Research Article - International Journal of Medical Research & Health Sciences ( 2022) Volume 11, Issue 7
Management and Maxillofacial Rehabilitation of COVID-19 Associated Mucormycosis
Aishwarya Chatterjee*Aishwarya Chatterjee, Department of Surgical Oncology, University of Rajasthan, Jaipur, Rajasthan, India, Email: smiledoctor32@gmail.com
Received: 26-May-2022, Manuscript No. ijmrhs-22-65026; Editor assigned: 30-May-2022, Pre QC No. ijmrhs-22-65026(PQ); Reviewed: 13-Jun-2022, QC No. ijmrhs-22-65026; Revised: 25-Jul-2022, Manuscript No. ijmrhs-22-65026(R); Published: 08-Aug-2022, DOI: O
Abstract
Objectives: To study and present a management protocol formulated to treat coronavirus disease associated invasive fungal sinusitis (mucormycosis) (CAM) and related defects.
Methods: A prospective interventional study was conducted at a tertiary care center over three months, involving patients with mucormycosis of the paranasal sinuses suffering from or having a history of coronavirus disease infection (COVID-19) who underwent debridement surgery. A protocol was formulated incorporating all the departments involved for management of post COVID-19 associated mucormycosis (CAM) patients. A separate protocol for early prosthetic rehabilitation was also developed.
Results: Twenty patients underwent surgical and medical intervention along with prosthetic rehabilitation for CAM. All of the patients were post COVID-19 infected who had developed acute symptoms. The maxillary sinus was affected in all these patients and 25% of the patients had involvement of the orbit along with the maxillary sinus. All patients had been administered steroid during the treatment for COVID-19 associated illness. Infrastructure maxillectomy of the right side was done in 35% of patients, bilateral maxillectomy was done in 30% of patients, and two patients underwent infrastructure maxillectomy and orbital exenteration of right side. Six patients received surgical obturator inserted on second day post-maxillectomy, 8 patients received intermediate obturator inserted on the 10th-12th day post-maxillectomy and 6 patients received silicone obturator inserted on 14th-18th day after bilateral maxillectomy.
Conclusion: early management, prompt treatment and post-operative comprehensive rehabilitation towards an optimum Quality Of Life (QOL) can be achieved for good prognosis in patients affected by CAM. The prosthetic rehabilitation protocol provided prosthesis earlier and faster to the patients that improved their QOL.
Keywords
Coronavirus associated mucormycosis, Mucormycosis, COVID-19, Maxillofacial prosthesis, Silicone prosthesis, Obturator
Introduction
The etiologic factor for Coronavirus disease (COVID-19) is the novel beta coronavirus named Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) [1]. As on 18 April 2021, COVID-19 status in India reports 1801316 active cases, an increase of 12.18 % [2]. This is an unprecedented second wave that the country is experiencing. Among several treatment options for management of COVID-19 is the use of systemic steroids with or without anti-viral medication. However, use of high dose glucocorticoids for long duration may lead to increased susceptibility to bacterial and fungal infections [3-5]. Pulmonary aspergillosis complicating COVID-19 recovery has been reported while mucormycosis more rarely so [6].
The combination of uncontrolled diabetes mellitus, administration of steroid and COVID-19 infection is ideal breeding grounds for fungal spore.
Acute rhino-Orbito-cerebral mucormycosis is often a fatal disease [7] with mortality rates ranging between 40-80% in uncontrolled diabetes. In the back drop of long ICU stays with compromised immunity, the burden of mucormycosis infection as post COVID sepsis is high in India [8]. In a post-mortem study of 10 patients, among other pathological processes, secondary disseminated mucormycosis was reported as a novel finding as early as March-April 2020 [9]. A systematic review reported 82 cases of CAM from India, 9 cases from USA, 3 cases from Iran and 19 cases from other parts of the world [10].
A protocol was formulated by specialties to manage cases of acute fungal rhino sinusitis, presenting as post COVID-19 sepsis. In this prospective interventional study we discuss in detail about patients with COVID-19 Associated Mucormycosis (CAM) and palatal involvement here in the Indian setting.
Materials and Methods
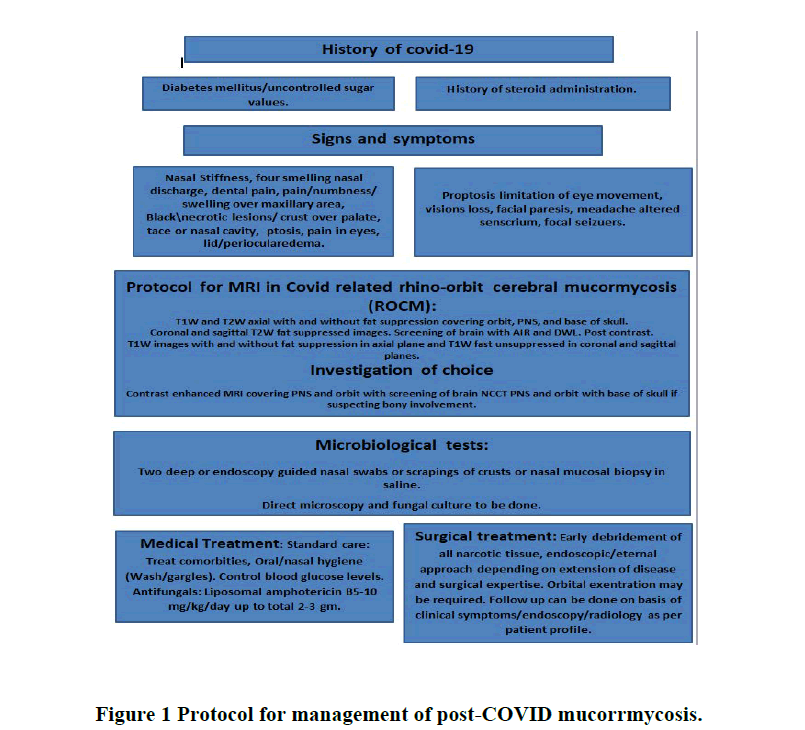
Protocols for management of suspected post COVID-19 Associated Mucormycosis (CAM) patients were formulated by a group consisting of several specialties: Ear Nose Throat (ENT), ophthalmology, medicine, endocrinology, neurology, neurosurgery, radio diagnosis, dental and prosthetic surgery, microbiology and pathology (Figure 1).
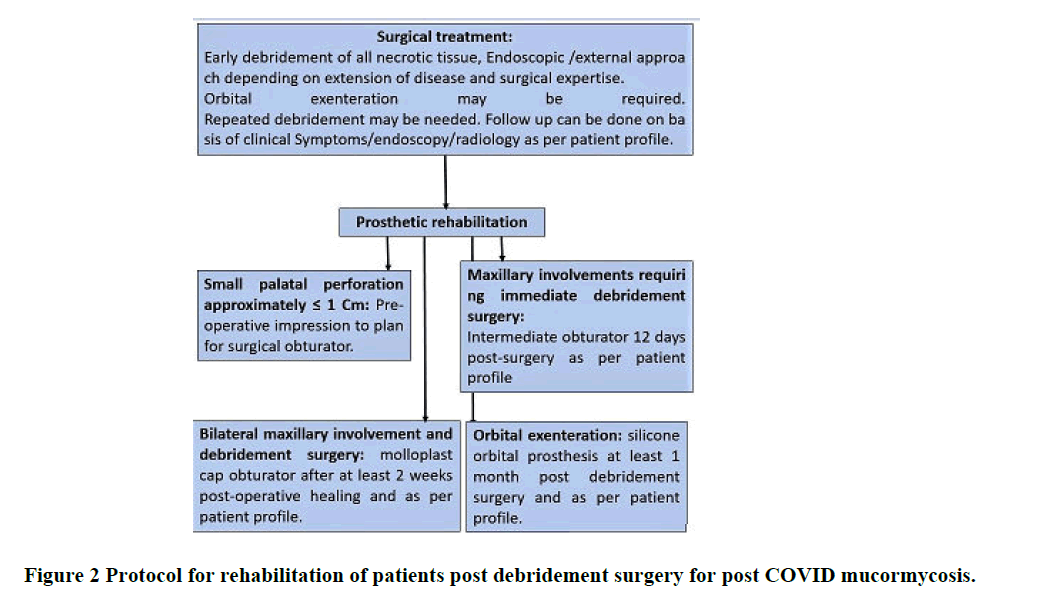
Details of patients suspected of CAM over a period of three months from April 2021 to June 2021 were included in this prospective interventional study. Patients' demographic data, hospitalization records, history of comorbidities, past history of COVID-19 infection, history of steroid administration and duration, medical and surgical intervention and rehabilitation details were recorded. Patients with needs for prosthesis were rehabilitated according to the protocol formulated (Figure 2).
Statistical analysis: Information of demographics, management, intervention and rehabilitation of patient satisfying these guidelines was gathered. Data was subjected to statistical analysis using Statistical package for social sciences (SPSS v 26.0, IBM, USA).
Result
A total of 20 patients underwent surgical and medical intervention along with prosthetic rehabilitation for CAM. Majority of the patients were male with mean age of 54.75 years with a range of 42 to 78 years. All of the patients were post COVID-19 infected who had developed acute symptoms as listed in (Figure 1). The mean duration of COVID-19 infection was 13.75 days.
The chief complaint of majority of the patients at presentation was swelling and pain in the affected side of the face. 60% of patients did not give any history of pre-existing Diabetes Mellitus (DM), 30% gave a history of type II DM and 10 % were not aware of their diabetes status. The maxillary sinus was affected in all these patients and 25% of the patients had involvement of the orbit along with the maxillary sinus. At the time of presentation 45% of the patients had DM, 15% had both hypertension and DM, 15% had hypertension, one patient had dengue and DM and one patient had liver disease as comorbidities. No comorbidity was seen associated in 15 % of the patients. All patients had been administered steroid during the treatment for COVID-19 associated illness. Dexamethasone was administered to 45% of the patients, 30 % received methylprednisolone, 5% received both dexamethasone and methylprednisolone and 10% were not aware of administration of steroid. However 10% of the patients did not receive any steroid. The duration of steroid administration. The maximum duration was 12 days and minimum duration was 4 days in these patients. Of the 20 patients, 11 were hospitalized and 9 were under home quarantine. The mean duration of hospitalization or home quarantine was 11.15 days.
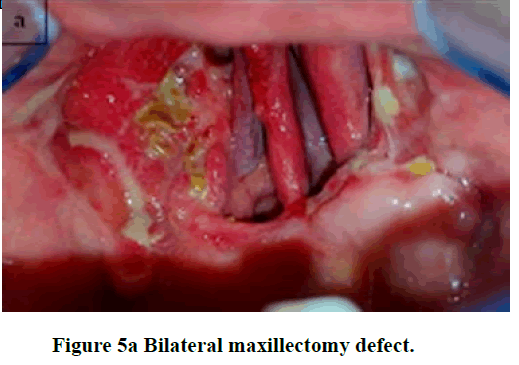
Aggressive medical and surgical intervention was initiated. Radical surgical debridement of affected soft and hard tissue, till healthy viable tissue is encountered was done in all the patients. Infrastructure maxillectomy of the right side was done in 35% of patients and bilateral maxillectomy was done in 30% of patients. Only 2 patients underwent infrastructure maxillectomy and orbital exenteration of right side. Amphotericin B was started as per protocol and under physician supervision.
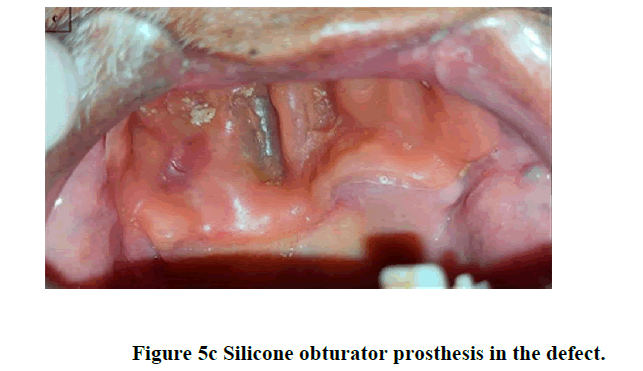
The main aim after debridement surgery in this group of patients was to improve nutrition and start oral intake as early as possible. A protocol was formulated (Figure 2) to address this requirement. Rehabilitation with obturator prosthesis was planned. All the obturator prosthesis was removable in nature. Impression was made in irreversible hydrocolloid (Imprint, DPI) impression material. The impressions were poured with improved dental stone. In cases where the contralateral arch had considerable number of teeth, retention was obtained from the defect as well as by adapting 21 gauge stainless steel orthodontic wire around these teeth in the stone model obtained after impression. Autopolymerising resin (RR cold cure, DPI) was used to fabricate the obturator prosthesis. After curing the prosthesis was finished and polished following standard laboratory protocol. There were few cases in which bilateral maxillectomy were done. Primary impression was taken with irreversible hydrocolloid (Imprint, DPI) and model was fabricated in dental plaster (Plaster of Paris, Neelkanth). A custom tray was fabricated out of autopolymerising resin (RR cold cure, DPI). Border moulding was done out of green stick tracing compound (Pinnacle tracing sticks, DPI) and a secondary impression made with addition silicone medium viscosity (Aquasil Monophase, Dentsply) tray material after adequately blocking the defect. The master cast was made out of improved dental stone (Kalstone, Kalabhai). Modelling wax (Modeling wax, PDP) was adapted in to the defect. Standard laboratory procedures were followed, dewaxing was done and the mould obtained. Heat curing silicone (Molloplast B, Detax) was packed in the mould and standard curing steps were followed. The silicone obturator obtained was trimmed off excess and inserted in the defect. All the patients were trained on how to use the obturator. Instructions on its hygiene and maintenance were given.
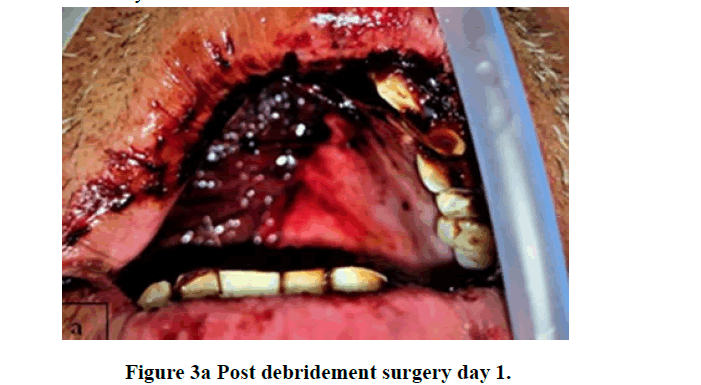
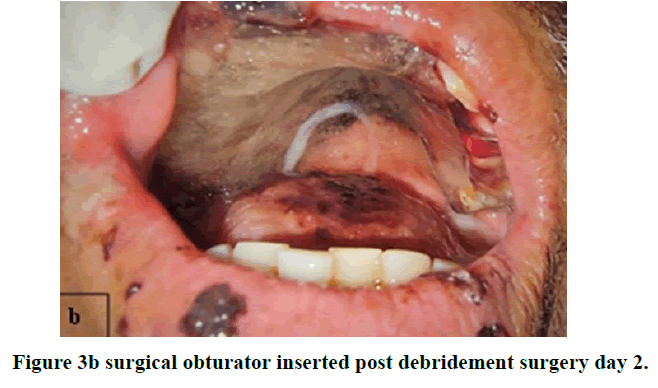
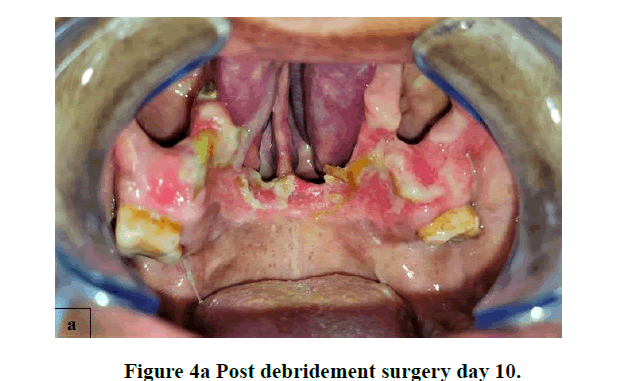
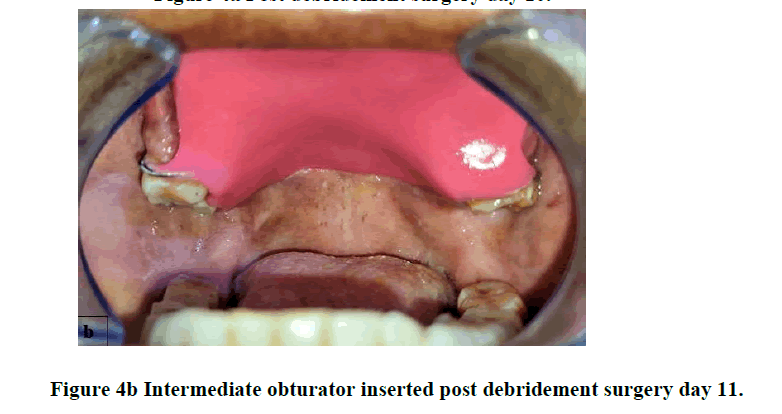
Of the 20 patients six patients received surgical obturator which were inserted on second day post-maxillectomy, 8 received intermediate obturator inserted on the 10th-12th day post-maxillectomy and 6 patients received silicone obturator inserted on 14th-18th day after bilateral maxillectomy (Figure 3a,b). Individual care and rehabilitation could be done after triage according to the rehabilitation protocol adopted by us (Figure 4a,b). Intraoral rehabilitation with obturator enabled return to early oral intake.
Discussion
This study demonstrated the management and maxillofacial rehabilitation of patients diagnosed with mucormycosis as a complication of severe to moderate COVID-19 infections. Mucormycosis is an opportunistic infection of fungal origin mainly affecting immunocompromised and debilitated patient [6-11]. CAM is only emerging now as a new entity in different parts of the world [4].
Critically ill patients with prolonged hospitalization requiring stay in ICU/mechanical ventilation, multiple comorbidities and use of corticosteroids are more likely to develop fungal infection. It is also believed that the fungal infection may develop during the middle and later stages of COVID-19 disease specially gravely ill ones [12,3,4]. It has been postulated that triad of pre-existing or unknown DM, COVID-19 infection and high dose corticosteroid use initiates a cascade which increases the likelihood of contracting opportunistic fungal infection [10]. However in this study it was seen that some of the patients were under treatment at home quarantine after contracting COVID-19 infection. All patients developed mucormycosis after they had tested negative for COVID-19 infection.
The usual mode of entry is by inhalation of fungal spores through nose. It then invades the blood vessels causing thrombosis and eventually necrosis hence referred to as angio-invasive fungi. Most common form is the rhinomaxillary variant, involvement of the sphenopalatine and greater palatine artery leads to avascular necrosis of the maxilla. Disease may even spread to orbit and cranium [11]. That is why it must be recognized early and treatment started promptly to avoid morbidity and mortality [6-13]. As compared to a previous study [14], all our cases had rhinomaxillary involvement with some showing spread to orbit.
Pain and swelling in the maxillary dentition was the chief complaint in most of our cases. First investigation of choice is usually Non-Contrast Computed Tomography (NCCT) of the paranasal sinuses [15]. If intra-orbital or intracranial extension is suspected, gadolinium-enhanced magnetic resonance imaging is resorted to. Focal bony erosions and extra-sinus spread with erosion of the maxillary sinus walls are strongly suggestive of the diagnosis [13,14]. This was instituted in our protocol for early diagnosis of suspected CAM at the outset. It has been reported that MRI is more sensitive than a CT scan in detecting fungal sinusitis [13,6].
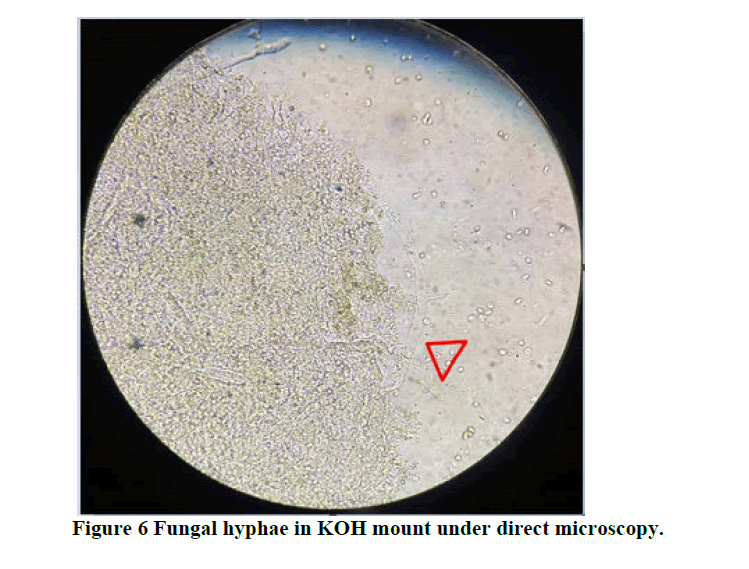
Microbiologic and histopathologic confirmation of fungal spores and hyphae is diagnostic of the type of fungus. If a potential diagnosis of CAM was made based on imaging, as per recommendations and guidelines a biopsy specimen was obtained by endoscopy. Direct microscopic evidence of fungal hyphae in Potassium Hydroxide (KOH) mounts was confirmatory of mucormycosis (Figure 5a,b,c).
There is strong recommendation for early surgical treatment for mucormycosis. Surgery alone is not curative but provides disease control and for histopathological confirmation. Repeat debridement or resection need to be done as required [13,14]. Post-surgical treatment first line antifungal therapy with liposomal Amphotericin B, 5-10 mg/kg per day need to be started immediately. There is marginal to moderate recommendation for Posaconazole oral suspension and delayed release tablet as a suitable alternate treatment [13]. Mortality rates range from 40% to 80%.
High mortality rates (>80%) are reported in cases with disseminated disease or intracranial involvement. Lower mortality is reported when early tissue-based diagnosis is feasible and surgical debridement is done [13,7]. It is worthy to note that though 25% of patient had orbital involvement, 10% underwent exenteration highlighting the effort to save the orbit and associated structures at all cost.
Radical surgery initiated early may salvage and stabilize the patient. However, it will lead to a complex oro-nasoorbital defect [16]. There are various options aimed at reconstruction of these defects. In the early stages surgical reconstruction will be risky as repeated debridement is required and associated comorbidities need to be managed first. The main aim post debridement surgery is to start oral intake as early as possible to improve the nutritional requirements of these patients. Obturator prosthesis is suitable in this situation, as it is removable, rapid alternative to reconstruction, non-invasive, easy to manipulate, easier hygiene maintenance and economical [17].
A number of obturator designs have been reported in the literature for rehabilitation of patients affected by mucormycosis [18]. In our study surgical and intermediate obturator were used for rehabilitation of CAM cases postmaxillectomy. Silicone obturator was used in cases with bilateral maxillectomy (Figure 6). The mode of retention for surgical and intermediate obturator were from the remaining dentition, whereas, for bilateral maxillectomy cases retention was obtained from anatomical undercuts selectively recorded during the impression procedure. Though Osseointegrated dental implants or zygomatic implants could have been used for retention of the obturator, however conventional mode was adopted as surveillance of the defect was of priority and any invasive procedure was postponed till complete remission of fungal infection and healing.
A number of case reports and reviews are present describing CAM. Our data from a tertiary care teaching institute is a first comprehensive ongoing experience of CAM involving the palate over the past three months. All 20 patients have received comprehensive treatment involving various specialties for CAM. They had completed two months follow-up at the end of the study period. All patients had started oral feed and there was improvement in quality of life of the patients. To the best of our knowledge this is a first that a protocol for early rehabilitation of these patients was put in place. There were no mortalities.
Conclusion
Among the still evolving long term effects of COVID-19 infection, CAM is dangerous. It must be given immediate and serious attention. As the probable causal factors of uncontrolled diabetes and steroid use have been identified, multiple specialty approach to its treatment should be sought for early management. Post-operative comprehensive rehabilitation towards an optimum quality of life can be achieved for good prognosis in patients affected by CAM.
References
- Sharma D, et al. To Study the Role of Absolute Lymphocyte Count and RDW in COVID 19 Patients and their Association with Appearance of Symptoms and Severity. The Journal of the Association of Physicians of India, Vol. 68, No. 8, 2020, pp. 39-42.
- Garg D, et al Coronavirus Disease (COVID-19) Associated Mucormycosis (CAM): Case Report and Systematic Review of Literature. Mycopathologia, Vol. 186, No. 2, 2021, pp. 289-298.
- Nasir N, et al. COVID-19 Associated Pulmonary Aspergillosis (CAPA) in patients admitted with severe COVID-19 pneumonia: An observational study from Pakistan. Mycoses, Vol. 63, No. 8, 2020, pp. 766-770.
- Werthman-Ehrenreich A. Mucormycosis with orbital compartment syndrome in a patient with COVID-19. The American Journal of Emergency Medicine, Vol. 42, 2021, pp. 264-265.
- Mekonnen ZK, Ashraf DC and Jankowski T. Acute Invasive Rhino-Orbital Mucormycosis in a Patient with COVID-19-Associated Acute Respiratory Distress Syndrome. Ophthalmic Plastic and Reconstructive Surgery, Vol. 37, No. 2, 2021, pp.e40-e80.
- Soman R and Sunavala A. Post COVID-19 Mucormycosis from the Frying Pan into the Fire. The Journal of the Association of Physicians of India, Vol. 69, No. 1, 2021, pp. 13-14.
- Hanley B, et al. Histopathological findings and viral tropism in UK patients with severe fatal COVID-19: a post-mortem study. The Lancet Microbe, Vol. 1, No. 6, 2020, pp. e245-e253.
- Singh AK, et al. Mucormycosis in COVID-19: A systematic review of cases reported worldwide and in India. Diabetes and Metabolic Syndrome: Clinical Research and Reviews, Vol. 15, No. 4, 2021, pp. 102146.
- Mengji AK, et al. Mucormycosis in a surgical defect masquerading as osteomyelitis: a case report and review of literature. Pan African Medical Journal, Vol. 23, No. 1, 2016, pp. 16.
- Song G, Liang G and Liu W. Fungal Co-infections Associated with Global COVID-19 Pandemic: A Clinical and Diagnostic Perspective from China. Mycopathologia, Vol. 185, No. 4, 2020, pp. 599-606.
- Cornely OA, et al. Global guideline for the diagnosis and management of mucormycosis: an initiative of the European Confederation of Medical Mycology in cooperation with the Mycoses Study Group Education and Research Consortium. The Lancet Infectious Diseases, Vol. 19, No. 12, 2019, pp. e405-e421.
- Sharma S, et al. Post coronavirus disease mucormycosis: a deadly addition to the pandemic spectrum. The Journal of Laryngology and Otology, Vol. 135, No. 5, 2021, pp.442-447.
- Deshpande SN, et al. Prosthetic rehabilitation of face following naso-orbital mycosis. Indian Journal of Plastic Surgery, Vol. 39, No. 1, 2006, pp. 73-75.
- Dholam KP, Sadashiva KM and Bhirangi PP. Rehabilitation of large maxillary defect with two-piece maxillary obturators. Journal of Cancer Research and Therapeutics,Vol. 11, No. 3, 2015, pp. 664.
- Mani UM, et al. A modified technique to fabricate a complete hollow obturator for bilateral maxillectomy in a patient with mucormycosis- A technical case report. Special Care in Dentistry, 2019, pp. 1-7.
- Naveen S, et al. Mucormycosis of the Palate and its Post-Surgical Management: A Case Report. Journal of International Oral Health, Vol. 7, No. 12, 2015, pp. 134-137.
- Shah RJ, et al. Prosthetic Rehabilitation of Acquired Maxillary Defects Secondary to Mucormycosis: Clinical Cases. The Journal of Contemporary Dental Practice, Vol. 15, No. 2, 2014, pp. 242-249.
- Mehta S and Pandey A. Rhino-Orbital Mucormycosis Associated With COVID-19. Cureus, Vol. 12, No. 9, 2020, pp. e10726.