Research - International Journal of Medical Research & Health Sciences ( 2022) Volume 11, Issue 6
Non-Sacral Ewing’s Sarcoma: A Rare Entity
2Department of Anaesthesia, Dr. B R Ambedkar State Institute of Medical Sciences, Mohali, India
Ravneet Kaur Gill, Department of Anaesthesia, Dr. B R Ambedkar State Institute of Medical Sciences, Mohali, India, Email: drravneetkgill@gmail.com
Received: 10-Jun-2022, Manuscript No. ijmrhs-22-66322; Editor assigned: 13-Jun-2022, Pre QC No. ijmrhs-22-66322 (PQ); Reviewed: 21-Jun-2022, QC No. ijmrhs-22-66322 (Q); Revised: 21-Jun-2022, Manuscript No. ijmrhs-22-66322 (R); Published: 30-Jun-2022
Abstract
Ewing’s Sarcoma (ES) mainly affects the second decade of life with long bones as the preferred site. Chromosomal translocation of t (11;22) is the most common abnormality associated with it. The spine is rarely involved and most commonly sacrum is involved. Non-sacral ES is rare and especially in middle age. We hereby report a case where a 46-year female had L2 vertebral pathological fracture (due to non-sacral ES) and presented as acute paraparesis.
Keywords
Ewing’s Sarcoma (ES), Non-sacral ES, Lumbar ES
Introduction
The spine is a rare site of involvement in primary sarcomas with an incidence rate of 3.5%-14.9% [1]. Ewing’s Sarcoma (ES) is the second most common primary bone tumor mainly manifesting in the second decade of life and has a predilection for the long bones of the extremities and the pelvis. The sacrum remains the preferred site for primary involvement in the spine whereas non-sacral spinal involvement accounts for approximately 0.9% of all cases [2]. The first case of spinal Ewing’s sarcoma was reported in 1945 in a 21-year-old male [3]. Spinal Ewing’s sarcoma represents vague symptoms of low back ache or visible swelling which can be occasionally confused with infective pathology but aggressive symptoms of neurological involvement are rare. We report a rare case of lumbar spine Ewing’s sarcoma in a middle-aged female that presented with acute paraparesis and was managed with surgical decompression.
Case Report
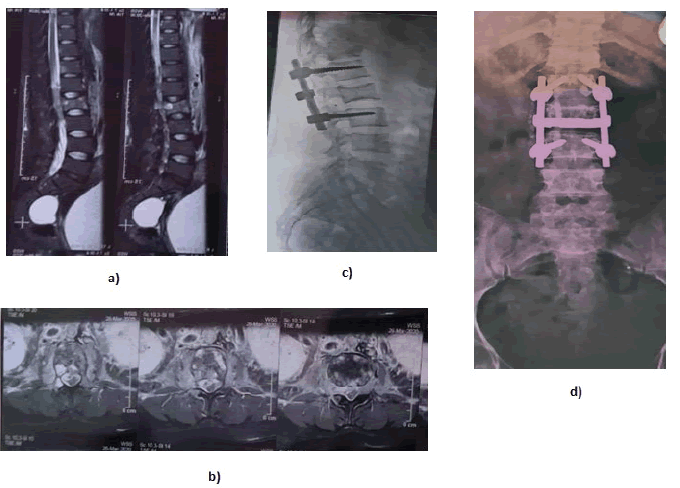
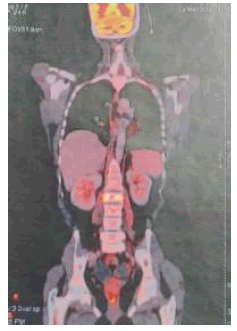
A 46-year-old female patient presented to us with low backache for 2 months associated with weakness of both limbs for 2 weeks. Repeated numbness with difficulty in walking was the main concern of the patient. On neurological examination, she had motor power of 2/5 in both her lower limbs. Tone and power in both upper limbs were unaffected. Reflexes in both lower limbs were exaggerated. Magnetic Resonance Imaging (MRI) screening of the whole spine revealed a pathological fracture of L2 vertebrae and para-vertebral and intra-spinal soft tissue mass at the L2 vertebra along with effacement of exiting nerve roots (Figure 1). No significant changes were seen at other levels. A needle biopsy was done which revealed monomorphic small round cells with scanty cytoplasm which gave a provisional diagnosis of the metastatic cause. Oncology consultation was sought after which preoperative chemotherapy was started. As the patient developed deterioration of power in their lower limbs, she underwent L2 laminectomy and posterior fixation along with the removal of the extradural mass, using a posterior midline incision in the prone position. Histopathological examination of the specimen was consistent with a diagnosis of Ewing sarcoma. Immunohistochemistry revealed strong reactivity for CD 99, Vimentin, FLI-1, and NKX2.2. The Ki-67 proliferation index was 70%. MRI brain and whole body Positron Emission Tomography (PET) scan (Figure 2) showed no other tumor sites or distant metastases, and thus a diagnosis of primary spinal primitive neuroectodermal tumor (ES) was established. Postoperative improvement was gradually seen and the patient was referred to the oncology department for further management. The patient was followed up in both departments for further 16 months which was uneventful.
Discussion
ES is a neuro-ectodermal tumor associated with various chromosomal translocations but the most common is the reciprocal translocation t(11;22)(q24;q12). Long bones of the lower extremities (45%) are the main sites of presentation followed by the pelvis (20%), upper extremities (13%), an axial skeleton with ribs (13%), and face (2%) [4]. Spine as the primary site is rarely encountered and often confused with infective etiology [5]. Since the initial presentation varies widely from non-specific symptoms of fever and gradual backache, it is misdiagnosed up to 80% in the first presentation [6]. 30%-50% of patients complain of low-grade fever [3]. Such presentation poses a huge problem in developing countries like India where infective etiologies like tuberculosis are endemic and also present in a similar manner [7]. Patients tend to report to a hospital only after the symptoms aggravate and hamper their daily proceedings. Generalized features which often resemble infective etiology are treated at local hospitals with empirical antibiotics and analgesics. This leads to a delay in the diagnosis and thus inadvertently leads to the progression of the disease.
ES is mainly encountered in the second decade of life with a peak at 15-17 years, being rare in adults [8]. In our patient of 46 years, the initial presentation was very much similar to infective etiology and tuberculosis was the main differential diagnosis. MR imaging along with needle biopsy pointed towards metastatic pathology. Sacrum remains the preferred site in the spine but rare involvement of lumbar vertebrae is also mentioned. Laminectomy with decompression and fixation remains the modality of choice in neuro-compromised patients and it was beneficial to our patient as it lead to a slight improvement of power in both the lower limbs [9].
Preoperative chemotherapy targets at reducing the tumor size and controlling the micrometastasis. Most commonly regimen of vincristine, adriamycin, cyclophosphamide, ifosfamide, and etoposide is used. In India various regimens are followed one being the POG 9354 protocol which includes four to five cycles of neoadjuvant chemotherapy vincristine, adriamycin and cyclophosphamide alternated with etoposide and ifosfamide for 48 weeks. The initial use of radiotherapy (limit <45 Gy) can be given in patients with epidural compression but cord edema can further aggravate the neurological compromise. The multidisciplinary approach offers survival rates of 50% to 80% and gives an acceptable level of life.
Conclusion
Although a rare entity, especially in the age group of >45 years, non-sacral spinal ES may be encountered which may masquerade as infective pathology. An aggressive and timely approach may be the essential factor determining the residual effects of the neurological compromise in such cases.
Declarations
Conflict of Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
REFERENCES
- Gopalakrishnan, C. V., et al. "Primary Ewing's sarcoma of the spine presenting as acute paraplegia." Journal of Pediatric Neurosciences, Vol. 7, No. 1, 2012, pp. 64-66.
Google Scholar Crossref - Bemporad, Joshua A., et al. "Pseudohemangioma of the vertebra: An unusual radiographic manifestation of primary Ewing's sarcoma." American Journal of Neuroradiology, Vol. 20, No. 10, 1999, pp. 1809-13.
Google Scholar - Bhat, Guruprasad, and Srijit Padmanabh. "Ewing's sarcoma of the spine: Misdiagnosed as tuberculosis and presenting as paraplegia." Archives of Medicine and Health Sciences, Vol. 6, No. 2, 2018, pp. 257-59.
Google Scholar - Grier, Holcombe E. "The Ewing family of tumors: Ewing's sarcoma and primitive neuroectodermal tumors." Pediatric Clinics of North America, Vol. 44, No. 4, 1997, pp. 991-1004.
Google Scholar Crossref - Haresh, K. P., et al. "A rare case of intradural extramedullary Ewing's sarcoma with skip metastasis in the spine." Spinal Cord, Vol. 46, No. 8, 2008, pp. 582-84.
Google Scholar Crossref - Widhe, Björn, Torulf Widhe, and Henrik CF Bauer. "Ewing sarcoma of the rib-initial symptoms and clinical features: Tumor missed at the first visit in 21 of 26 patients." Acta Orthopaedica, Vol. 78, No. 6, 2007, pp. 840-44.
Google Scholar Crossref - Rajappa, Srinivasan, P. Gopinath Menon, and Sandhya Sundaram. "Ewings sarcoma of the hand-A case report." Journal of Hand and Microsurgery, Vol. 2, No. 2, 2010, pp. 82-84.
Google Scholar Crossref - Iacoangeli, Maurizio, et al. "Nonmetastatic Ewing’s sarcoma of the lumbar spine in an adult patient." Case Reports in Oncological Medicine, Vol. 2012, 2012.
Google Scholar Crossref - Dini, Leandro I., Rodrigo Mendonca, and Pasquale Gallo. "Primary Ewing's sarcoma of the spine: Case report." Neuropsychiatry Archives, Vol. 64, 2006, pp. 654-59.
Google Scholar Crossref