Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 5
Necrotizing Soft Tissue Infections: Management and its Outcome in a Tertiary Health Care Center: An Observational Study
Ab. Hamid Wani, Satish Parihar, Javid Iqbal, Sourabh Katoch*, Sanjay Dhar and Nasib Chand DigraSourabh Katoch, Department of Surgery, Government Medical College Jammu, Jammu and Kashmir, India, Email: drhamid121@gmail.com
Received: 21-Apr-2021 Accepted Date: May 18, 2021 ; Published: 25-May-2021, DOI: O
Abstract
Background: Necrotizing Soft Tissue Infections (NSTIs) is a life-threatening condition encountered by surgeons with high morbidity and mortality. It is a rapidly progressive disease and the overall mortality ranges between 25%-35% even in the best centers.
Aim: To study epidemiology, management, and outcome of patients with NSTIs.
Methods: Fifty patients were included in this observational study, irrespective of age and gender, all patients were thoroughly evaluated, investigated, resuscitated and debridement was done.
Results: Wound debridement was done in all patients, diversion in the form of colostomy was done in 03 (6%) patients and skin grafting in 17 (34%) patients, healing by secondary intention in 12 (24%) patients, delayed primary closure in 05 (10%) patients, local pedicle flap in 02 (4%) patients and rotational flap in 02 (4%) patients, with an overall mortality of 18% (09) patients.
Conclusion: Early diagnosis and treatment in the form of broad-spectrum antibiotics, multiple debridements’ and proper wound care is the key to success.
Keywords
NSTIs (Necrotizing Soft Tissue Infections), GAS (Group A beta-hemolytic Streptococci), CRF (Chronic Renal Failure)
Introduction
Necrotizing Soft Tissue Infections (NSTIs) are serious and life-threatening infections encountered by surgeons [1]. NSTIs initially start in the dermis and epidermis and then involve the deeper layers like adipose tissue, fascia, and muscles [2]. They are caused by toxin-producing bacteria and characterized by rapid progression of the disease with significant local tissue destruction, systemic toxicity, and death depending upon the strain of bacteria and toxins produced [3]. The mortality rate is as high as 25% to 35% even with optimal treatment. NSTIs can occur in any area of the body but most commonly involves extremities (60%-80%), perineum and genitalia (12%-16%), and chest or abdomen (10%-12%). NSTIs are 3 types [3]. Type I infections are poly-microbial with various species of grampositive, gram-negative, and anaerobic bacteria-including Clostridial species. Type II infections involve Group A β-hemolytic Streptococci (GAS), either alone or in combination with staphylococcal species. Type III NSTIs are caused by gram-negative marine organisms, most commonly Vibrio vulnificus. Poly-microbial NSTIs are more commonly encountered than mono-microbial [4]. Impaired host immunity, local tissue hypoxia as in atherosclerosis, burns, cancer, corticosteroid use, diabetes mellitus, peripheral vascular disease, postoperative infection, and trauma are predisposing factors for NSTIs [5]. The present study was undertaken to evaluate the epidemiology, management, and outcome of patients with NSTIs.
Material and Methods
The study was conducted in the post-graduate department of surgery Government Medical College Jammu and fifty patients were included in the study over three years between 2017-2019. Detailed history, Clinical examination which includes general and systemic examination along with a local examination of the affected area to look for the site, size, color, discharge, pain or painless, odor from the wound, whether there was any restriction in the mobility due to the involved area and any foreign body present in the wound. Any history of trauma including surgical intervention, any burn, long-term comorbid conditions, insect or snake bite was also ruled out. Laboratory parameters included routine hematological workup, urine examination, ABG, liver function tests with serum proteins and albumin, wound cultures, blood culture, tissue biopsies, etc. Plain radiography, ultrasonography, computed tomography, and MRI were done as per treatment protocol as and when required.
Inclusion Criteria
• All patients with necrotizing soft tissue infection irrespective of age and gender
• Intraoperatively diagnosed case of necrotizing fasciitis
Exclusion Criteria
• Localized subcutaneous infections
• Bedsores
The patient treatment modalities and their outcome were assessed and a note was made of any diversion, grafting, or any other procedure. Associated comorbid conditions were noted. Patients were analyzed as per the severity of the disease, the bacteriological study of the affected area, and the outcome.
Results
Fifty patients included in this study were in the age group of 09 days old to 77 years with a mean age of 47.46 ± 17.04 years. Most of the patients were male (36) and females (14), and the most common occupation among the patients presenting to us were farmers 28 (56%) followed by skilled 09 (18%) employees 06 (12%) and others 07 (14%). The most common site affected was perineal 23 (46%), lower limb 15 (30%) trunk in 6 (12%) patients, and 06 (12%) others like upper limbs, breast, and chest. The commonest presentation was pain (50%) cases, swelling in 24%, discharge in 16% and fever was present in about 10% cases. 10% of patients presented within 01 weeks of clinical symptoms, 24% in the 2nd week, and 66% after 02 weeks. The mean duration of the presentation was 24.30 ± 17.59 days. Erythema and edema were the most common clinical signs and were seen in about 94% and 30% cases respectively. 56% of patients were found to be anemic. 36% of patients were found to be having raised blood sugar levels and 57% of patients were having raised serum creatinine levels. Most of the cases were idiopathically followed by trauma as a cause as shown in Table 1.
| Etiology | No. of Patients | Percentage |
|---|---|---|
| Idiopathic | 20 | 40% |
| Trauma | 14 | 28% |
| Burns | 6 | 12% |
| Post-surgery | 2 | 4% |
| Paraplegia | 2 | 4% |
| Long segment myelitis | 3 | 6% |
| Injection | 1 | 2% |
| Road traffic accident | 1 | 2% |
| Lactation | 1 | 2% |
Table 1: Etiology of necrotizing soft tissue infections
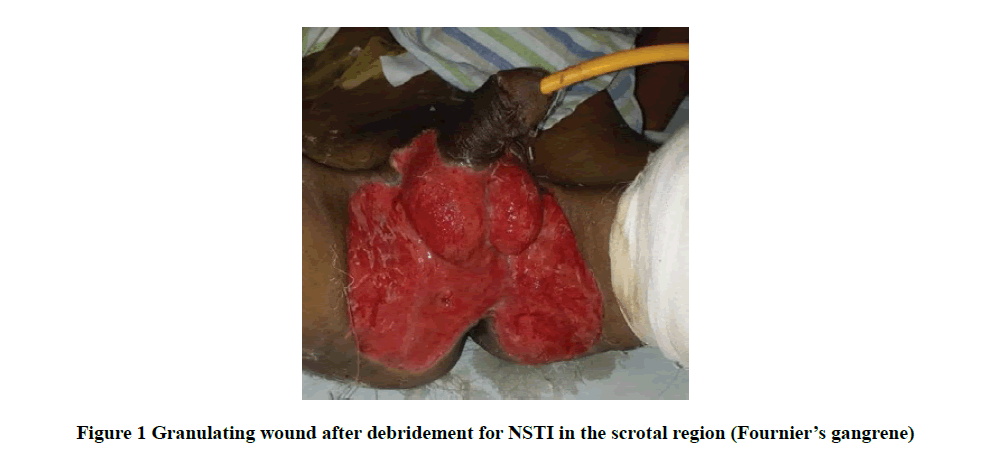
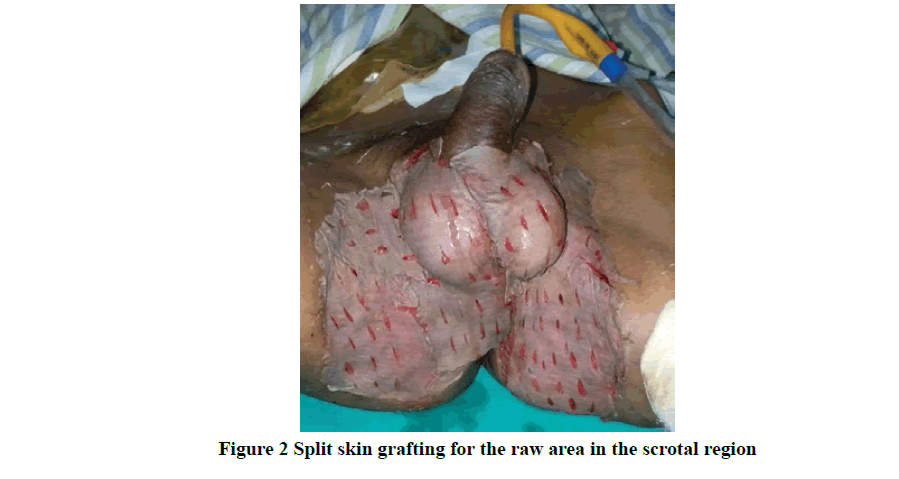
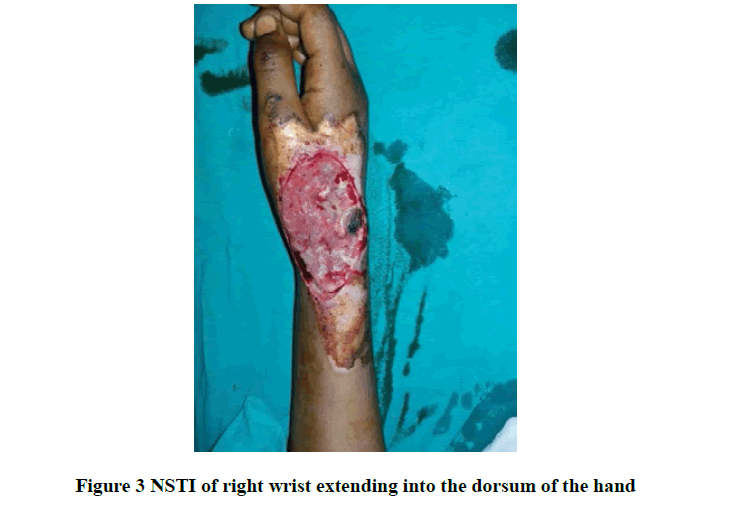
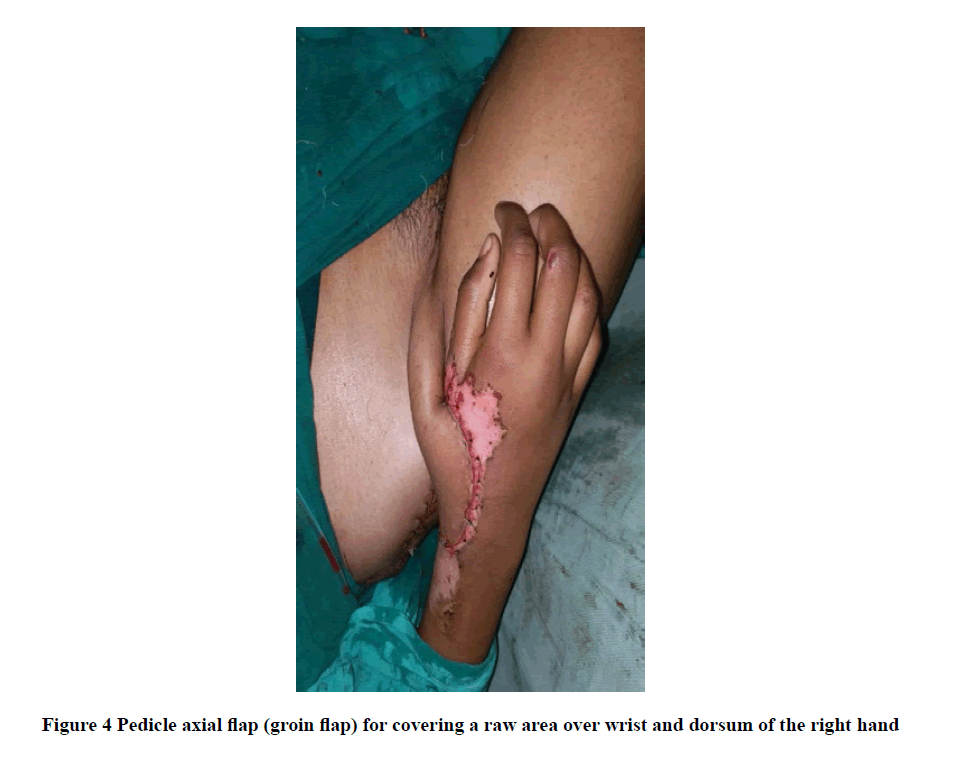
The commonest comorbidity being diabetes mellitus, hypertension, and CRF, microbiological examination revealed mono-microbial infection in 74% (37) cases and poly-microbial in 26% (13) cases. The commonest organism cultured was Escherichia coli in 56%, followed by Staphylococcus aureus in 40% and Pseudomonas in 30%. All the patients initially received broad-spectrum antibiotics and it consists of a cephalosporin with aminoglycoside and metronidazole. Wound debridement (Figure 1) was performed in all patients, 34% require SSG as shown in Figure 2, 6% needed diversion in the form of colostomy, and 8% needed flap coverage including local pedicle flap (Figure 3 and Figure 4) and rotational flap as shown in Table 2.
| Treatment | No. of patients | Percentage |
|---|---|---|
| Debridement is followed by healing by secondary intention | 12 | 24% |
| Debridement followed by SSG | 17 | 34% |
| Debridement, diversion, and healing by secondary intention | 3 | 6% |
| Debridement followed by flaps cover | ||
| a. Local pedicle flap | 2 | 8% |
| b. Rotational Flap | 2 | |
| Debridement followed by delayed primary closure | 4 | 10% |
| Repeated debridement due to extension of NSTIs | 9 | 18% |
Table 2: Management in different patients
Hospital stay ranges between 07 to 30 days with a mean of 16 days. The overall mortality was 18% (09) patients. In these patients, multiple debridement’s were done but they developed sepsis and died.
Discussion
Necrotizing Soft Tissue Infections (NSTIs) predominantly occur in males, with a higher incidence in an older population with trauma as the most common etiological factor [6,7]. In the present study, the incidence was highest among the farmers as most of our patients belong to the rural population. This pattern shows that by improving the hygiene, safety, and working environment, the incidence of NSTIs can be reduced. The majority of the cases of NSTIs follow minor injury due to trauma, RTA, insect bite, etc. Poor care for the wound following the trivial trauma is the major cause of NSTIs. The incidence of NSTIs was highest following the trauma. The foreign body that might get lodged or the deep inoculation that occurs with trauma and other cause forms a perfect place for the organisms to flourish and complemented by lowered host defense due to alcoholism, diabetes which leads to fulminant local infection leading to necrotizing infection. Sharma SK in a retrospective study had shown that trauma to be the most common etiological factor with diabetes as the associated comorbid condition [8]. Most of the cases in the present study were idiopathic with the commonest associated comorbid conditions like diabetes, hypertension, CRF, etc. In the present study, we found that the perineum was the most common site for necrotizing soft tissue infection followed by the lower limb and upper limb. The least common site involved was the anterior abdominal wall. Similar studies conducted in other parts of the world show the perineum as the most common site of necrotizing soft tissue infection like in the studies of Mpirimbanyi, et al. [9]. Most of the patients in this study present with pain, swelling, and discharge from the affected area which is supported by the studies of Headley AJ, et al. [10]. The commonest signs were edema followed by ulcer which correlates with the study of Singh G, et al. [11]. The most common organism isolated from the wound site was E. coli followed by Staphylococcus aureus, Pseudomonas, Streptococcus, and mono-microbial infection in 74% of cases. Thirunavukkarasu S and Ragumani P in their study found E. coli to be the most common organism involved in polymicrobial infections [7].
Three patients needed diversion in the form of colostomy due to extensive infection of the perineum in our study which correlates with a study by Khan P, et al. [12]. In the present study, 09 patients died with a mortality rate of 18% (09/50). The various factors that contributed to the mortality included advanced age, involvement of multiple areas, raised serum creatinine, deranged liver function tests, DM, hypertension, CKD, immunosuppression, etc. Similar results were seen in a study by Elliot DC, et al. [13].
Conclusion
Early diagnosis in patients with a high degree of clinical suspicion of NSTIs, use of broad-spectrum antibiotics, liberal and multiple debridement of infected areas, and early skin cover is the key to success.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Anaya, Daniel A., et al. "Predicting death in necrotizing soft tissue infections: A clinical score."Surgical Infections,Vol. 10, No. 6, 2009, pp. 517-22.
- Anaya, Daniel A., et al. "Predictors of mortality and limb loss in necrotizing soft tissue infections."Archives of Surgery,Vol. 140, No. 2, 2005, pp. 151-57.
- Hakkarainen, Timo W., et al. "Necrotizing soft tissue infections: Review and current concepts in treatment, systems of care, and outcomes."Current Problems in Surgery,Vol. 51, No. 8, 2014, pp. 344-62.
- Giuliano, Armand, et al. "Bacteriology of necrotizing fasciitis."The American Journal of Surgery,Vol. 134, No. 1, 1977, pp. 52-57.
- Das, Dilip Kumar, Michael G. Baker, and Kamalesh Venugopal. "Increasing incidence of necrotizing fasciitis in New Zealand: A nationwide study over the period 1990 to 2006."Journal of Infection,Vol. 63, No. 6, 2011, pp. 429-33.
- Kalaivani, V., and Bharati V. Hiremath. "Necrotising soft tissue infection-risk factors for mortality."Journal of Clinical and Diagnostic Research: JCDR,Vol. 7, No. 8, 2013, pp. 1662-65.
- Thirunavukkarasu, S., and P. Ragumani. "Necrotizing soft tissue infections: Our experience at Govt. Royapettah Hospital." IOSR: Journal of Dental and Medical Sciences, Vol. 15, No. 7, 2016, pp. 9-13.
- Sharma, Santosh Kumar. "Necrotizing soft tissue infections-A study in tertiary centre of North Bihar."Journal of Medical Science and Clinical Research,Vol. 5, No. 7, 2017, pp. 25653-56.
- Mpirimbanyi, Christophe, et al. "Necrotizing soft tissue infections at a tertiary referral hospital in Rwanda: Epidemiology and risk factors for mortality."World Journal of Surgery,Vol. 42, No. 8, 2018, pp. 2314-20.
- Headley, Adrienne J. "Necrotizing soft tissue infections: A primary care review."American Family Physician,Vol. 68, No. 2, 2003, pp. 323-28.
- Singh, Gurpreet, et al. "Necrotising infections of soft tissues-A clinical profile."European Journal of Surgery,Vol. 168, No. 6, 2002, pp. 366-71.
- Kha, Pauline, et al. "Necrotizing soft-tissue infections in New Caledonia: epidemiology, clinical presentation, microbiology, and prognostic factors."Asian Journal of Surgery,Vol. 40, No. 4, 2017, pp. 290-94.
- Elliott, David C., Joseph A. Kufera, and Roy AMMD Myers. "Necrotizing soft tissue infections. Risk factors for mortality and strategies for management."Annals of Surgery,Vol. 224, No. 5, 1996, pp. 672-83.