Research Article - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 8
Knowledge, Attitude and Practice of Occupational Radiation Safety among Physicians in Saudi Arabia
Abdulmonem Alsiddiky, Nouf Alabdulkarim*, Nouf Altwaijri, Waleed Awwad and Khalid BakarmanNouf Alabdulkarim, Department of Orthopedics, College of Medicine, King Saud University, Riyadh, Saudi Arabia, Email: Noufhalabdulkarim@gmail.com
Received: 26-Jul-2021 Accepted Date: Aug 24, 2021 ; Published: 31-Aug-2021
Abstract
Background: Despite its advantages, ionizing radiation causes adverse reactions on living organisms. To apply protective measures, physicians must minimize the time of exposure as possible, maximize their distance from the radiation source and wear protective gear. This study aimed to understand the level of awareness, knowledge, and safe practice of radiology among physicians in different specialities within the medical field. Methods and Material: A cross-sectional study was conducted in Riyadh, Saudi Arabia. Physicians in several specialities, medical and surgical, of different levels of experience, were included, and physicians without a medical license were excluded. A 16-item self-administered questionnaire measuring physicians’ knowledge, attitude, and exposure to radiation and radiation safety. Results: One hundred and thirty-five physicians were included in the study; the mean of the years of experience for those physicians was 10.79 years. Only 23% of participants have undergone radiation safety training. The physicians’ measured total knowledge, attitudes, and practice scores showed that the physician’s overall mean knowledge score on radiology safety was 51.5%, which is relatively low. The physician’s attitudes toward radiological safety converged significantly and positively on their good safety practices total score. Conclusions: Knowledge is very deficient when it comes to radiation safety, therefore, departmental education sessions concerning specific gaps of knowledge must be implemented for the betterment of knowledge and practice as they positively correlate. Physicians have a good attitude towards radiation safety but are found to be non-compliant more often than not.
Keywords
Attitude, Radiography, Radiation safety, Occupational safety, Occupational hazards
Introduction
X-ray imaging was first discovered in the late 1800s [1]. It was and still is one of the most important leaps in medicine. The application of X-rays and other types of ionizing radiation in medicine is advancing in the process of diagnosis of illnesses and lately in therapeutic practices too [1-3].
Radiation is classified into ionizing and nonionizing. Despite its unquestionable advantages, ionizing radiation causes adverse reactions on living organisms. Ionizing radiation begins with the separation of an electron from an atom or a molecule releasing free radicals, which are hyperactive and chemically unstable [3]. There are mainly two types of radiation effects: deterministic effects concerning higher doses and stochastic effects which are associated with lower doses [4,5]. Before any research was conducted on the effects of radiation, it was reported that workers who were exposed to massive amounts of radiation had suffered from dermatosis, haematological disorders, cataracts, and different types of cancers [1].
The Center for Disease Control and Prevention has ALARA (As Low As Reasonably Possible) as the guiding principle for radiation safety. ALARA is achieved by utilizing three basic protective measures: time, distance, and shielding. To apply these protective measures, people that deal with radiation must minimize the time of exposure as much as possible, maximize their distance from radiation sources and use protective gear [6].
Understanding the principles of radiation safety and how to effectively apply them is critical.
Occupational radiation has always posed concerns of causing harmful effects on the future children of the worker [7,8]. A significant correlation was noted between the occupational exposure of workers in the Sellafield nuclear plant and the higher incidence of congenital anomalies or leukemias in their children [7,9,10].
Multiple studies from all around the world aimed to evaluate the knowledge level of physicians regarding the effects of radiation [11-15]. It was found that radiation safety knowledge is deficient in operative rooms staff and, surprisingly, more deficient in radiologists [16-19]. In Saudi Arabia, underestimation of radiation effects amongst pediatricians was recognized [20]. We are conducting this study to understand the level of awareness, knowledge, and safe practice of occupational radiation exposure among physicians in different specialities within the medical field. As noted above, knowledge and awareness are quite limited in many specialities. Therefore, we want to understand our medical community’s level of knowledge, awareness, and safe practice to improve occupational safety.
Materials and Methods
A cross-sectional study was conducted from January 2020 to March 2020. Including authorized physicians in all specialities, excluding non-authorized physicians. A total of 135 physicians responded and completed the questionnaire. We used an English 16-item online questionnaire adapted from Abdellah, et al. which measures physicians’ knowledge, attitude, and exposure to radiation and radiation safety [11]. Approval was obtained from the Institutional Review Board in King Saud University, Riyadh, Saudi Arabia (Approval No. E-20-4618). Informed consent was obtained; all the participants were informed about the purpose of the study and their right to withdraw at any time without any obligation towards the study team. Also, no incentives or rewards were given.
Statistical Analysis
Means and standard deviations were used to describe continuous variables. Moreover, categorically measured variables were described with frequencies and percentages. The statistical assumption of normality for the continuous variables was assessed using the Kolmogorov-Smirnove test and the visual Histograms; Levene’s test of equal variance was used for testing the homogeneity of variance statistical assumptions for measured concepts and continuous variables. Independent samples t-test and one-way ANOVA tests were used to assess the statistical significance of the mean differences on the participant’s “knowledge of radiology safety score.” The Bi-variate Pearson’s correlation (r) test was used to assess the associations between metric variables. The compute command in the analysis program was used to comprise the composite total score for their attitudes toward radiology safety. The exploratory factor analysis procedure was used to assess the factorial validity and the factor structure of all the measured concepts and their reliability was assessed with the Cronbach’s (α) alpha test of internal consistency. Statistical Package for the Social Sciences (SPSS IBM V21) was used for the data analysis, EXCEL program was used for creating figures and depictions. Alpha significance level was considered at 0.050 level.
Results
One hundred and thirty-five participants were included in the study. The resulted data analysis findings for the sociodemographic characteristics are displayed in Table 1. 77.8% of the responding participants were males. The distribution of the participant’s age groups showed that 37% were aged between 20-30 years, 25.2% were aged between 31-40 years, 21.5% were aged between 41-50 years, and the remainder of the 16.3% were aged ≥ 51 years. 79.3% of the participants reside in Riyadh, the capital city of Saudi Arabia. With regards to the participant’s speciality, 55.6% of participants were orthopaedic surgeons, 4.4% were specialized in neurosurgery, 5.9% specialized in Radiology. The mean ± SD years of experience for the participants were 10.79 years, SD=9.51 years; however, the analysis of the categorized experience years indicated that 30.4% had 1-4 years of experience, 20.7% had 5-8 years, 24.4% had 9-15 years and 24.4% had ≥ 16 years. When it came to radiation safety training, only 23% of participants have undergone radiation safety training, whereas most have not been trained. In addition, participants were asked to indicate the number of radiation safety articles they read per week, 48.9% read none, 20% read one article/week, 23% read between 2-5 articles per week, and the remainder 8.1% read >5 articles per week.
| Frequency | Percentage | |
|---|---|---|
| Gender | ||
| Female | 30 | 22.2 |
| Male | 105 | 77.8 |
| Age groups | ||
| 20-30 | 50 | 37 |
| 31-40 | 34 | 25.2 |
| 41-50 | 29 | 21.5 |
| ≥ 51 | 22 | 16.3 |
| City of Residence | ||
| Riyadh | 107 | 79.3 |
| Outside Riyadh | 28 | 20.7 |
| Physicians Rank | ||
| Medical Student | 36 | 26.7 |
| Intern/Resident | 17 | 12.6 |
| Fellow/Registrar | 24 | 17.8 |
| Consultant | 58 | 43 |
| Seniority | ||
| Junior | 52 | 38.5 |
| Senior | 83 | 61.5 |
| Speciality | ||
| Medical student | 39 | 28.9 |
| Orthopedics/surgery | 75 | 55.6 |
| Neurosurgery | 6 | 4.4 |
| Radiology | 8 | 5.9 |
| Other specialities | 7 | 5.2 |
| Experience years, mean (SD) | 10.79 (9.51) | |
| Experience years groups | ||
| 1-4 | 41 | 30.4 |
| 5-8 | 28 | 20.7 |
| 9-15 | 33 | 24.4 |
| ≥16 | 33 | 24.4 |
| Did you take any radiation safety training? | ||
| No | 104 | 77 |
| Yes | 31 | 23 |
| How many medical articles about radiation safety do you read/week? | ||
| None | 66 | 48.9 |
| One/week | 27 | 20 |
| 2-5/week | 31 | 23 |
| >5/week | 11 | 8.1 |
Table 2 displays the findings for physicians’ practice and radiation exposure. We found that 26.7% do not get exposed to radiation at any time during work, 17.8% get exposed once or less per week, 31.9% get exposed 1-3 times per week and 23.7% get exposed more than three times per week. Subsequently, participants were asked to indicate how far from an X-ray field do they stand without any protection during a radiologically guided procedure, 3% do not care about radiation, 3% stand 1 meter away, 38.5% stand at least 2 meters away, and 14.1% stand 5 meters away from the ongoing radiological procedure/device. Nevertheless, 41.5% of physicians noted that they work within the operation room in general. Participants were asked to indicate how much radiation, in milli-sieverts (mSv), is a person exposed on average per year from natural exposure to radiations, 75.6% noted that they do not know, 8.1% answered 0.24 mSv/year, 12.6% believed the annual exposure was 2.4 mSv/year and were correct, 2.2% answered 24 mSV/year. Moreover, participants were asked to indicate the approximate radiation dose, in (mSv), of a chest x-ray, the findings showed that only 14.8% had correctly answered 0.2 mSv whereas 68.9% did not know the amounts, 9.6% answered 0.02 mSv, 3% answered 2 mSv and 3.7% answered 20 mSv.
| Frequency | Percentage | |
|---|---|---|
| How often do you expose to radiation every week? | ||
| Never | 36 | 26.7 |
| Once or less/week | 24 | 17.8 |
| 1-3 times/week | 43 | 31.9 |
| >3 times per week | 32 | 23.7 |
| How far from the X-ray, do you stand without any protection during the radiological-guided procedure? | ||
| Do Not care about radiation | 4 | 3 |
| 1 Meter | 4 | 3 |
| 2 Meters | 52 | 38.5 |
| 5 Meters | 19 | 14.1 |
| I work in the operating room | 56 | 41.5 |
| How much radiation, in milli-Sieverts (mSV), is a person exposed to, on average, every year, from natural? | ||
| Do Not know | 102 | 75.6 |
| 0.24 mSV | 11 | 8.1 |
| 2.4 mSV | 17 | 12.6 |
| 24 mSV | 3 | 2.2 |
| 240 mSV | 2 | 1.5 |
| What is the approximate radiation dose, in (mSv), of a chest X-ray? | ||
| Do Not Know | 93 | 68.9 |
| 0.02 mSV | 13 | 9.6 |
| 0.2 mSV | 20 | 14.8 |
| 2 mSV | 4 | 3 |
| 20 mSV | 5 | 3.7 |
Table 3 displays the participant’s personal radiological safety precautionary practices and use of personal protective equipment at the workplace. The participants were asked to indicate how frequently they had used each of the personal protective equipment and precautionary measures listed using (Never/Unsure/Often). The results showed that 80% used lead aprons while doing radiological guided procedures and that significantly less than expected numbers of the participants were unsure or had rarely used lead aprons. On the other hand, a substantial proportion of the participants stated that they wear thyroid shields (43.7%). Conversely, 84.4% stated that they do not use leaded gloves, p<0.001. In addition, 80% stated that they do not use eyeglasses while performing radiologically guided procedures, p<0.001. Furthermore, 53.3% stated that they do not use a minimal endoscopic time as a precautionary radiological measure, p<0.001.
| Never/Rarely | Uncertain | Often/always | χ2/df=2 | p-value | |
|---|---|---|---|---|---|
| Lead aprons | 18 (13.3) | 9 (6.7) | 108 (80%) | 133.2 | <0.001 |
| Thyroid shields | 64 (47.4) | 12 (8.9) | 59 (43.7) | 36.58 | <0.001 |
| Leaded gloves | 114 (84.4) | 15 (11.1) | 6 (4.4) | 159.6 | <0.001 |
| Eyeglasses | 108 (80) | 13 (9.6) | 14 (10.4) | 132.31 | <0.001 |
| Minimal endoscopic time | 72 (53.3) | 34 (25.2) | 29 (21.5) | 24.58 | <0.001 |
| Increasing distance from X-ray device | 54 (40) | 14 (10.4) | 67 (49.6) | 33.91 | <0.001 |
The participants were asked to rate four types of radiologically protective equipment PPE’s for efficiency in protecting healthcare workers against physical radiological matter exposure. As displayed in Table 4. A significant proportion of the participants (94.1%) had noted that lead aprons are protective against radiation exposure, p<0.001. Also, a statistically significant number of participants (85.9%) had agreed on the protective ability of thyroid shields. However, a substantive number (35.6%) of participants were uncertain about the protective ability of leaded gloves, p=0.008. In addition, 31.9% were uncertain whether the eyeglasses were radiation protective or not p<0.001.
| Not protective | Uncertain | Protective | χ2/df=2 | p-value | |
|---|---|---|---|---|---|
| Lead aprons | 1 (0.7) | 7 (5.2) | 127 (94.1) | 224.53 | <0.001 |
| Thyroid shields | 10 (7.4) | 9 (6.70 | 116 (85.9) | 168.04 | <0.001 |
| Leaded gloves | 29 (21.6) | 48 (35.6) | 58 (43) | 9.64 | 0.008 |
| Eyeglasses | 19 (14.1) | 43 (31.9) | 73 (54.1) | 32.53 | <0.001 |
To assess the participants’ knowledge of the radiological exposure sensitivity of various body organs, they were asked to rate eight vital body organs for sensitivity to radiative offenders with (1=Not sensitive, 2=Uncertain, and 3=Sensitive) as shown in Table 5. The results showed that 41.5% had correctly agreed on the sensitivity of the human urinary bladder to radiation, 34.1% were uncertain and 24.4% had answered incorrectly. A significantly high number of participants (82.2%) had agreed correctly that the gonads are radiation sensitive. Furthermore, 40% had incorrectly inferred that the kidneys were radiation insensitive, highlight an overall lack of knowledge.
| Not sensitive | Uncertain | Sensitive | χ2/df=2 | p-value | |
|---|---|---|---|---|---|
| Urinary bladder | 33 (24.4) | 46 (34.1) | 56 (41.5) | 5.911 | 0.052 |
| Gonads | 3 (2.2) | 21 (15.6) | 111 (82.2) | 148.8 | <0.001 |
| Kidneys | 54 (40) | 46 (34.1) | 35 (25.9) | 4.04 | 0.132 |
| Skin | 25 (18.5) | 35 (25.9) | 75 (55.6) | 31.11 | <0.001 |
| Central nervous system | 44 (32.6) | 42 (31.1) | 49 (36.3) | 0.578 | 0.749 |
| Bone marrow | 2 (1.5) | 29 (21.6) | 104 (77) | 124.13 | <0.001 |
| Thyroid glands | 1 (0.7) | 15 (11.1) | 119 (88.1) | 184.7 | <0.001 |
| Gastrointestinal tract | 48 (35.6) | 49 (36.3) | 38 (28.1) | 1.644 | 0.439 |
The participants were asked to select the best correct answer to whether if a chest X-ray is counted as a 1 unit, how many units would a patient absorb in different radiological procedures. As displayed in Table 6, the best correct answer to each of these tests is underlined. Of the participants, 34.1% had correctly inferred that abdominal CT scans can be equivalent to 50-300 X-rays, conversely, 23% had incorrectly inferred that the abdominal CT scan equivalence was 10-50 X. A significantly high number of participants 68.1% and 71.1% had correctly answered that the x-ray equivalent in an MRI and US respectively is zero.
| DNK | Zero X | 1-10 X | 10-50 X | 50-300 X | >300 X | Test statistic | p-value | |
|---|---|---|---|---|---|---|---|---|
| Abdominal CT scan | 35 (25.9) | 0 | 0 | 31 (23) | 46 (34.1) | 23 (17) | 8.14 | 0.043 |
| MRI | 32 (23.7) | 92 (68.1) | 4 (3) | 6 (4.4) | 1 (0.70 | 0 | 218.4 | <0.001 |
| US | 39 (28.9) | 96 (71.1) | 0 | 0 | 0 | 0 | 24.1 | <0.001 |
| Radio-nuclide Imaging | 70 (51.9) | 10 (7.4) | 9 (6.7) | 20 (14.8) | 11 (8.1) | 15 (11.1) | 118.73 | <0.001 |
| DNK: I don’t know | ||||||||
The descriptive and relative importance index analyses of the participants’ indicators of attitude towards radiological safety are displayed in Table 7. The top perceived attitude was feeling confident about the steps needed to be taken when caring for patients needing radiation precautions which had received an agreement mean of 2.56/5 and a significantly relative agreement weight, suggesting an overall substantial confidence perceived by those physicians about their skilfulness on radiation precautions.
| Mean (SD) | RII (%) | Rank | |
|---|---|---|---|
| The policies and procedures on radiation precautions are clear and easy to understand | 3.50 (1.01) | 70.1 | 2 |
| I feel confident about the steps I need to take when caring for patients needing radiation precautions | 3.56 (0.99) | 71.1 | 1 |
| I know whom to contact if I have questions about what radiation precautions are needed for a particular patient | 2.79 (1.26) | 55.9 | 9 |
| I feel I can clearly explain the radiation precautions needed to my patients and their visitors | 3.32 (1.03) | 66.4 | 4 |
| I feel safe when caring for patients needing radiation precautions | 3.39 (1.10) | 67.7 | 3 |
| I feel the institutional policies and procedures are based on current regulations | 3.27 (0.98) | 65.5 | 5 |
| I feel confident the institution is carefully monitoring my radiation exposure | 2.81 (1.16) | 56.1 | 8 |
| I feel that I will be called if I received higher than acceptable exposures | 2.94 (1.28) | 58.8 | 7 |
| I feel that working with patients receiving radiation will not affect my ability to have a child | 3.04 (1.10) | 60.9 | 6 |
Table 8 displays the descriptive analysis and descriptive bivariate Pearson’s correlation test between the participants’ measured total knowledge, attitudes, and practice scores. where the Pearson’s (r) test suggested that the physicians’ knowledge and attitude towards radiology safety had correlated positively with their measured good radiology safety practices, r=0.23
| Knowledge | Practice | Attitude | Mean (SD) | |
|---|---|---|---|---|
| Knowledge score on radiology safety 0-18 points score | 1 | 9.27 (3.47) | ||
| Radiology safe practices total 0-7 points score | 0.226** | 1 | 2.48 (1.51) | |
| Attitudes toward radiology safety 9-45 points score | 0.146 | 0.229** | 1 | 28.62 (6.60) |
| **: Correlation is significant at the 0.01 level (2-tailed) | ||||
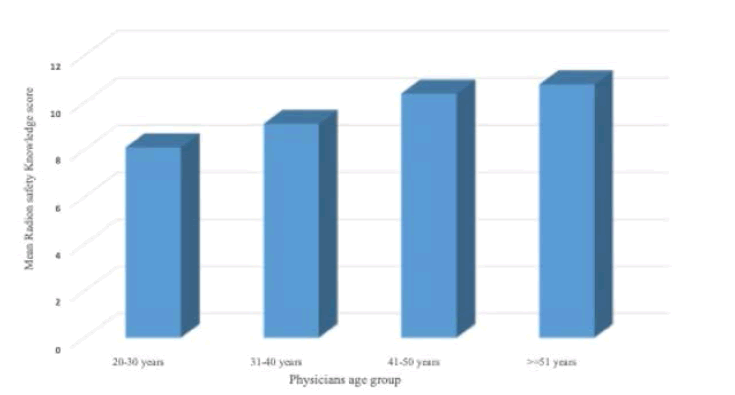
The mean differences in physicians’ knowledge on radiology safety across the levels of their socio-demographic, professional, and working characteristics are displayed in Table 9. Differences were noted across the levels of their age groups, f(3,131)=4.64, p=0.004, (Figure 1). Hochberg’s adjusted posthoc pairwise comparison analysis showed that radiology consultants measured significantly higher mean radiation knowledge than orthopaedic surgeons when pairwise compared, p=0.014.
| Mean (SD)-Physicians Knowledge of Radiology Safety | Test statistic | p-value | |
|---|---|---|---|
| Gender | |||
| Female | 8.30 (3.32) | t(133)=1.76 | 0.081 |
| Male | 9.55 (3.48) | ||
| Age groups | |||
| 20-30 | 8.10 (3.29) | f(3,131)=4.64 | 0.004 |
| 31-40 | 9.10 (3.30) | ||
| 41-50 | 10.38 (3.28) | ||
| ≥ 51 | 10.77 (3.57) | ||
| City of residence | |||
| Riyadh | 9.13 (3.46) | t(133)=0.94 | 0.35 |
| Outside Riyadh | 9.82 (3.53) | ||
| Physicians rank | |||
| Junior | 8.10 (3.20) | t(133)=3.28 | 0.001 |
| Senior | 10.02 (3.43) | ||
| Specialty | |||
| Medical intern | 7.69 (3.60) | f(4,130)=5.93 | <0.001 |
| Orthopedics/surgery | 9.56 (3.33) | ||
| Neurosurgery | 9.17 (3.13) | ||
| Radiology | 13.50 (1.60) | ||
| Other specialties | 10.14 (1.58) | ||
| Experience years groups | |||
| 1-4 | 8.68 (2.88) | f(3,131)=3.38 | 0.02 |
| 5-8 | 8.10 (4.03) | ||
| 9-15 | 9.76 (3.35) | ||
| ≥16 | 10.55 (3.38) | ||
| Did you take any radiation safety training? | |||
| No | 8.93 (3.46) | t(133)=2.12 | 0.036 |
| Yes | 10.42 (3.30) | ||
| How many medical articles about radiation safety do you read/week? | |||
| None | 8.02 (3.54) | f(3,131)=11.10 | <0.001 |
| One/week | 8.89 (2.71) | ||
| 2-5/week | 11.23 (2.84) | ||
| >5/week | 12.27 (2.01) | ||
| How often do you get exposed to radiation every week? | |||
| Never | 8.11 (3.45) | t(133)=2.40 | 0.018 |
| Once or more times/week | 9.70 (3.39) | ||
Discussion
Our results showed that most of our participants had no training in radiation safety, which was similar to other studies [11,21-24]. Given that there is an increasing demand for fluoroscopy, the majority of participants had no safety education or training even though, 25% of the participants in Partap, et al.’s paper use fluoroscopy daily [23,25,26]. Campanella, et al. reported that only about half of the participants had radiation protection training [27]. Sadigh, et al. noted that only 39% of residents had radiation safety discussions every 6 months at least [28]. According to Friedman, et al., approximately half of the urology residents and fellows felt adequately trained in radiation safety [29]. Interestingly, Harris, et al. noted that most of the urology residents had fluoroscopic radiation safety training, either formally, informally, or both, with 46% having radiation safety in their curriculum [30]. Furthermore, most of the literature shows a lack of training in radiation safety, our results support that the physicians, who had training in radiation safety, had significantly higher knowledge than those who had never been trained [31]. Friedman, et al. stated that knowledge on radiation safety improved after departmental education for urology residents [29].
Although our results revealed that knowledge positively correlates with the number of radiation safety articles read per week, 48.9% of our participants do not read about radiation safety. Similarly, most of the participants in Abdellah, et al.’s paper denied reading about radiation safety [11]. Knowledge regarding the sensitivity of different organs to radiation was variable. Most of our participants knew that the gonads, bone marrow, and thyroid are sensitive to radiation; however, knowledge is still lacking when it comes to other organs like the urinary bladder and kidneys. Hamarsheh, et al. as well found that the knowledge regarding the sensitivity of the organs to radiation was lacking [22].
Most of our participants’ knowledge was deficient when it came to radiation exposure from natural background radiation; and the radiation dose of a chest X-ray in (mSv). Abdellah, et al. noted that the lack of knowledge was most evident in background radiation dose; in addition, only 63.8% identified the chest X-ray radiation dose correctly [11]. Sadigh, et al. noted that the residents in their study had limited knowledge about the specific estimated dose effects (e.g., brain malformation during pregnancy, cataracts in personnel, and cancer risk in children); however, most believe there’s a link between exposure to radiation and the development of cancer [28]. Furthermore, many physicians did not know the maximum annual dose recommended [21,29].
In comparison to Abdellah, et al.’s results, variability was noted among the correct equivalence of a chest X-ray to different radiological investigations, except for when it came to ultrasound and MRI, which most participants answered correctly [11]. In addition, a systematic review done by Krille, et al. concluded that physicians had low knowledge concerning the radiation doses and risks of CT scans [32]. Similarly, our results showed that a small number of participants correctly estimated how much a dose of a CT scan is equivalent to units of a chest X-ray. Hamarsheh, et al. examined a similar concept in which the participants were asked to estimate the effective dose for different radiological procedures and found that knowledge was extremely deficient [22].
Our Participants had relatively low knowledge of radiology safety, which is similar to other results [11,21,24,25,28- 31,33-35]. Unsurprisingly, radiology and emergency staff departments had better knowledge of radiation protection than the rest of the medical staff according to Szarmach, et al. [1]. Most of the participants in the Hamarsheh , et al. paper were oblivious to the concept of ALARA, which embodies the basic principles of radiation safety [22]. That opposes the results found by Friedman, et al., where the concept of ALARA was practised by most of the participants [29]. However, knowledge scores correlate significantly and positively with good radiology safety practices, which is similar to Abuzaid, et al., who noted a positive correlation between adherence to safety practices and knowledge on radiation safety [36].
Senior physicians have better knowledge of radiation safety than junior physicians, which is similar to other results in the literature, where Rashid, et al. noted that emergency consultants estimated the doses more accurately than residents and specialists [37]. Our results show that knowledge is fairly affected by speciality, as radiology consultants had better radiation knowledge than orthopaedic surgeons.
The ideal distance between the X-ray field and a person is 2 meters [38]. We found that 41.5% of participants stated that they work within the operation room with the X-ray machine not paying much attention to how far it is from them. However, 38.5% of our participants keep at least 2 meters (6.5 feet) away from the X-ray machine, which demonstrates good practice. Conversely, in a study conducted on dental undergraduate and endodontic postgraduate students, most respondents agreed that the ideal distance between the X-ray field is 2 meters (6.5 ft) [39].
Most of our participants use lead aprons. Friedman, et al. study demonstrated higher compliance with chest and pelvic shields [29]. In addition, a study in Turkey reported that 75.24% of urologists used lead aprons [40]. Only 43.7% of our participants use thyroid shields at all times, in contrast, Friedman, et al. mentioned that 96% of their participants use them [29]. Our results demonstrated that 84.4% and 80% of our participants do not use lead-lined gloves and eyeglasses, respectively. Likewise, Friedman, et al. reported that none of their participants used lead-lined glasses and gloves [29]. The overall mean score of good radiological safety practice measures was 35.4%, which is relatively low. In comparison, the mean good safety practice score was 59.3% in a similar study conducted in Egypt [11].
The participants’ overall attitude toward radiological safety was measured with 63.6% agreement/positive attitude points, which suggests a good attitude toward radiological safety. In comparison, the attitude score in a similar study conducted in Egypt was 46.9% [11]. Moreover, another study in Kashmir reported high attitude scores [41].
This study was limited by the fact that our questionnaire was distributed online; therefore, some participants may have searched for the answers before submitting, which would affect the knowledge score. The availability of PPE might have affected our results. Expanding the study on a larger sample size would better represent our population.
Conclusion
The knowledge is very deficient when it comes to radiation safety, therefore, departmental education sessions concerning specific gaps of knowledge must be implemented for the betterment of knowledge and practice as they positively correlate. Physicians have a good attitude towards the concept of radiation safety but are found to be noncompliant more often than not.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
Ethics Approval and Consent to Participate
Ethical approval was granted by our institutional review board following the National Committee of Bio-Ethics (NCBE) guidelines with the IRB number E-20-4618.
Funding
The authors are grateful to the Deanship of Scientific Research, King Saud University for funding through the Vice Deanship of Scientific Research Chairs.
Authors’ Contributions
Abdulmonem Alsiddiky reviewed the final version of the manuscript, contributed to the study design and manuscript preparation, and performed the literature review and statistical analysis. Nouf Alabdulkarim and Nouf Altwaijri contributed to the study design and manuscript preparation. Waleed Awwad contributed to the manuscript preparation and data collection. All authors read and approved the final manuscript.
Acknowledgements
None.
References
- Szarmach, Arkadiusz, et al. "Radiation safety awareness among medical staff." Polish Journal of Radiology, Vol. 80, 2015, pp. 57-61.
- Shah, Abdul Saeed, et al. "Assessment of radiation protection awareness levels in medical radiation science technologists-A pilot survey." Journal of Postgraduate Medical Institute (Peshawar-Pakistan), Vol. 21, No. 3, 2007.
- Naqvi, S. Tahira S., et al. "Awareness of hazards of X-ray imaging and perception regarding necessary safety measures to be taken during X-ray imaging procedures among patients in public sector tertiary hospitals of Karachi, Pakistan." Cureus, Vol. 11, No. 5, 2019, e4756.
- United Nations Scientific Committee on the Effects of Atomic Radiation. "UNSCEAR 1994 Report: Sources and effects of ionizing radiation." Report to the General Assembly 1 (2010).
- Frigerio, N. A., and R. S. Stowe. "Carcinogenic and genetic hazard from background radiation." Biological and Environmental Effects of Low-Level Radiation, 1976.
- Centers for Disease Control and Prevention. "Radiation and Your Health: Radiation Safety." 2015. https://www.cdc.gov/nceh/radiation/safety.html
- Memon, Anjuman Gul, et al. "Occupational health related concerns among surgeons." International Journal of Health Sciences, Vol. 10, No. 2, 2016, pp. 279-91.
- Zadeh, H. G., and T. W. Briggs. "Ionising radiation: Are orthopaedic surgeons' offspring at risk?" Annals of the Royal College of Surgeons of England, Vol. 79, No. 3, 1997, pp. 214-20.
- Sever, Lowell E., et al. "A case-control study of congenital malformations and occupational exposure to low-level ionizing radiation." American Journal of Epidemiology, Vol. 127, No. 2, 1988, pp. 226-42.
- Gardner, Martin J., et al. "Results of case-control study of leukaemia and lymphoma among young people near Sellafield nuclear plant in West Cumbria." British Medical Journal, Vol. 300, No. 6722, 1990, pp. 423-29.
- Abdellah, Rasha F., et al. "Assessment of physicians’ knowledge, attitude and practices of radiation safety at Suez Canal University Hospital, Egypt." Open Journal of Radiology, Vol. 5, No. 04, 2015, pp. 250-58.
- Madrigano, Renata Rodrigues, et al. "Assessment of non-radiologist physicians' knowledge about aspects related to ionizing radiation in imaging exams." Brazilian Radiology, Vol. 47, 2014, pp. 210-16.
- Sin, Ho‐kwan, et al. "Assessing local patients' knowledge and awareness of radiation dose and risks associated with medical imaging: A questionnaire study." Journal of Medical Imaging and Radiation Oncology, Vol. 57, No. 1, 2013, pp. 38-44.
- Kada, Sundaran. "Awareness and knowledge of radiation dose and associated risks among final year medical students in Norway." Insights into Imaging, Vol. 8, No. 6, 2017, pp. 599-605.
- Zewdneh, Daniel, Seife Teferi Dellie, and Tewodros Ayele. "A study of knowledge & awareness of medical doctors towards radiation exposure risk at Tikur Anbessa specialized referral and teaching hospital, Addis Ababa, Ethiopia." Journal of Pharmacy and Biological Sciences, Vol. 2, No. 4, 2012, pp. 1-5.
- Kamoun, H., et al. "Staff knowledge in radiation protection-multicentric study in orthopedic surgery in greater Tunis." Archives of Occupational Diseases and the Environment, Vol. 76, No. 3, 2015, pp. 269-78.
- Famurewa, O. C., et al. "Radiation dose and radiation protection principle awareness: A survey among Nigerian paediatricians." The Nigerian Postgraduate Medical Journal, Vol. 21, No. 1, 2014, pp. 28-33.
- Ongolo-Zogo, P., et al. "Knowledge of radiation protection: Survey of the personnel of the diagnostic, radiotherapy and nuclear medicine hospital services in Yaoundé Cameroon." Radiation Protection, Vol. 48, No. 1, 2013, pp. 39-49.
- Marzouk Moussa, I., and H. Kamoun. "Staff knowledge of radiation protection-A Survey in the University Hospital of Mongi Slim La Marsa (Tunisia)." Radioprotection, Vol. 51, No. 2, 2016, pp. 123-28.
- Al-Rammah, Tamader Y. "CT radiation dose awareness among paediatricians." Italian Journal of Pediatrics, Vol. 42, No. 1, 2016, pp. 1-6.
- Saeed, Mohammed K., et al. "Radiation awareness among physicians about the hazards of radiological examinations on the health of workers and their patients in Saudi Arabia." Journal of Radiation Research and Applied Sciences, Vol. 11, No. 4, 2018, pp. 299-304.
- Hamarsheh, A., and M. Ahmead. "Assessment of physicians' knowledge and awareness about the hazards of radiological examinations on the health of their patients." EMHJ-Eastern Mediterranean Health Journal, Vol. 18, No. 8, 2012, pp. 875-81.
- Partap, Amanda, et al. "Knowledge and practice of radiation safety among health professionals in Trinidad." SAGE Open Medicine, Vol. 7, 2019.
- Brun, Amandine, et al. "Radiation protection for surgeons and anesthetists: Practices and knowledge before and after training." Journal of Radiological Protection, Vol. 38, No. 1, 2018, p. 175.
- Erkan, I., et al. "The investigation of radiation safety awareness among healthcare workers in an education and research hospital." International Journal of Radiation Research, Vol. 17, No. 3, 2019, pp. 447-53.
- Fidan, Firat, et al. "Behaviour and knowledge skill levels of orthopedic surgeons about radiation safety and fluoroscopy use: A survey analysis." Acta orthopaedica et traumatologica turcica, Vol. 53, No. 4, 2019, pp. 301-05.
- Campanella, Francesca, et al. "Are physicians aware enough of patient radiation protection? Results from a survey among physicians of Pavia District-Italy." BMC Health Services Research, Vol. 17, No. 1, 2017, pp. 1-6.
- Sadigh, Gelareh, et al. "Radiation safety knowledge and perceptions among residents: A potential improvement opportunity for graduate medical education in the United States." Academic Radiology, Vol. 21, No. 7, 2014, pp. 869-78.
- Friedman, Ariella A., et al. "Radiation safety knowledge and practices among urology residents and fellows: Results of a nationwide survey." Journal of Surgical Education, Vol. 70, No. 2, 2013, pp. 224-31.
- Harris, Andrew M., et al. "Assessment of radiation safety knowledge among urology residents in the United States." Journal of Endourology, Vol. 33, No. 6, 2019, pp. 492-97.
- Walsh, Devin F., et al. "Radiation safety education as a component of orthopedic training." Orthopedic Reviews, Vol. 11, No. 1, 2019.
- Krille, Lucian, et al. "Systematic review on physician's knowledge about radiation doses and radiation risks of computed tomography." European Journal of Radiology, Vol. 76, No. 1, 2010, pp. 36-41.
- Faggioni, Lorenzo, et al. "Awareness of radiation protection and dose levels of imaging procedures among medical students, radiography students, and radiology residents at an academic hospital: Results of a comprehensive survey." European Journal of Radiology, Vol. 86, 2017, pp. 135-42.
- Moifo, Boniface, et al. "Knowledge on irradiation, medical imaging prescriptions, and clinical imaging referral guidelines among physicians in a sub-Saharan African country (Cameroon)." Radiology Research and Practice, Vol. 2017, 2017.
- Khamtuikrua, Chaowanan, and Sirilak Suksompong. "Awareness about radiation hazards and knowledge about radiation protection among healthcare personnel: A quaternary care academic center-based study." SAGE Open Medicine, Vol. 8, 2020.
- Abuzaid, M. M., W. Elshami, and H. Hasan. "Knowledge and adherence to radiation protection among healthcare workers at operation theater." Asian Journal of Scientific Research, Vol. 12, No. 1, 2019, pp. 54-59.
- Barnawi, Rashid A., et al. "Doctors’ knowledge of the doses and risks of radiological investigations performed in the emergency department." Saudi Medical Journal, Vol. 39, No. 11, 2018, pp. 1130-38.
- Radiation Safety In Dental Practice A study guide and excerpts from The California Radiation Control Regulations pertaining to dental practice Radiation Safety Protection Program template. 2014. https://www.cda.org/Portals/0/pdfs/practice_support/radiation_safety_in_dental_practice.pdf
- Almohaimede, Amal A., et al. "Knowledge, Attitude, and Practice (KAP) of radiographic protection by dental undergraduate and endodontic postgraduate students, general practitioners, and endodontists." International Journal of Dentistry, Vol. 2020, 2020.
- Söylemez, Haluk, et al. "Radiation exposure-do urologists take it seriously in Turkey?" The Journal of Urology, Vol. 187, No. 4, 2012, pp. 1301-05.
- Tabish, S A, SK, Amir. "Knowledge, attitude and practice of radiation safety among radiologists, technologists and X-ray technicians in hospitals of Kashmir." International Journal of Scientific Research, Vol. 7 No. 5, 2018, pp. 989-93.