Research Article - International Journal of Medical Research & Health Sciences ( 2022) Volume 11, Issue 12
Ocular Manifestation in Mucormycosis Patients in Post COVID Patients in Western Rajasthan
Sujata Kumari1*, Arvind Chauhan1 and Narendra Kumar22Department of Skin and Venereal Diseases (VD), S.M.S. Medical College, Jaipur, Rajasthan, India
Sujata Kumari, Department of Ophthalmology, Dr. S.N. Medical College, Jodhpur, Rajasthan, India, Email: sujatachoudhary486@gmail.com
Received: 12-Jul-2022, Manuscript No. IJMRHS-22-69139; Editor assigned: 14-Jul-2022, Pre QC No. IJMRHS-22-69139 (PQ); Reviewed: 28-Jul-2022, QC No. IJMRHS-22-69139; Revised: 12-Oct-2022, Manuscript No. IJMRHS-22-69139 (R); Published: 21-Oct-2022
Abstract
Aim: There are increasing cases of rhino-orbital mucormycosis in patients who found positive for corona virus (COVID-19). Diabetes Mellitus (DM) is main risk factor for both COVID-19 and mucormycosis. We aim to find out ocular manifestation of mucormycosis in post COVID patients.
Material and methods: we conducted a study in 110 patients at Dr. S.N. medical college, Jodhpur, Rajasthan. We selected all the details of case reports/series of patients with mucormycosis and COVID-19 who came to OPD during COVID pandemic with chief complain of upper respiratory tract infection like fever, cold, cough. Then, we analyzed the patients according to associated co-morbidities, location of mucormycosis, use of steroids and ocular complaints of mucormycosis.
Results: we selected 110 patients for the study who found positive for COVID-19 at any time during or before the study. In this study 82 patients (74.54%) were males and 28 were females, both in patients who were active for COVID-19 64 patients (58%) and recovered 46 patients (42%). Pre-existing DM was present in 81 patients (73.63%); Diabetic Ketoacidosis (DKA) was present in 15 patients (13.63%). History of corticosteroid uses for COVID-19 treatment was present in 78 patients (70.90%); history of remdesivir for COVID-19 treatment was present in 12 patients (29.10%). History of no steroid was present in 20 patients. Most common sign found is ptosis in 60 patients (54.54%), total ophthalmoplagia in 58 patients (52.72%), proptosis in 58 patients (52.72%), periocular edema in 57 patients (51.81%), periocular tenderness in 57 patients (51.81%), decreased vision noted in 15 patients (13.63%), in which complete loss of vision in 10 patients (9.09%), central retinal artery occlusion is found in 10 patients (9.09%), disc pallor is found in 10 patients (9.09%).
Conclusion: Diabetes is important risk factor both COVID-19 and mucormyosis.
Keywords
COVID-19, Mucormycosis, Diabetes, Mucormyosis, Diabetic ketoacidosis
Introduction
COVID-19 infection began in India around March 2021 and rapidly spread; reaching a peak around may 2021 [1]. COVID-19 associated Rhino-Orbital Cerebral Mucormycosis (CA-ROCM) cases recognized during the first wave of COVID-19. Whose patients reported mucormycosis, having COVID-19 positive history in mostly patients? [2].
CA-ROCM has a worldwide distribution. In this study we recruit all 110 patients from Dr. S.N. medical college attached COVID-19 dedicated hospital Mathura Das Mathur Hospital, Jodhpur.
The primary reason which facilitates the growth of mucorales spores in people with COVID-19 is an ideal environment of low oxygen (hypoxia), high glucose (diabetes, new onset hyperglycemia, steroid induced hyperglycemia), acidic medium (metabolic acidosis, Diabetic Ketoacidosis (DKA), increased ferritin level in blood and decreased phagocytic activity of White Blood Cells (WBC) due to immunosuppression (SARS-CoV-2 mediated, steroid mediated or background co-morbidities) with several other risk factor including prolonged hospitalization with or without mechanical ventilators.
Mucormycosis is an angioinvasive disease caused by mold fungi of genus Rhizopus, Mucor, Rhizomucor, Absidia and Cunninghamella of order mucorales, class zygomycetes [3]. The Rhizopus oryzae is most common type and responsible for about 60% cases of mucormycosis cases in humans and about 90% of Rhino Orbital Cerebral (ROCM) form [4].
During the COVID-19 pandemic where corticosteroid used as a treatment of COVID-19 there cases of mucormycosis increased because of decreased immunity. Intracranial involvement of mucormycosis increased the fatality rates.
A preliminary study was designed to document clinical along with microbiological, pathological, radiological features and possible risk factor triggering the COVID-19 associated ROCM and to formulate guidelines for prevention of the disease.
Materials and Methods
A cross sectional study conducted at Dr. S.N. medical college, Jodhpur, Rajasthan attached hospital Mathura Das Mathur Hospital. We selected 110 patients who are admitted or discharged and found positive for COVID-19 by RTPCR at any time during or before the study. Detailed history of patients was obtained by hospital data and files. Written and informed consent was taken from all the patients. A detailed data collection sheet was formulated for the information collection from the hospital records based on demographic profile, vaccination status, date of COVID-19 diagnosis, date of onset of symptoms of CA-ROCM, clinical features of ROCM, associated comorbidities, glycosylated Hemoglobin (HbA1c) status, treatment received for COVID-19, nasal endoscopic findings, microbiological, pathological, radiological details, medical treatment initiated for ROCM, surgical planning or execution.
Details of recent or past COVID-19 symptoms and findings were collected from the available documents of patients in hospital records. The diagnosis of COVID-19 was based on positive Reverse Transcriptase Polymerase Chain Reaction (RTPCR) reports or rapid antigen report of naso-oropharyngeal swab. Patients recovered from COVID-19 infection three month ago and currently RTPCR negative for SARS-CoV-2 were termed as recent COVID-19 the time limit of three months was taken as per widely accepted definition of post-acute COVID-19 syndrome [5]. Active COVID-19 cases were defined who were found positive by RTPCR during the study. Severity of COVID-19 was based on the prescribed Indian government guidelines [6]. Mild cases of COVID-19 were managed by home isolation with symptomatic treatment. Patients with moderate to severe were hospitalized and managed with oxygen therapy, anticoagulation, awake positioning, Intravenous (IV) methylprednisolone 0.5 to 1 mg/kg or IV dexamethasone 0.5-2 mg/kg according to severity of COVID-19. If the symptoms were improved then it switched to oral route. Antibiotics were prescribed only if the suspicion of bacterial infection.
Statistical analysis: Collected data was fed into Microsoft excel sheet and statistical analysis was done using IBM SPSS 22 software.
Results
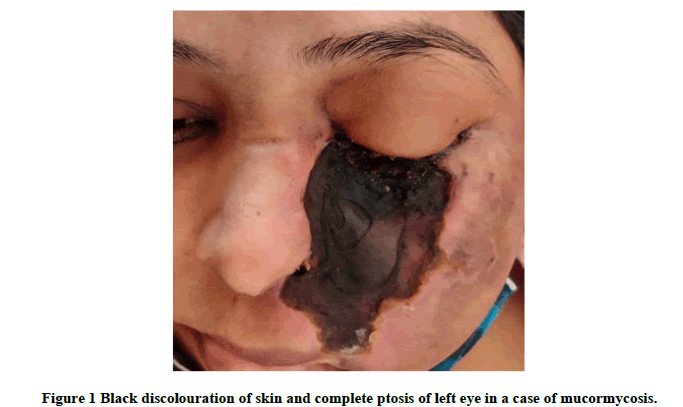
We included 110 patients of mucormycosis during COVID-19 pandemic. The demographic profile and risk factor of Figure 1 ROCM are given in Table 1. The mean age of patients was 50 years, ranging from 30-85 years. In study 82 patients were male and 28 were females.
| Risk factor | Number of cases | Percentage (n=110) |
|---|---|---|
| Age | 30-85 years | - |
| Gender | ||
| Male | 82 | 74.54% |
| Female | 28 | 25.45% |
| Covid vaccination status | ||
| No dose | 90 | 81.81% |
| First dose | 20 | 18.18% |
| Severity of COVID infection | ||
| Mild | 40 | 36.36% |
| Moderate | 50 | 45.45% |
| Severe | 20 | 18.18% |
| Oxygen status | ||
| Given | 72 | 65.45% |
| Not given | 38 | 34.54% |
| Steroid history | 78 | 70.90% |
| No | 20 | 18.18% |
| Oral | 20 | 18.18% |
| IV | 38 | 34.54% |
| Remdesivir given | 12 | 10.90% |
| Diabetes history | ||
| Pre-existing | 81 | 73.63% |
| DKA | 15 | 13.63% |
| Duration of diabetes | >5 years | |
| HbA1c | 6.9 | |
| Other co-morbidities | ||
| Hypertension | 20 | 18.18% |
| Coronary artery disease | 10 | 9.09% |
| Thyroid disease | 6 | 5.45% |
| Chronic kidney disease | 3 | 2.72% |
Table 1: Demographic picture and risk factor of ROCM.
In 110 cases 64 patients (58%) has now active COVID-19 and 46 patients (42%) has recovered from COVID-19. From 110 cases, 81 patients (73.63%) has pre-existing diabetes mellitus. 15 patients (13.63%) has Diabetic Ketoacidosis (DKA). 78 patients (70.90%) has history of corticosteroid given as a treatment of COVID-19. 12 patients (29.10%) given remdesivir as a treatment of COVID-19. 91 patients (82.72%) were nose and sinus involvement, rhino-orbital involvement in 80 patients (72.72%).
Facial pain was the commonest and earliest symptom of ROCM patients which is present in 40 patients (36.36%). Then facial swelling in 23 patients (20.90%), decreased vision noted in 15 cases (13.63%), black stained nasal discharge in 10 patients (9.09%), ptosis noted in 5 patients (4.54%) (Table 2).
| First symptom of ROCM | Number of cases | Percentage (n=110) |
|---|---|---|
| Facial pain | 40 | 36.36% |
| Facial swelling | 23 | 20.90% |
| Decreased vision | 15 | 13.63% |
| Black stained nasal discharge | 10 | 9.09% |
| Diplopia | 5 | 4.54% |
| Facial numbness | 2 | 1.81% |
| Ptosis | 5 | 4.54% |
Table 2: Clinical features of ROCM patients.
Most common sign found is ptosis in 60 patients (54.54%), total ophthalmoplagia in 58 patients (52.72%), proptosis in 58 patients (52.72%), periocular edema in 57 patients (51.81%), periocular tenderness in 57 patients (51.81%), decreased vision noted in 15 patients (13.63%), in which complete loss of vision in 10 patients (9.09%), central retinal artery occlusion is found in 10 patients (9.09%), disc pallor is found in 10 patients (9.09%) (Table 3).
| Sign and Symptoms | Number of cases | Percentage (n=110) |
|---|---|---|
| Ptosis | 60 | 54.54% |
| Total opthalmoplgia | 58 | 52.72% |
| Proptosis | 58 | 52.72% |
| Periocular edema | 57 | 51.81% |
| Periocular tenderness | 57 | 51.81% |
| Decreased vision | 15 | 13.63% |
| Complete loss of vision | 10 | 9.09% |
| Cental retinal artery occlusion | 10 | 9.09% |
| Disc pallor | 10 | 9.09% |
| Disc edema | 9 | 8.18% |
| Eyelids black discolouration | 10 | 9.09% |
| Facial palsy | 5 | 4.54% |
| Exenteration done | 10 | 9.09% |
Table 3: Ocular sign and symptoms related to Mucormycosis at presentation.
All the patients were treated with Amphotericin B liposomal IV 5 mg/kg/day. In 10 patients Functional Endoscopic Sinus Surgery (FESS) is done combined with maxillectomy and orbital exenteration. Transcutaneous retro bulbar amphotericin B injection (1 ml of 3.5mg/ml) daily for 3 days was given in about 25 eyes with stage 3 ROCM patients.
Discussion
Mucormycosis is known to be associated with malignant hematological disease, severe neutropenia, uncontrolled diabetic mellitus, prolonged use of steroid, major trauma, IV drug abuse, iron overload. It has been noted that cases of mucormycosis increases in diabetic mellitus patients, use of immunosuppressive therapy, ICU stay for long time, use of mechanical ventilators. In another study the median age of ROCM patients noted 44.5, 51.9, 52 years with male predilection of 60%, 71%, 66% respectively [7,8].
Airway epithelial damage of COVID-19 due to oxygen delivery devices, prolonged use of humidifiers without cleaning, use of industrial oxygen, multiple swab tests have been noted to facilitates the growth of fungi in lung tissues [9-11].
So that, the mutant COVID-19 variant in presence of glycemic dysregulation predisposes the development of ROCM.
Conclusion
Introduction of red flag sign of ROCM in the national guidelines for COVID management facilitates early diagnosis so that can prevent the mortality. Diabetes is important risk factor both both COVID-19 and mucormyosis.
References
- Menon S. India COVID: how bad is the second wave? BBC News, May 7, 2021.
- Sen M. Black fungus: These two states account for nearly 42% of Indiaâ??s 28,252 mucormycosis cases. Mint, June 7, 2021.
- Eucker J, et al. Mucormycosis. Mycoses, Vol. 44, No. 7, 2001, pp. 253-260. [Crossref][Googlescholar][Indexed]
- Mandell GL et al. Mandell, Douglas and Bennetts principles and practice of infectious diseases, 5th ed. Elsevier, USA, 2000.
- Government of India, Ministry of Health and Family Welfare. Clinical management protocol for COVID-19 in adults. 2021.
- Pakdel F, et al. Mucormycosis in patients with COVID-19: a cross-sectional descriptive multicentre study from Iran. Mycoses. Vol. 64, No. 10, 2021, pp. 1238-1252. [Crossref][Googlescholar][Indexed]
- Sen M, et al. Epidemiology, clinical profile, management and outcome of COVID-19-associated rhino-orbital cerebral mucormycosis in 2826 patients in India-collaborative OPAI-IJO Study on Mucormycosis in COVID-19 (COSMIC), report 1. Indian Journal of Ophthalmology, Vol. 69, No. 7, 2021, pp. 1670-1692. [Crossref][Googlescholar][Indexed]
- Ramaswami A, et al. COVID-19 associated mucormycosis presenting to the emergency department-an observational study of 70 patients. QJM, Vol. 114, No. 7, 2021, pp. 464-470. [Crossref][Googlescholar][Indexed]
- Bhuyan A. Experts criticise Indiaâ??s complacency over COVID-19. The Lancet, Vol. 397, No. 10285, 2021, pp. 1611-1612. [Crossref][Googlescholar][Indexed]
- Gokulshankar S, Mohanty BK. COVID-19 and black fungus. Asian Journal of Medicine and Health Sciences, Vol. 4, No. 1, 2021, pp. 138. [Googlescholar]
- Brewster CT, et al. Steam inhalation and paediatric burns during the COVID-19 pandemic. The Lancet, Vol. 395, No. 10238, 2020, pp. 1690. [Crossref][Googlescholar][Indexed]