Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 9
Paradigm Shift in Malaria Parasite Density Determination to First Principle Protocol
Iseimokumo Christopher Peletiri1,2*, Blessing Ukamaka Osita1,2, Nkechi Adaoma Nwoke1,3, Joseph Salifu David1,4 and Eugene Ifeanyichukwu Ikeh12Medical Microbiology & Parasitology Laboratories, National Hospital, Abuja, FCT, Nigeria
3Medical Laboratory Services Division, Department of Hospital Services, Federal Ministry of Health, Abuja, Nigeria
4Laboratory Department, Gwarinpa General Hospital, Life-Camp, Abuja, FCT, Nigeria
Iseimokumo Christopher Peletiri, Department of Medical Microbiology, Faculty of Clinical Sciences, College of Health Sciences, University of Jos, Nigeria, Email: kumochris@hotmail.com
Received: 18-Aug-2021 Accepted Date: Sep 23, 2021 ; Published: 30-Sep-2021, DOI: o
Abstract
Background: The need for a simple and more accurate malaria diagnosis and parasite density determination cannot be over-emphasized at such a time when there is increased infection prevalence and higher mortality rate as reported by the World Health Organization. Objective: This article highlights the simple novel approach in using the ‘first principle’ protocol on malaria parasite density determination. Methods: The protocol based on the first principle on malaria parasite quantification was used. The diameter of the field of view (dFOV, 0.178 mm) multiplied by 100 fields gives the diameter of the circle of thick blood film required. The volume of blood in the thick film is equal to the diameter of the circle of thick blood film divided by the volume of blood used (8 μL) and further divided by the magnification to give 0.002 μL. When one microlitre was divided by 0.002 μL, it gave 500 as a factor. Results: Results showed (1+) as 5 to 50 parasites/μL of blood; (2+) as 50 to 500 parasites/μL of blood; (3+) as 500 to 5000 parasites/ μL of blood; and (4+) as >5000 parasites/μL of blood. Conclusion: For us to maintain the desired quality assurance in the diagnosis of malaria, we must have to use an automatic pipette to dispense the actual volume of blood (8 μL) required to prepare a thick blood film of a circle within a specified diameter (18 mm). The use of this method has revealed that it is more accurate, quicker, reproducible, sensitive, actual result value, simple, straightforward, and scientifically verified parasitological method.
Keywords
Paradigm shift, First principle, Malaria parasite density, Quantification, Accurate, Verified method
Introduction
The need for a more accurate diagnosis of malaria cannot be over-emphasized at such a time when the current World Malaria Report showed increased prevalence and higher mortality rate. The 2020 World Malaria Report which revealed malaria as one of the most dangerous infectious diseases and caused about 229 million infections and 409,000 deaths worldwide is frightening. More worrisome about the report is the fact that Nigeria is being reported as having the highest number of global malaria cases, about 62 million cases representing 27% of global malaria cases; and accounted for the highest number of deaths, 94,000 deaths (23%) of the global malaria deaths [1]. This is certainly an emergency and so demands urgent action to stop this high number of avoidable deaths in Nigeria and the West African sub-region.
In the parasitology laboratory diagnosis of malaria, the parasite density of a positive blood film must be known because of the following reasons:
i. The clinician needs to know the severity of the infection.
ii. The clinician needs to know how the infection is responding to treatment (treatment monitoring).
iii. Parasite counts are important in Plasmodium falciparum infections, which are always considered potentially dangerous.
iv. District health officers should be aware of the severity of the cases being observed in health facilities in their area.
v. Determination of the density of infections may be required in cross-sectional and epidemiological investigations or in special studies, such as monitoring the therapeutic efficacy of antimalarial medicines [2].
Parasite density serves as one of the diagnostic criteria for severe malaria infection and its monitoring is important for the diagnosis and treatment of malaria. Parasite density is associated with patient prognosis [3-5]. Parasitaemia is one of the essential indicators of the therapeutic effects of antimalarial drugs, and daily blood smear analysis is recommended to document the decrease in parasite density until the absence of parasite on treatment day seven [4]. With the emergence of resistance to available antimalarial drugs, accurate quantitation of parasitemia is required for malaria parasite clearance determination following antimalarial treatment [6,7].
Two methods are frequently used in the examination of thick blood films and subsequent counting of malaria parasites, and include the use of the ‘First (1st) principle’ on malaria parasite quantification (count) (factor 500), and the use of 8000 White Blood Cell (WBC) count as a factor. Methods based on counting a set of WBCs before declaring a slide negative are commonly used in clinical settings and counting parasites per set number of WBCs is reported to be the most commonly used method for parasite density estimation in research studies [8]. Variations in WBC counts affect the volume of blood examined to detect parasites as well as estimates of parasite density if a simultaneously obtained true WBC count is not used [9]. Agu-Gyasi and colleagues in 2012 used an assumed white blood cell count of 10,000/ μL of blood to estimate malaria parasite density. As of 1980, the WBC factor used then was 100 [10,11]. This clearly shows an inconsistent use of the WBC factor.
A research article by Greenwood and Armstrong in 1991 titled “Comparison of two simple methods for determining malaria parasite density” was published by the Transactions of the Royal Society of Tropical Medicine and Hygiene, Volume 85: 186-188 [12]. The two simple methods compared were:
i. The number of parasites present per white blood cell was counted and this figure was multiplied by 8000 (an average white blood cell count per microlitre) to give the parasite density. This is the method contained in Basic Malaria Microscopy, Part 1, Learner’s Guide (2nd edition) published by WHO, 2010 and so used worldwide till date. Currently, parasitemia is still been determined by counting parasites per 200 or 500 WBCs and a factor of 8000 [2,13]. According to WHO the factor (8000) is arbitrarily used for the calculation to obtain parasite count per microlitre of blood, though with wide variations among individuals [2]. The normal range of leukocytes (WBC count) per microlitre of blood is between 4000 to 11000 in healthy humans. So, why the use of 8000 to obtain parasite count per microlitre of blood? Therefore, the use of an arbitrary number (8000) in the calculation to obtain final values at per microlitre of blood falls short of the required quality assurance in malaria diagnosis.
ii. In the second method, the number of parasites present per high power microscope field (100× objective) was determined and the parasite density was calculated from this value and the assumed volume of blood present in one high power field.
From their findings, they reported that the latter method (ii) proved to be more accurate than that based on the determination of the parasite/white blood cell ratio. Based on their findings, they proposed 500 as a factor, calculating that (5-8) μL was the volume of blood required to make a satisfactory thick film and that the volume of blood in one thick film (100× objective) of a well-prepared thick film was about 0.002 μL. We have investigated and verified their proposal and so affirm the volume of blood in one thick film as 0.002 μL.
Therefore, this article intends to highlight the simple novel approach in using the “first (1st) principle protocol” on malaria parasite density determination.
Materials and Methods
Formulation of the First (1st) Principle
The first (1st) principle on malaria parasite quantification states that “When a measured volume of blood (e.g., 8 μL) is spread within a defined diameter of the circle (thick film) (e.g., 18 mm) under a magnification of 1000 (100× objective), the volume of blood in one thick film field (0.002 μL) is obtained; and with the value of several parasites seen per 100 fields or average number per each field which when multiplied by a factor (500) will give malaria parasites quantification (count) per microlitre of blood” [14]. We simply modified the proposal by Greenwood and Armstrong to deduce the statement of this first principle [12].
Malaria parasites are counted by estimating the parasite numbers/μL of blood from the thick film. Between 10-100 fields (depending on the parasitemia) are examined to determine the average number of trophozoites per thick film field. Ten fields are sufficient when the parasite density is high. For malaria quantification, the factor of 500 was proposed by Greenwood and Armstrong [12]. They calculated that 5 μL-8 μL was the volume of blood required to make a satisfactory thick film and that the volume of blood in one thick film field (100× objective) of a well-prepared thick film is about 0.002 μL.
Verification/Application of 1st Principle
To verify their proposal and arrival of 0.002 μL as stated, we investigated, verified, and affirmed as thus:
i. Calculation of the diameter of the circle of thick blood film required will be equal to the diameter of Field of View (dFOV, 0.178 mm) multiplied by 100 fields [15,16].
Therefore, dFOV multiplied by 100 fields
=0.178 mm × 100=17.8 mm=18 mm
ii. Estimation of volume of blood in one thick film field (100× objective)
The volume of blood in one thick film (100× objective) of a well-prepared thick film will be equal to the diameter of the circle of thick blood film divided by the volume of blood used and further divided by the magnification.
Diameter of the circle of thick blood film=18 mm
The volume of blood used=8 μL
Magnification of 100 × objective=1000
Formula: Diameter of the circle of thick blood film/volume of blood used/magnification
= 18/8/1000=2.25/1000=0.00225=0.002 μL
With this outcome, we can create a table (Table 1) for the required diameter of the circle of thick blood film prepared from other volumes of blood used (e.g., 5 μL, 6 μL, and 7 μL).
| The volume of blood (µL) a |
Diameter of thick blood film (mm) b |
Value of (b/a) c |
The volume of blood in one thick film field=Value (c)/Magnification of 100 × objective (1000)=µL |
|---|---|---|---|
| 5 | 12 | 12/5=2.4 | 2.4/1000=0.002 |
| 6 | 14 | 14/6=2.33 | 2.33/1000=0.002 |
| 7 | 16 | 16/7=2.28 | 2.28/1000=0.002 |
| 8 | 18 | 18/8=2.25 | 2.25/1000=0.002 |
Malaria parasites quantification (counts) are measured as per microlitre (μL) of blood. Therefore, to convert 0.002 μL to one (1) microlitre (μL) is simply by dividing 1 μL with 0.002 μL, which gives 500. Therefore, the number of parasites seen and counted per 100 thick films or the average number per thick film field multiplied by 500 gives the number of parasites/μL of blood. This method, Greenwood and Armstrong found to be more accurate and quicker than counting the parasites against white blood cells in a thick film using the WHO method as was used by Molineaux and Gramiccia [11,12].
Preparation of Thick and Thin Blood Films
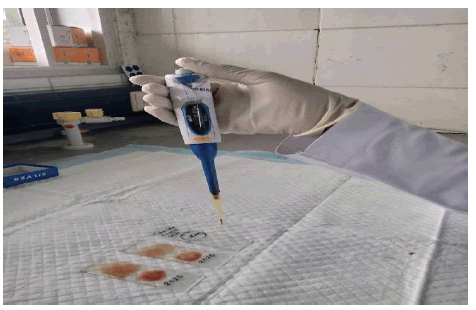
i. Using an automatic pipette, transfer 8 μL of blood to a clean microscope glass slide and prepare a thick film of a circle with 18 mm diameter
ii. On the same slide, prepare a good thin blood film as shown in Figure 1
iii. Allow airing to dry for about 30 minutes at RT or about 40℃ for less than 30 minutes
iv. When dried, fix thin-film briefly with methanol
v. Stain prepared slides with 3% Giemsa stain for 30-45 minutes (for urgent cases, use 10% Giemsa stain for 10 minutes)
vi. Wash slides carefully and allows drying properly
vii. Examine slides with 100 × objective
Results
Reporting of Results/Parasite Quantification
Counting of malaria parasites with Giemsa stained thick blood film [17].
For designation of the relative count on a thick film, a simple code from one to four plus (1+ to 4+) or the plus sign scheme is used to report parasite numbers:
• (1+)=1-10 parasites per 100 thick film fields
(take note of the number of parasites counted/100 fields)
Therefore; (1/100 to 10/100)
=(0.01 to 0.1) × 500
=5 to 50 parasites/μL of blood
• (2+)=11-100 parasites per 100 thick film fields
(take note of the number of parasites counted/100 fields)
Therefore; (10/100 to 100/100)
=(0.1 to 1) × 500
=50 to 500 parasites/μL of blood
• (3+)=1-10 parasites per thick film field
(take note of average number of parasites counted/each field)
Therefore; (1 to 10) × 500
=500 to 5000 parasites/μL of blood
• (4+)= >10 parasites per one thick film field
(take note of average number of parasites counted/each field)
Therefore; (>10) × 500
= >5000 parasites/μL of blood
There is the need to update our reporting format to meet the requirement for personalized medical care (individual patient care) as shown in Table 2.
| Laboratory No. | Patient Hospital No. | Patient’s Name | Microscopy Result | Number of parasites seen per 100 fields or average number per field | The value obtained by dividing by 100 or per field | Multiply by a factor (500) | Parasite Count/µL of blood |
|---|---|---|---|---|---|---|---|
| 1 | 10101 | Tomorrow Good | Negative | 0 | 0 | 500 | 0 |
| 2 | 61124 | Brilliant Girl | Positive 1+ | 1/100 fields | 0.01 | 500 | 5 |
| 3 | 12033 | Truth Saves | Positive 1+ | 6/100 fields | 0.06 | 500 | 30 |
| 4 | 100230 | Itis well | Positive 1+ | 9/100 fields | 0.09 | 500 | 45 |
| 5 | 23456 | Baby Boy | Positive 2+ | 12/100 fields | 0.12 | 500 | 60 |
| 6 | 14365 | Baby Girl | Positive 2+ | 50/100 fields | 0.5 | 500 | 250 |
| 7 | 45615 | Good Boy | Positive 2+ | 90/100 fields | 0.9 | 500 | 450 |
| 8 | 20202 | Yesterday Forget | Positive 3+ | 2/field | 2 | 500 | 1,000 |
| 9 | 22231 | Morning Bay | Positive 3+ | 4/field | 4 | 500 | 2,000 |
| 10 | 24113 | Evening Stone | Positive 3+ | 9/field | 9 | 500 | 4,500 |
| 11 | 11122 | Village Boy | Positive 4+ | 13/field | 13 | 500 | 6,500 |
| 12 | 26781 | Native Girl | Positive 4+ | 25/field | 25 | 500 | 12,500 |
| 13 | 44129 | Last Born | Positive 4+ | 60/field | 60 | 500 | 30,000 |
Our reporting system for malaria diagnosis should be updated to meet personalized patient care. For example:
Malaria Parasite (MP) Result for Patient 1
Thick and thin films: Trophozoites of Plasmodium falciparum 3+ seen
Malaria Parasites quantification (count): 4,500 parasites/μL of blood
Malaria Parasite (MP) Result for patient 2
Thick and thin films: Trophozoites of Plasmodium falciparum 3+ seen
Malaria Parasites quantification (count): 2,000 parasites/μL of blood
Malaria Parasite (MP) Result for Patient 3
Thick and thin films: Trophozoites of Plasmodium falciparum 3+ seen
Malaria Parasites quantification (count): 1,000 parasites/μL of blood
Counting Malaria Parasites Against Wbcs in the Thick Blood Film
The number of parasites is counted about a standard number of leukocytes in the thick film. The number of leukocytes used (8000) is arbitrary [2]. In addition to the materials already being used, you will need:
i. Two tally counters (one to count parasites and the other to count leukocytes)
ii. a simple electronic calculator.
The method:
• Count the number of parasites seen on one tally counter and the number of white blood cells on the other, oil immersion field by field
• The number of parasites and white blood cells counted depends on how numerous the parasites are and the time you have available to make the count
• When counting is completed (either against 200 or 500 WBCs), the number of parasites relative to the number of leukocytes is calculated and expressed as ‘parasites per microlitre of blood’ from the simple mathematical formula
Number of parasites counted × 8000/Number of leukocytes=parasites per microlitre
For example, see likely values obtained from patients’ samples;
Patient 1:
Number of parasites counted=105
Number of leukocytes counted=200
Factor=8000
So, using the formula above, we have
105 × 8000/200=4,200 parasites/μL of blood
Patient 2:
Number of parasites counted=87
Number of leukocytes counted=500
Factor=8000
So, using the formula above, we have
87 × 8000/500=1,392 parasites/μL of blood
Discussion
According to the Advanced Learner’s Dictionary, the word ‘arbitrary’ means “not seeming to be based on a reason, system or plan and sometimes seeming unfair”. The New International Webster’s Comprehensive Dictionary of the English Language, Deluxe Encyclopedic Edition defined ‘arbitrary’ as that action based on mere opinion or prejudice or capricious. Therefore, the arbitrary use of the factor (8000) in the current widely used malaria parasite density determination worldwide being a mere opinion and not based on an acceptable scientific reason should be discontinued and replaced with the more accurate method using the first principle as stated above. Malaria parasite density determination based on the first principle method is a more accurate and scientifically verified simple methodology that would enhance straightforward diagnosis of malaria in the West African sub-region, the most affected region of malaria infection worldwide.
While comparing the two methods, O’Meara, et al. reported overall parasite densities that were significantly lower and the discrepancy between readers was higher when using the grid method compared to the WBC method [9]. In their recommendations, they stated that the significant differences measured by the grid method and the WBC method need to be evaluated. As was earlier proposed by Greenwood and Armstrong, we have evaluated and verified the first principle protocol as the surer way to the diagnosis and parasite density determination of malaria parasite infection [12]. Being a novel methodology, as against the World Health Organization propagated method of counting malaria parasites against 200 or 500 WBCs and using 8000 WBC counts as a factor, related works in support to the use of the first principle protocol are very scarce in the literature. Therefore, our submission on this matter (first principle protocol on malaria parasite density determination) is baseline data for reference.
For us to maintain quality assurance/control in the parasitology laboratory diagnosis of malaria, we must have to use an automatic pipette to dispense the required volume of blood (e.g. 8 μL) to prepare a thick blood film of a circle within a specified diameter (e.g.18 mm). The proposal by Greenwood and Armstrong in 1991 that the volume of blood in a well-prepared thick film as 0.002 μL has been verified [12]. The factor of 500 as proposed by Greenwood and Armstrong to obtain parasite count per microlitre of blood was also confirmed [12]. The report by Greenwood and Armstrong that they found the use of counting malaria parasites with a measured volume of blood spread within a defined diameter to be more accurate and quicker than counting the parasites against white blood cells is very true [12]. We do not need the use of WBC count in the diagnosis and estimation of malaria parasite density (quantification) when quality assurance is of the essence.
The use of this verified method (First (1st) principle) has revealed that it is an accurate, quicker, reproducible, sensitive, actual result value, simple, shorter (reduced)-turnaround time, straightforward, and scientifically verified parasitological method [14]. The use of counting malaria parasites against WBCs is less accurate, result value approximated, tedious, cumbersome, clumsy, and a dangerous method as it increases the time of exposure to microscope light rays with attendant long time negative side effects to the eyes of the microscopist.
As stated in the Malaria Microscopy Quality Assurance (QA) Manual, it is necessary to ensure that healthcare professionals and patients have full confidence in the laboratory result, and the diagnostic results benefit the patient and community. Hospitals and health centers require expert microscopy for the management of malaria cases; it is the gold standard in endemic countries for identifying mixed infections, treatment failures, and quantifying parasite density [18]. While appreciating technological advances in the area of automation in malaria parasite diagnosis, the use of Giemsa stained thick and thin blood films would remain the gold standard in resource-limited settings for a long while. The future perspectives therefore should be focused on training and re-training of laboratory professionals in the accurate diagnosis of malaria leveraging on this simple but more accurate protocol of using the ‘first principle protocol’. There should be sincerity of purpose on the part of all stakeholders in this business of fighting to eliminate or at least reduce the malaria burden globally.
Finally, owing to the novelty of this research work, related references in support of this novel methodology are rare.
Recommendations and Conclusion
We recommend as follows:
1. The paradigm shift in malaria parasite diagnosis and quantification method from the less accurate, result value approximated, tedious, time-consuming hematological method (counting malaria parasites against WBCs and multiplied by a factor of 8000 WBC) to a more accurate, quicker, reproducible, sensitive, actual result value, simple, short (reduced)-turnaround time, straightforward, and scientifically verified parasitological method of using a measured volume of blood spread within a defined diameter of the circle.
2. The World Health Organization (WHO) in line with one of her functions “to establish and stimulate the establishment of international standards for biological, pharmaceutical, and similar products and to standardize diagnostic procedures” should without further delay propagate this verified parasitological method (First principle protocol) in the evaluation of malaria parasite quantification worldwide.
3. The use by WHO in the training and certification of various levels of competence in malaria parasite microscopy with the less accurate and tedious hematological method should be discontinued.
4. Henceforth, the WHO should commence the usage of the scientifically verified parasitological method (First principle protocol) both for training and certification purposes of microscopists on malaria quantification.
5. The call by WHO in 2010 that the ‘plus system’ in the reporting of malaria result was an old method, which was adjudged simple, but far less accurate for establishing parasite density in thick blood film because of its perceived unreliability and to be replaced by the hematological method of counting malaria parasites against WBCs is far less accurate, time-consuming and tedious, hence the recommendation by WHO should be urgently reviewed for possible upgrade to the use of the ‘first principle protocol’.
6. Functional medical laboratories should be established in all the health centers located in our rural areas to be manned by qualified Medical Laboratory Scientists and Medical Laboratory Technicians alike. As there are Government employed Medical Officers, Pharmacists/Pharmacy Technicians as well as Nurses at the Primary Health care facilities, qualified Medical Laboratory Scientists and Medical Laboratory Technicians should equally be employed to render service for which they are being trained; to avert unqualified personnel from running malaria tests amongst others.
7. Finally, we strongly recommend that henceforth, malaria parasite diagnosis and quantification test results should be done solely based on the ‘first principle protocol’ as stated in these lessons from the field.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
References
- World Health Organization. "World malaria report 2020: 20 years of global progress and challenges." 2020.
- World Health Organization. "Basic malaria microscopy: Part I. Learner's guide." World Health Organization, 2nd ed., 2010.
- Gonçalves, Bronner P., et al. "Parasite burden and severity of malaria in Tanzanian children." New England Journal of Medicine, Vol. 370, No. 19, 2014, pp. 1799-808.
- Griffith, Kevin S., et al. "Treatment of malaria in the United States: A systematic review." JAMA, Vol. 297, No. 20, 2007, pp. 2264-77.
- World Health Organization. "Management of severe malaria: A practical handbook, 3rd ed." WHO: Geneva, Switzerland, 2012.
- Ashley, Elizabeth A., et al. "Spread of artemisinin resistance in Plasmodium falciparum malaria." New England Journal of Medicine, Vol. 371, No. 5, 2014, pp. 411-23.
- White, Nicholas J. "Malaria parasite clearance." Malaria Journal, Vol. 16, No. 1, 2017, pp. 1-14.
- Dhorda, Mehul, et al. "Towards harmonization of microscopy methods for malaria clinical research studies." Malaria Journal, Vol. 19, No. 1, 2020, pp. 1-14.
- O’Meara, Wendy Prudhomme, et al. "Systematic comparison of two methods to measure parasite density from malaria blood smears." Parasitology Research, Vol. 99, No. 4, 2006, pp. 500-04.
- Adu-Gyasi, Dennis, et al. "Estimating malaria parasite density: Assumed white blood cell count of 10,000/μl of blood is appropriate measure in Central Ghana." Malaria Journal, Vol. 11, No. 1, 2012, pp. 1-6.
- Molineaux, Louis, Gabriele Gramiccia, and World Health Organization. "The Garki project: Research on the epidemiology and control of malaria in the Sudan savanna of West Africa." World Health Organization, 1980.
- Greenwood, B. M., and J. R. M. Armstrong. "Comparison of two simple methods for determining malaria parasite density." Transactions of the Royal Society of Tropical Medicine and Hygiene, Vol. 85, No. 2, 1991, pp. 186-88.
- Yoon, Jung, et al. "An automated microscopic malaria parasite detection system using digital image analysis." Diagnostics, Vol. 11, No. 3, 2021, pp. 527-39.
- Peletiri IC. "Malaria diagnosis: The differential applicability of microscopy and malaria antigen test (Rapid Diagnostic Test)" 3rd Annual Scientific Conference organized by the Association of Medical Laboratory Scientists of Nigeria, 2021.
- Armstrong WP. "Diameter of the field of view. In: Physical Properties and Structure of Cells." 2012.
- Cheebrough, Monica. "District laboratory practice in tropical countries, part 2." 2000, pp. 207-12.
- Peletiri, I. C., and N. K. O. Ibecheozor. "Malaria status amongst some patients at an Elite Hospital in Abuja, Nigeria." International Journal of Malaria Research and Reviews, Vol. 1, No. 2, 2013, pp. 12-21.
- World Health Organization. "Malaria microscopy quality assurance manual-version 2." World Health Organization, 2016.
References
- World Health Organization. "World malaria report 2020: 20 years of global progress and challenges." 2020.
- World Health Organization. "Basic malaria microscopy: Part I. Learner's guide." World Health Organization, 2nd ed., 2010.
- Gonçalves, Bronner P., et al. "Parasite burden and severity of malaria in Tanzanian children." New England Journal of Medicine, Vol. 370, No. 19, 2014, pp. 1799-808.
- Griffith, Kevin S., et al. "Treatment of malaria in the United States: A systematic review." JAMA, Vol. 297, No. 20, 2007, pp. 2264-77.
- World Health Organization. "Management of severe malaria: A practical handbook, 3rd ed." WHO: Geneva, Switzerland, 2012.
- Ashley, Elizabeth A., et al. "Spread of artemisinin resistance in Plasmodium falciparum malaria." New England Journal of Medicine, Vol. 371, No. 5, 2014, pp. 411-23.
- White, Nicholas J. "Malaria parasite clearance." Malaria Journal, Vol. 16, No. 1, 2017, pp. 1-14.
- Dhorda, Mehul, et al. "Towards harmonization of microscopy methods for malaria clinical research studies." Malaria Journal, Vol. 19, No. 1, 2020, pp. 1-14.
- O’Meara, Wendy Prudhomme, et al. "Systematic comparison of two methods to measure parasite density from malaria blood smears." Parasitology Research, Vol. 99, No. 4, 2006, pp. 500-04.
- Adu-Gyasi, Dennis, et al. "Estimating malaria parasite density: Assumed white blood cell count of 10,000/μl of blood is appropriate measure in Central Ghana." Malaria Journal, Vol. 11, No. 1, 2012, pp. 1-6.
- Molineaux, Louis, Gabriele Gramiccia, and World Health Organization. "The Garki project: Research on the epidemiology and control of malaria in the Sudan savanna of West Africa." World Health Organization, 1980.
- Greenwood, B. M., and J. R. M. Armstrong. "Comparison of two simple methods for determining malaria parasite density." Transactions of the Royal Society of Tropical Medicine and Hygiene, Vol. 85, No. 2, 1991, pp. 186-88.
- Yoon, Jung, et al. "An automated microscopic malaria parasite detection system using digital image analysis." Diagnostics, Vol. 11, No. 3, 2021, pp. 527-39.
- Peletiri IC. "Malaria diagnosis: The differential applicability of microscopy and malaria antigen test (Rapid Diagnostic Test)" 3rd Annual Scientific Conference organized by the Association of Medical Laboratory Scientists of Nigeria, 2021.
- Armstrong WP. "Diameter of the field of view. In: Physical Properties and Structure of Cells." 2012.
- Cheebrough, Monica. "District laboratory practice in tropical countries, part 2." 2000, pp. 207-12.
- Peletiri, I. C., and N. K. O. Ibecheozor. "Malaria status amongst some patients at an Elite Hospital in Abuja, Nigeria." International Journal of Malaria Research and Reviews, Vol. 1, No. 2, 2013, pp. 12-21.
- World Health Organization. "Malaria microscopy quality assurance manual-version 2." World Health Organization, 2016.