vol. 23, No. 3, 2017, pp. 161-68.
- Ahmad, Muayyad M., et al. "Colorectal cancer in Jordan: Prevention and care." Global Health Promotion, Vol. 22, No. 4, 2015, pp. 39-47.
- Bidouei, Farzad, et al. "Knowledge and perception toward colorectal cancer screening in east of Iran." International Journal of Health Policy and Management, Vol. 3, No. 1, 2014, pp. 11-15.
- Salimzadeh, Hamideh, et al. "Knowledge and practice of Iranians toward colorectal cancer, and barriers to screening." International Journal of Preventive Medicine, Vol. 3, No. 1, 2012, pp. 29-35.
- Almadi, Majid A., et al. "Effect of public knowledge, attitudes, and behavior on willingness to undergo colorectal cancer screening using the health belief model." Saudi Journal of Gastroenterology: Official Journal of the Saudi Gastroenterology Association, Vol. 21, No. 2, 2015, pp. 71-77.
- Gimeno Garcia, Antonio Z. "Factors influencing colorectal cancer screening participation." Gastroenterology Research and Practice, Vol. 2012, 2012.
- Papanikolaou, Ioannis S., et al. "Awareness and attitudes of Greek medical students on colorectal cancer screening." World Journal of Gastrointestinal Endoscopy, Vol. 4, No. 11, 2012, pp. 513-17.
- Christou, Aliki, and Sandra C. Thompson. "Colorectal cancer screening knowledge, attitudes and behavioural intention among Indigenous Western Australians." BMC Public Health, Vol. 12, No. 1, 2012, pp. 1-16.
- Gede, Noemi, Diana Remenyi Kiss, and Istvan Kiss. "Colorectal cancer and screening awareness and sources of information in the Hungarian population." BMC Family Practice, Vol. 19, No. 1, 2018, pp. 1-6.
- Wilkes, Michael S., et al. "Pairing physician education with patient activation to improve shared decisions in prostate cancer screening: A cluster randomized controlled trial." The Annals of Family Medicine, Vol. 11, No. 4, 2013, pp. 324-34.
- Galal, Yasmine Samir, et al. "Colon cancer among older Saudis: Awareness of risk factors and early signs, and perceived barriers to screening." Asian Pacific Journal of Cancer Prevention, Vol. 17, No. 4, 2016, pp. 1837-46.
- Wan, Puteh Sharifa Ezat, et al. "Relationship of Knowledge, Attitude, Practice (KAP) and demographic factors with quality of life among urban colorectal cancer patients in Malaysia." Middle East Journal of Cancer, Vol. 5, No. 1, 2014, pp. 31-40.
- Ravichandran, Kandasamy, Nasser A. Al-Hamdan, and Gamal Mohamed. "Knowledge, attitude, and behavior among Saudis toward cancer preventive practice." Journal of Family and Community Medicine, Vol. 18, No. 3, 2011, pp. 135-42.
- Basch, Corey H., et al. "Fear as a barrier to asymptomatic colonoscopy screening in an urban minority population with health insurance." Journal of Community Health, Vol. 41, No. 4, 2016, pp. 818-24.
- Qumseya, Bashar J., et al. "Barriers to colorectal cancer screening in Palestine: A national study in a medically underserved population." Clinical Gastroenterology and Hepatology, Vol. 12, No. 3, 2014, pp. 463-69.
- Koo, Jenn Hian, et al. "Knowledge of, attitudes toward, and barriers to participation of colorectal cancer screening tests in the Asia-Pacific region: A multicenter study." Gastrointestinal Endoscopy, Vol. 76, No. 1, 2012, pp. 126-35.
- Gili, Margalida, et al. "Psychosocial factors associated with the adherence to a colorectal cancer screening program." Cancer Detection and Prevention, Vol. 30, No. 4, 2006, pp. 354-60.
- Alamri, Hamad M., et al. "Public awareness of colorectal cancer and perceived barriers to its screening among attendees of primary health care centers in the eastern province of Saudi Arabia." International Journal of Scientific Research, Vol. 6, No. 10, 2017, pp. 590-97.
- Wong, Reuben K., et al. "Gender differences in predictors of colorectal cancer screening uptake: A national cross sectional study based on the health belief model." BMC Public Health, Vol. 13, No. 1, 2013, pp. 1-12.
- Mosli, Mahmoud, et al. "Knowledge, attitude, and practices of primary health care physicians toward colorectal cancer screening." Saudi Journal of Gastroenterology: Official Journal of the Saudi Gastroenterology Association, Vol. 23, No. 6, 2017, pp. 330-36.
- Scheid, Dewey C., et al. "Improving colorectal cancer screening in family medicine: An Oklahoma Physicians Resource/Research Network (OKPRN) study." The Journal of the American Board of Family Medicine, Vol. 26, No. 5, 2013, pp. 498-507.
- Klabunde, Carrie N., et al. "A national survey of primary care physicians’ colorectal cancer screening recommendations and practices." Preventive Medicine, Vol. 36, No. 3, 2003, pp. 352-62.
- Rawl, S. M., et al. "Do benefits and barriers differ by stage of adoption for colorectal cancer screening?" Health Education Research, Vol. 20, No. 2, 2005, pp. 137-48.
- Yong, Sook Kwin, et al. "Colorectal cancer screening: Barriers to the Faecal Occult Blood Test (FOBT) and colonoscopy in Singapore." Proceedings of Singapore Healthcare, Vol. 25, No. 4, 2016, pp. 207-14.
- Cho, Young Ae, et al. "Genetic risk score, combined lifestyle factors and risk of colorectal cancer." Cancer Research and Treatment: Official Journal of Korean Cancer Association, Vol. 51, No. 3, 2019, pp. 1033-40.