Research - International Journal of Medical Research & Health Sciences ( 2022) Volume 11, Issue 10
Morphometric Study of Orbitary and Periorbitary Region in Peruvian Skulls: Importance to Surgical Approach
Saenz-Poma Gustavo1,2, Chavez-Asmat Roberto Jesus2,3,4*, Anampa-Guzman Andrea5 and Shiroma-Castro Julio22Faculty of Human Medicine, National University of San Marcos, Lima, Peru
3Development of Student Research in Health Sciences (ADIECS), Lima, Peru
4Hospital de Caridade Sao Vicente de Paulo, Brazil
5San Fernando Scientific Society (SCSF), Lima, Peru
Chavez-Asmat Roberto Jesus, Hospital de Caridade Sao Vicente de Paulo, Brazil, Email: Rjasmat7@gmail.com
Received: 01-Oct-2022, Manuscript No. ijmrhs-22-76349; Editor assigned: 19-Oct-2022, Pre QC No. ijmrhs-22-76349 (PQ); Reviewed: 24-Oct-2022, QC No. ijmrhs-22-76349 (Q); Revised: 24-Oct-2022, Manuscript No. ijmrhs-22-76349 (R); Published: 30-Oct-2022
Abstract
Background: The orbit is a conical structure where lies the elements that allow vision. The volume of the orbit and the distances between its reference points vary depending on race and sex, so there are different values determined around the world. Methods: Sixty adult human dried skulls from the collection of the Department of Morphological Sciences, San Marcos, Lima-Peru; were used in the present study, on request and authorization. The orbital and periorbital region were measured bilaterally using Digital Vernier Caliper “Onogal”® and the volume of orbit was determined in ml, using a modified method of displaced volume. Results: Significantly lower values were found in the medial wall from the left eye (Student's T-test, p=0.01), specifically in the distance from the Anterior Lacrimal Crest (ALC) to the Anterior Ethmoidal Foramen (AEF). Also, the lateral wall presented lower values (p=0.01) in the distance from Zygomatico Frontal Suture to the Lacrimal Fossa (ZFS-LF). Conclusions: Measurements of a medial and lateral wall from the Peruvian skulls were lower in the left orbital region, compared with the right side; and volume measurements are similar to findings from previous studies in Asian skulls. The similar genetic traits between Asian and Amerindian (Quechua-Aymara) races could explain these findings.
Keywords
Morphometry, Orbit, Skull, Peru
Introduction
The orbit is a conic structure where lie the elements that allow vision and is composed of the orbital region, including its lateral and medial walls, floor and roof; and the periorbital region. Each of these parts has useful points of reference in the surgical approach [1]. The volume of the orbit could be modified by an alteration in the tissue occupying this space (muscles, nerves, vessels, etc), deteriorating ultimately the function of vision. The causes of this alteration could be a trauma, tumor, infectious or endocrinal pathology [2].
The volume of the orbit and the distances between its reference points vary according to race and sex, having different values determined worldwide. In China, the 3D reconstruction technique was used to describe 11 anatomical parameters while in Taiwan, a similar technique was used to calculate the orbital volume [3]. In addition, the dimensions of the bottom and side wall of 11 dried skulls of adult patients were measured in Thailand [4]. Indian dry skulls were used to measure 17 anatomical parameters as well as the variability of position, shape, size, and incidence of the infraorbital foramen and 4 parameters of the supraorbital region [5]. Computed tomography and software were used to determine the orbital volume in European adult skulls [6]. Also, 19 parameters of the upper, lower, and lateral orbit walls were measured with millimetriccompass [7]. Other research emphasized the geometric and morphometric relationships of the ethmoidal foramen with the orbital apex [1]. In Latin America, a study in Chile determined the orbital volume using the principle of Cavalieri supplemented with sequential analysis of computed tomography in dry skulls [5]. Brazilian skulls were examined to 3-D parameters around the infraorbital foramen [8].
No data about Peruvian skulls have been reported in the literature. Therefore, it is necessary to study this population, to get a better comprehension of orbital and periorbital morphometry and its possible applications. Measurements of these dimensions are important to know the safe surgical distance to avoid damage to structures found in the orbit such as the optic nerve, the ophthalmic artery, the trochlear nerve, the ethmoidal arteries, and other sensory nerves. In addition, during an orbital reconstruction after trauma or tumours, comprehension of orbital volume is fundamental to restoring the anatomy of this region.
This study aimed to determine the distances between the various points of reference of the orbit and the orbital volume in Peruvian skulls.
Methods
Sixty adult human dried skulls of unknown age and sex from the collection of the Department of Morphological Sciences, Faculty of Medicine, "San Fernando" of San Marcos, Lima-Peru were used in the present study, on request and authorization. The skulls with damages or apparent anomalies in the area of measurement were excluded. The orbital and periorbital region from the skulls were measured bilaterally using Digital Vernier Caliper “Onogal”®. The volume of the orbit was determined by applying 5 mg of dental sticky wax "Top Was", which was placed with a strainer to seal the holes of the orbit. Then, the mold obtained was filled with distilled water to determine the volume in ml (Figures 1 and 2).
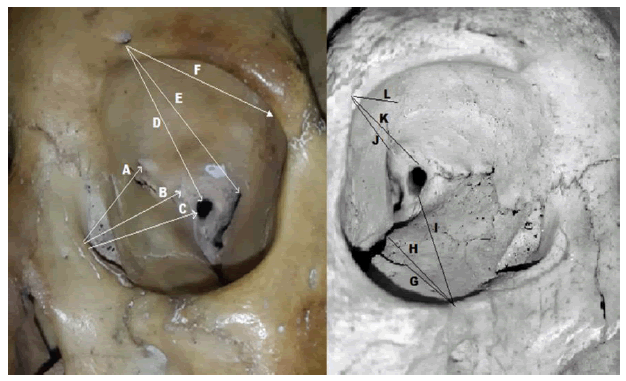
Figure 1. Orbital Measurements: Left image A) Anterior Lacrimal Crest-Anterior Ethmoidal Foramen (ALC-AEF). B) Anterior Lacrimal Crest-Posterior Ethmoidal Foramen (ALC-PEF). C) Anterior Lacrimal Crest-Optic Foramen (ALC-OF). D) Supraorbital Foramen-Optic foramen (SOF-OF). E) Supraorbital Foramen-Posterior Sphenoid Fissure (SOF-PSF). F) Supraorbital ForamenLacrimal Fossa (SOF-LF). Right Image: G) Infraorbital Margin-Anterior Margin of Infraorbital Canal (IOM-AMC). H) ) Infraorbital Margin-Anterior Sphenoid Fissure (IOM-AEF). I) ) Infraorbital Margin-Optic Foramen (IOM-OF). J) Zygomaticofrontal SuturePosterior Sphenoid Fissure (ZFS-PEF). K) Zygomaticofrontal Suture-Optic Foramen (ZFS-OF). L) Zygomaticofrontal Suture-Lacrimal Fossa (SFC-LF).
Morphometric data, such as lengths and volume, were expressed as mean ± Standard Deviation (SD). The Student's T test was performed to compare the mean value of the right and left sides. A p-value <0.05 was considered statistically significant; the data was analyzed using the SPSS V.18 program.
Results
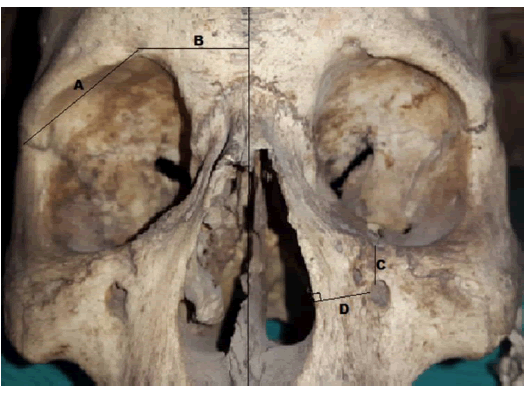
Measurements of the periorbital region were divided into supraorbital, which includes the distances between Nasal Midline-Supraorbital Foramen (NM-SOF) and Supraorbital Foramen-Zygomaticofrontal Suture (SOF-ZFS); and infraorbital, corresponding to the distances of the Infraorbital Foramen-Pyriform aperture (IOF-PA) and Infraorbital Foramen-Infraorbital Margin (IOF-IOM). No significant difference was found between both eyes (Table 1).
| Measurements | Total | RE | LE | p* | |
|---|---|---|---|---|---|
| Supraorbital | NM-SOF | 24.07 ± 3.57 | 24.09 ± 3.49 | 24.05 ± 3.67 | 0.95 |
| SOF-ZFS | 30.20 ± 2.76 | 30.17 ± 2.68 | 30.23 ± 2.86 | 0.90 | |
| Infraorbital | IOF-PA | 16.49 ± 1.64 | 16.39 ± 1.53 | 16.60 ± 1.75 | 0.48 |
| IOF-IOM | 7.28 ± 1.88 | 7.11 ± 1.89 | 7.45 ± 1.87 | 0.32 | |
|
RE: Right eye. LE: Left eye. |
|||||
|
NM-SOF: Nasal Midline-Supraorbital foramen. |
|||||
|
SOF-ZFS: Supraorbital foramen-Zygomaticofrontal suture. |
|||||
|
IOF-PA: Infraorbital foramen-Pyriform aperture. |
|||||
|
IOF-IOM: Infraorbital foramen-Infraorbital margin. |
|||||
|
Values expressed in mm (mean ± DS)* T Student`s T-Test: RE vs LE. |
|||||
Measurements of the orbital region were described in Table 2. Significantly lower values were found in the medial wall of the left eye (Student's T, p=0.01), specifically in the distance from the Anterior lacrimal crest to the Anterior Ethmoidal Foramen (ALC-AEF). In addition, the distance from the Zygomaticofrontal suture to the Lacrimal fossa (ZFS-LF) has lower values in the lateral wall (Student's T, p=0.01).
| Measurements | Total | RE | LE | p* | |
|---|---|---|---|---|---|
| Roof | SOF-LF | 18.50 ± 2.53 | 18.16 ± 2.56 | 18.84 ± 2.46 | 0.13 |
| SOF-PSF | 40.86 ± 4.15 | 41.20 ± 4.16 | 40.53 ± 4.15 | 0.38 | |
| SOF-OF | 46.93 ± 2.60 | 47.06 ± 2.78 | 46.79 ± 2.43 | 0.56 | |
| Medial Wall | ALC-AEF | 26.00 ± 2.88 | 26.50 ± 3.11 | 25.49 ± 2.55 | 0.05 |
| ALC-PEF | 35.09 ± 2.66 | 35.74 ± 2.71 | 34.45 ± 2.47 | 0.01 | |
| ALC-OF | 43.24 ± 2.45 | 43.39 ± 2.33 | 43.10 ± 2.58 | 0.50 | |
| Lateral Wall | ZFS-LF | 12.38 ± 1.52 | 12.80 ± 1.68 | 11.96 ± 1.21 | 0.01 |
| ZFS-PSF | 35.54 ± 2.92 | 35.61 ± 3.40 | 35.46 ± 2.37 | 0.77 | |
| ZFS-OF | 46.52 ± 2.34 | 46.44 ± 2.63 | 46.60 ± 2.02 | 0.68 | |
| Floor | IOM-OF | 46.56 ± 2.48 | 46.44 ± 2.50 | 46.67 ± 2.47 | 0.61 |
| IOM-AEF | 22.33 ± 3.01 | 22.34 ± 3.02 | 22.33 ± 3.01 | 0.98 | |
| IOM-AMC | 13.26 ± 2.63 | 13.20 ± 2.60 | 13.31 ± 2.68 | 0.82 | |
| RE: Right eye. LE: Left eye. | |||||
| SOF-LF: Supraorbital foramen-Lacrimal fossa. | |||||
| SOF-PSF: Supraorbital foramen-Posterior sphenoid fissure. | |||||
| SOF-OF: Supraorbital foramen-Optic foramen. | |||||
| ALC-AEF: Anterior lacrimal crest-Anterior ethmoidal foramen. | |||||
| ALC-PEF: Anterior lacrimal crest-Posterior ethmoidal foramen. | |||||
| ALC-OF: Cresta lacrimal anterior-Optic foramen. | |||||
| ZFS-LF: Zygomaticofrontal suture-Lacrimal fossa. | |||||
| ZFS-PSF: Zygomaticofrontal suture-Posterior sphenoid fissure. | |||||
| ZFS-OF: Zygomaticofrontal suture-Optic foramen. | |||||
| IOM-OF: Infraorbital margin-Optic foramen. | |||||
| IOM-ASF: Infraorbital margin-Anterior sphenoid fissure. | |||||
| IOM-AMC: Infraorbital margin-Anterior margin of infraorbital canal. | |||||
| Values expressed in mm (mean ± DS) * T Student`s T -Test: RE vs LE. | |||||
The overall orbital volume was 24.72 ± 1.72 ml, 24.63 ± 1.77 ml for the right eye, and 24.81 ± 1.68 ml for the left eye, with no significant difference between them.
Discussion
Comprehension of the orbital and periorbital morphometry is important during the surgical approach, to avoid complications as a consequence of damage to the important nervous and vascular structures that lie in this region (blood vessels, nerves). These precedents could involve reconstructive surgery, post-ablative cancer surgery, craniofacial trauma, aesthetic facial skeleton, and others.
The present results would be useful to make certain surgical approaches to the orbit safer. If the orbit is approached from the floor (eg. subsidiary, sub-palpebral, and transconjunctival approaches), the surgeon must consider that the closest structure to be found from the Infraorbital Margin (IOM) is the anterior margin of the Infraorbital Canal (AMC), 13.26 mm ± 2.63 mm away, where the trigeminal nerve (V2) runs. Additionally, the distance from IOM to the optic nerve is 46.56 ± 2.4
If the orbit is approached from the medial wall (eg. transcaruncular, caruncular, and Lynch approaches), the distance between the Anterior Lacrimal Crest (ALC) to the optic nerve is 43.24 mm ± 2.45 mm and the first structure to be found in the anterior ethmoid artery that runs through the Anterior Ethmoid Foramen (AEF) (26 mm ± 2.28 mm). If the orbit is approached from the lateral wall (eg. Stallard-Wright incision and canthotomy incision), the zygomaticofrontal Suture (ZFS) is 46.32 mm ± 2.34 mm away from the optic nerve. Finally, during an approaching through the roof (eg. coronal and suprapalpebral incisions), it would be considered that the Supraorbital Foramen(SOF) is 46.93 mm ± 2.60 mm away from the optic nerve and 40.86 mm ± 2.15 mm away from the Posterior Sphenoid Fissure (PSF). Subtracting 5 mm to 10 mm from these measurements seems to be a proper technique to safely enter the optic foramen during an orbit surgery.
Measurements of the periorbital region, like distance from the nasal midline to the Supraorbital Foramen (NM-SOF) and from the supraorbital foramen to the Zygomaticofrontal Suture (SOF-ZFS), were similar to those found previously in two studies [2,9]. The distance from the infraorbital foramen to the Pyriform Aperture (IOF-PA) coincides with previous morphometric analysis of infraorbital for men made in Indian skulls but is lower than those obtained in Brazilian skulls (Table 3) [10]. Measurements of the orbital region in the present study mostly coincide with three studies being slightly lower in the SOF-LF and ZFS-FL measurements of the roof and side wall respectively (Table 4) [8,11].
| Measurements | Present study | Lopes P et al 2009 | Ashwini L et al 2011 | Singh R 2011 | Sharma N et al 2014 | |
|---|---|---|---|---|---|---|
| Supraorbital | NM-SOF | 24.07 ± 3.57 | 22.22 ± 2.39 | 21.02 ± 0.54 | ||
| SOF-ZFS | 30.20 ± 2.76 | 29.02 ± 0.30 | 28.61 ± 0.27 | |||
| Infraorbital | IOF-PA | 16.49 ± 1.64 | 35.18 ± 4.77 | 15.56 ± 2.31 | ||
| IOF-IOM | 7.28 ± 1.88 | 6.66 ± 1.67 | 6.15 ± 1.80 | |||
NM-SOF: Nasal midline–Supraorbital foramen. SOF-ZFS: Supraorbital foramen–Zigomaticofrontal suture. |
||||||
IOF-PA: Infraorbital foramen–Pyriform aperture. IOF-IOM: Infraorbital foramen- Infraorbital margin. |
||||||
Values expressed in mm (mean ± DS)* T Student`s T -Test: RE vs LE |
||||||
| Measurements | Present study | Karakas P et al 2002 | Thanasil Huanmanop M et al 2007 | Gosavi SN et al 2014 | |
|---|---|---|---|---|---|
| Roof | SOF-LF | 18.50 ± 2.53 | 33.6 ± 3.5 | 32.6 ± 5.3 | |
| SOF-PSF | 40.86 ± 4.15 | 40.0 ± 2.4 | 40.37 ± 3.2 | ||
| SOF-OF | 46.93 ± 2.60 | 45.3 ± 3.2 | 44.70 ± 2.3 | 45.11 ± 3.4 | |
| Medial Wall | ALC-AEF | 26.00 ± 2.88 | 23.9 ± 3.3 | 23.5 ± 2.6 | 20.7 ± 2.97 |
| ALC-PEF | 35.09 ± 2.66 | 35.6 ± 2.3 | 36.0 ± 2.5 | 33.1 ± 2.86 | |
| ALC-OF | 43.24 ± 2.45 | 41.7 ± 3.1 | 42.2 ± 2.3 | 39.71 ± 2.67 | |
| Lateral Wall | ZFS-LF | 12.38 ± 1.52 | 27.2 ± 3.7 | 24.39 ± 2.8 | |
| ZFS-PSF | 35.54 ± 2.92 | 34.5 ± 2.6 | 33.13 ± 3.1 | ||
| ZFS-OF | 46.52 ± 2.34 | 44.9 ± 2.5 | 46.9 ± 2.4 | 45.97 ± 3.9 | |
| Floor | IOM-OF | 46.56 ± 2.48 | 46.2 ± 2.8 | 48.32 ± 2.8 | |
| IOM-FEA | 22.33 ± 3.01 | 21.7 ± 2.0 | 21.51 ± 2.5 | ||
| IOM-MAC | 13.26 ± 2.63 | 12.3 ± 3.7 | 13.04 ± 4.4 | ||
SOF-LF: Supraorbital Foramen-Lacrimal Fossa. SOF-PSF: Supraorbital Foramen-Posterior Sphenoid Fissure. SOF-OF: Supraorbital Foramen-Optic Foramen. ALC-AEF: Anterior Lacrimal Crest-Anterior Ethmoidal Foramen. ALC-PEF: Anterior Lacrimal Crest-Posterior Ethmoidal Foramen. ALC-AO: Anterior Lacrimal Crest-Optic Foramen. ZFS-LF: Zygomaticofrontal suture-lacrimal fossa. ZFS-PEF: Zygomaticofrontal suture-Posterior sphenoid fissure. ZFS-OF: Zygomaticofrontal suture-Optic foramen. IOM-OF: Infraorbital margin-Optic foramen. IOM-ASF: Infraorbital margin-Anterior sphenoid fissure. IOM-AMC: Infraorbital margin-Anterior margin of infraorbital canal. |
|||||
The exact knowledge of the position of the infraorbital nerve, greater wing of the sphenoid, orbital projection of the palatine process, and infraorbital fissure as well as the relationship between them is useful during the dissection of the deep orbit, However, the roof of the orbit, the lateral wall, and the medial wall must still be considered, since trauma can also occur on these walls.
A modified method of displaced volume was used to calculate orbital volume. This method uses distilled water instead of silicone, as in previous studies [10,12]. Although it cannot outline exactly orbital edges, is the gold standard to calculate the orbital volume and can be used to compare the present results with others [9,13]. The mean volume was found to be 24.72 ± 1.72 cc, lower than the average obtained previously with 4 Caucasians skulls (27.15cc), and 10 Chilean skulls (27.47 cc) [5]. However, these results are similar to the mean orbital volume of 24.60 ± 2.68 cc. obtained from a sample of 54 Asian people and 22.8 ± 2.16 cc, obtained from 20 Taiwanese people; both performed by tomographic methods [14-17].
Genetic similarities exist between indigenous Asian and Native American populations, as demonstrated by L. Cavalli Sforza [3]. Who based on hereditary traits, language, and molecular analysis determined that there are lower genetic distances between Native American and Asian races than with others like Europeans and Caucasians. This data is reaffirmed with new studies based solely on genetic analysis which confirm that the Amerindian race and particularly the Quechua and Aymara come from the same trunk of Asian races [18-21]. This similar origin may be the reason for the very similar orbital volumes, but there is still the issue because there are no similarities with the Chilean population. The settlement of indigenous people existed after the arrival of Europeans interbreeding in different degrees throughout the American continent. Thereby, the Candela group (Consortium for the Analysis of the Diversity and Evolution of Latin America) researched the Chilean population and found that their genes are mostly of European ancestries, like the Colombian population. The genes of Native American ancestry dominate throughout the Peruvian territory, being higher in the southern region of the country [22].
The limitation of the study was the small sample size. However, it was bigger than the majority of the previous studies.
Conclusion
This study quantifies the orbital characteristics of Peruvian adults and provides useful parameters to be used during the surgical approach of the orbit. There was no difference between both eyes in the periorbital region and orbital volume in Peruvian skulls. However, measurements of a medial and lateral wall from the left orbital region are smaller than the right side, and volume measurements are similar to findings in previous studies in Asian skulls. This similarity could be explained by the lower differences in genetic traits between Asian and Amerindian (Quechua-Aymara) races, in comparison to another, as demonstrated in the studies mentioned above.
Declarations
Conflict of Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Fundings
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical Statement
Not applicable, no patients were involved in the study.
Acknowledgment
Thanks to the doctors responsible for the Academic Department of Morphological Sciences of the National University of San Marcos, for the accessibility to the skulls, corresponding to the Anatomy Amphitheater.
References
- Abed, Saif F., et al. "A cadaveric study of ethmoidal foramina variation and its surgical significance in Caucasians." British journal of ophthalmology, Vol. 96, No. 1, 2012, pp. 118-21.
Google Scholar Crossref - Ashwini, L. S., et al. "Morphological and morphometric analysis of supraorbital foramen and supraorbital notch: a study on dry human skulls." Oman medical journal, Vol. 27, No. 2, 2012, p. 129.
Google Scholar Crossref - Cavalli-Sforza, Luigi Luca. "Genes, pueblos y lenguas." Investigación y ciencia, Vol. 184, 1992, pp. 4-11.
Google Scholar - Clauser, Luigi, et al. "Posttraumatic enophthalmos: etiology, principles of reconstruction, and correction." Journal of Craniofacial Surgery, Vol. 19, No. 2, 2008, pp. 351-59.
Google Scholar Crossref - Coronado, César, et al. "Estimación del Volumen Orbitario Mediante Imágenes de TC y el Principio de Cavalieri." Revista chilena de radiología, Vol. 16, No. 2, 2010, pp. 59-63.
Google Scholar Crossref - Evans, B. T., and A. A. C. Webb. "Post-traumatic orbital reconstruction: anatomical landmarks and the concept of the deep orbit." British Journal of Oral and Maxillofacial Surgery, Vol. 45, No. 3, 2007, pp. 183-89.
Google Scholar Crossref - Golusiński, Wojciech, et al. "Endoscopic decompresion of orbital cavity in the course of the Graves' ophthalmopathy." Otolaryngologia Polska= The Polish Otolaryngology, Vol. 62, No. 5, 2008, pp. 587-92.
Google Scholar Crossref - Gosavi, Shilpa N., Surekha D. Jadhav, and Balbhim R. Zambare. "Orbital Morphology With Reference To Bony Landmarks. 20 La morfología de la órbita en relación a los parámetros óseos." Revista Argentina de Anatomía Clínica, Vol. 6, No. 1, 2014, pp. 20-25.
Google Scholar Crossref - Jansen, Jesper, et al. "Orbital volume analysis: validation of a semi-automatic software segmentation method." International Journal of computer assisted radiology and surgery, Vol. 11, No. 1, 2016, pp. 11-18.
Google Scholar - Ji, Yongrong, et al. "Quantitative morphometry of the orbit in Chinese adults based on a three‐dimensional reconstruction method." Journal of Anatomy, Vol. 217, No. 5, 2010, pp. 501-06.
Google Scholar Crossref - Karakaş, P., M. Bozkır, and O. Z. K. A. N. Oguz. "Morphometric measurements from various reference points in the orbit of male Caucasians." Surgical and Radiologic Anatomy, Vol. 24, No. 6, 2002, pp. 358-62.
Google Scholar - Koppel, David Andrew, et al. "The reliability of “Analyze” software in measuring orbital volume utilizing CT-derived data." Journal of Cranio-Maxillofacial Surgery, Vol. 31, No. 2, 2003, pp. 88-91.
Google Scholar Crossref - Lopes, P. T. C., et al. "Morphometric analysis of the infraorbital foramen related to gender and laterality in dry skulls of adult individuals in southern Brazil." Journal of Morphological Sciences, Vol. 26, No. 1, 2017.
Google Scholar Crossref - Miloro, Michael, et al. "Peterson's principles of oral and maxillofacial surgery." Vol. 1. Hamilton: BC Decker, 2004.
Google Scholar - Osaki, Tammy H., et al. "Comparison of methodologies in volumetric orbitometry." Ophthalmic Plastic & Reconstructive Surgery, Vol. 29, No. 6, 2013, pp. 431-36.
Google Scholar Crossref - Kuhn, Ferenc, et al. "The Ocular Trauma Score (OTS)." Ophthalmology Clinics of North America, Vol. 15, No. 2, 2002, pp. 163-5.
Google Scholar Crossref - Reich, David, et al. "Erratum: Reconstructing Native American population history (Nature (2012) 488 (370-374." Nature, 2012, p. 288.
Google Scholar Crossref - Ruiz-Linares, Andrés, et al. "Admixture in Latin America: geographic structure, phenotypic diversity and self-perception of ancestry based on 7,342 individuals." PLoS genetics, Vol. 10, No. 9, 2014.
Google Scholar Crossref - Sharma, Nidhi, et al. "Supraorbital foramen-Morphometric study and clinical implications in adult Indian skulls." Acta Medica International, Vol. 1, No. 1, 2014, p. 6.
Google Scholar - Shyu, Victor B., et al. "3D-assisted quantitative assessment of orbital volume using an open-source software platform in a Taiwanese population." PLoS One, Vol. 10, No. 3, 2015.
Google Scholar Crossref - Singh, Rajani. "Morphometric analysis of infraorbital foramen in Indian dry skulls." Anatomy & cell biology, Vol. 44, No. 1, 2011, pp. 79-83.
Google Scholar Crossref - Thanasil Huanmanop, M. D., M. D. Sithiporn Agthong, and M. D. Vilai Chentanez. "Surgical anatomy of fissures and foramina in the orbits of Thai adults." Journal of The Medical Association of Thailand, Vol. 90, No. 11, 2007, pp. 2383-91.
Google Scholar