Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 8
It's an Emergency and Serious, Celiac Crisis, Case Reports and Review
Abdullah Mohammed Albishi1*, Ali Saleh Alshamrani2, Khalid Mousa Asiri2, Bader IbraheemAsiri2, Afnan Ali Abonukhaa2 and Halimah Hussain A Alshehri22Internal Medicine Department, Armed Forces Hospital Southern Region, Khamis Mushayt, Saudi Arabia
Abdullah Mohammed Albishi, Gastroenterology and Endoscopy Department, Prince Sultan Military Medical City, Riyadh, Saudi Arabia, Email: dr.abdullah6975@gmail.com
Received: 23-Jul-2021 Accepted Date: Aug 24, 2021 ; Published: 31-Aug-2021
Abstract
Celiac disease, also known as gluten-sensitive enteropathy, is a chronic systemic autoimmune genetically predisposing disease with a wide diverse range of intestinal and extra-intestinal manifestations triggered by dietary gluten ingestion. Celiac crisis is a rare manifestation of celiac disease but is considered a life-threatening condition and medical emergency in which patients with celiac disease have profuse diarrhea and severe metabolic disturbances. In this article, we are reporting two patients presented with diarrhea, electrolyte disturbance, and a picture of dehydration. They were diagnosed with a celiac crisis. Our aim from this article is to improve the awareness of physicians about the celiac crisis and facilitate its diagnosis and management. A high index of suspicion is needed among clinicians regarding these atypical and very rare presentations.
Keywords
Celiac crisis, Celiac disease, Electrolyte disturbance, Dehydration, Case report
Introduction
Celiac disease, also known as gluten-sensitive enteropathy, is a chronic systemic autoimmune genetically predisposing disease with a wide diverse range of intestinal and extra-intestinal manifestations triggered by dietary gluten ingestion. Celiac disease affects 1% of the general population, but up to 60% of celiac disease diagnosis in adults is due to the atypical manifestations of the disease [1].
Celiac crisis is a rare manifestation of celiac disease but is considered a life-threatening condition and medical emergency in which patients with celiac disease have profuse diarrhea and severe metabolic disturbances. The celiac crisis was reported among the pediatric age group, but rare and not well documented among adults [2].
Case Report
1st Case report
A 61-year-old male, known case of diabetes mellitus type II, hypertension, celiac disease, and hypothyroidism presented to our Emergency Room (ER) complaining of chronic diarrhoea for a long time, but become severe in the last one week which was watery, yellowish, >6-7 bowel motion per day and no history of fever or PR bleeding. It was associated with vague abdominal pain, anorexia as well as recurrent vomiting with an altered level of consciousness for the same duration. He also gave a history of generalized fatigability with significant weight loss of more than 15 kg in the last 6 months. No history of new drugs or antibiotics used no history of contact or traveling recently. No history of similar attacks before or significant family history.
He was diagnosed nine months back as a celiac disease based on histopathology and positive serology as part of his investigations regarding iron deficiency anemia and chronic diarrhea, but he was not compliant with the gluten-free diet.
On Examination
At ER: he was a confused, pale, dehydrated, and ill-appearing patient. No lymphadenopathy.
Vital signs were BP 59/39 mmHg, HR=149 beat/min irregular-irregular, O2 saturation: 81% ambient air, and temperature=36.4°C.
The chest and cardiovascular system were normal.
The abdomen was soft, lax, non-tender, and had no palpable organomegaly. Lower limbs: pitting edema up to mild of thighs.
The central nervous system was grossly intact without signs of meningitis.
Investigations are shown in Table 1.
| CBC | |
| WBC | 10.5 |
| Hb | 8.3 |
| MCV | 84.2 |
| MCH | 26.7 |
| PLT | 657 |
| INR | 239 |
| LFTs | |
| Albumin | 12 |
| ALT | 35 |
| AST | 57.3 |
| Total bilirubin | 13.9 |
| Total protein | 45 |
| Renal profile | |
| Urea | 45.6 |
| Creatnine | 316.3 |
| Na | 123 |
| K | 3.2 |
| Chemistry | |
| TSH | 15 |
| Vit D | 41.3 |
| CRP | 5.6 |
| Ca2+ | 2.17 |
| Mg | 0.49 |
| Blood sugar | 11 mmol |
| Lactic acid | 3.9 |
| Others | |
| Cortisol level | 522 |
| Tissue transglutaminase IgA | 1200 |
ECG was a new Atrial Fibrillation (AF) with a rapid ventricular response. Chest x-ray was unremarkable and cardiac enzymes were normal. Venous blood gases showed pH: 7.29, PCO2: 2.9, HCO3: 13.2.
Stool analysis, parasite, ova, and C. difficile were all negative. Blood, urine, and stool cultures were unremarkable.
CT abdomen was done and showed dilated small bowel up to its end, no sizable mass or lymphadenopathy, patent intra-abdominal vasculatures with normal intra-abdominal organs.
Echocardiography showed EF 50% with mitral regurgitation with a rim of pericardial effusion.
At ER, a fluid challenge with normal saline 1.5 liters as a bolus was initiated, and also the patient was covered with antibiotics and started on a strict gluten-free diet. Over the next few hours, blood pressure was maintained at 85/60 mmHg but his level of consciousness deteriorated more. So, the patient was intubated and shifted to the Intensive Care Unit (ICU). During ICU admission, the patient had persistent hypotension despite fluid replacement, maximum inotropic support, hydrocortisone, board spectrum antibiotics, and ICU supportive care. The patient, unfortunately, died after three days.
2nd Case
A 50-year-old female not know to have any chronic disease before, presented to our ER with a history of intermittent diarrhoea since 3 years become more severe in the last 2 weeks which was watery, yellowish, 5 to 6 times per day, and no blood or mucus. It is associated with a history of perioral numbness, muscular cramps mainly in her legs, and carpal spasms. She has a history of weight loss of more than 10 kg in the last 6 months. No history of fever, abdominal pain, vomiting, hematemesis, melena, PR bleeding, decreases level of consciousness, convulsions, skin rash, and no joint pain. No history of used medications recently (eg: Antibiotics or laxatives, PPI). No history of surgery or history of similar attacks among her family. She had a history of a similar attack of chronic diarrhea associated with electrolytes disturbance (severe hypokalemia with hypocalcemia) before 2 years. At that time, the patient was admitted to our hospital as generalized body weakness with numbness with chronic intermittent diarrhea for investigation. Unfortunately, she refused to stay more than 2 days in the hospital. So, after hydration and correcting the electrolytes she went home against medical advice.
On Examination
The patient looked ill, conscious, oriented, and dehydrated, but wasn’t pale or jaundiced. Vital signs were BP=89/55, HR=116, O2 saturation=94% room air and afebrile cardiac and chest examinations were unremarkable.
The abdomen was soft, lax, non-tender, not distended, and had no palpable organomegaly.
Neuromuscular examination: Cranial nerves were intact, no limbs weakness, normal tone, and no cerebellar signs.
The patient had a positive Trousseau sign and a Chvostek sign.
Investigations are shown in Table 2.
| CBC | |
| WBC | 10.7 |
| Hb | 9.5 |
| MCV | 57.9 |
| MCH | 15.5 |
| PLT | 579 |
| INR | 1.7 |
| LFTs | |
| Albumin | 28.9 |
| ALT | 17.8 |
| AST | 37.8 |
| Total bilirubin | 8.6 |
| Direct bilirubin | 4.7 |
| Renal profile | |
| Urea | 1.42 |
| Creatnine | 57.4 |
| Na | 136.9 |
| K | 2.12 |
| Chemistry | |
| TSH | 3.21 |
| Vit D | 12 |
| CRP | 5.3 |
| Ca2+ | 2.07 |
| Mg | 0.59 |
| Blood sugar | 5.8 mmol |
| Others | |
| Cortisol level | 240.9 |
| Tissue transglutaminase IgA | High |
Blood gases were pH: 7.52, PCO2: 4.87, HCO3: 29.4.
ECG was flatting and inversion in T wave with Q-T interval prolongation in V3-V6. The chest x-ray was normal. Stool analysis, parasite, ova, and C. difficile all were negative. Blood, urine, and stool cultures were unremarkable.
The patient was admitted to ICU and rehydration with IV fluid with IV electrolyte corrections (Ca, Mg, K) were initiated with a close monitor of vital signs.
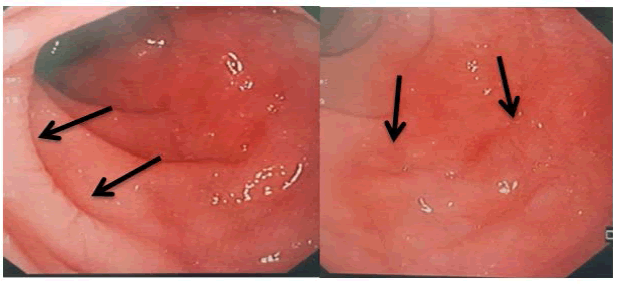
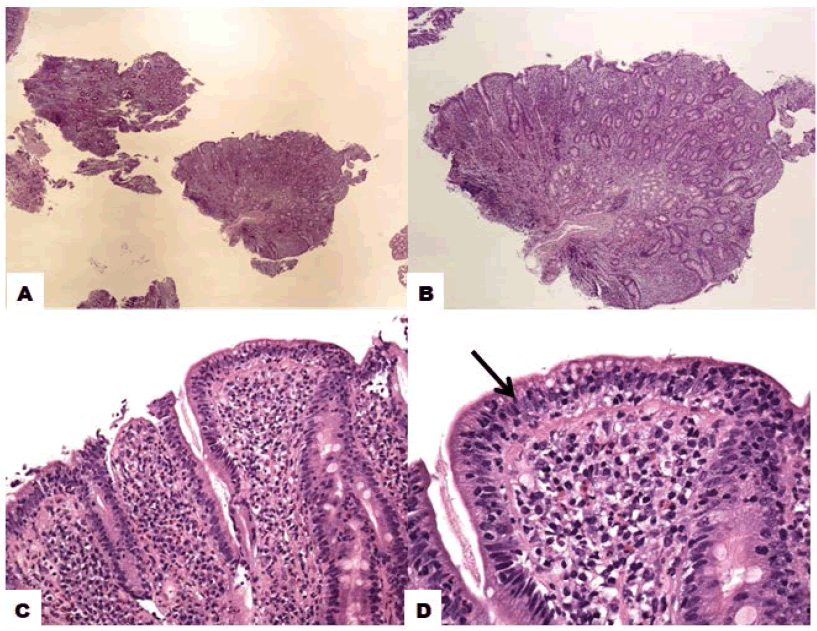
After stabilization, upper endoscopy was done and showed scalloping of duodenal folds and fissuring of mucosa as shown in Figure 1. The biopsy was taken and showed as shown in Figure 2 increase in intra-epithelium lymphocytosis with villous atrophy which going with celiac disease.
Figure 2. Histological features of celiac disease; A-B): Sections show fragments of the duodenal mucosa with total villous change/ atrophy (decrease in villous height, alteration of normal crypt/villous ratio with total disappearance of villi) and increased density of the mixed inflammatory cells in the lamina propria; C): Decreased the height of the enterocyte with flattening of enterocytes, and the presence of some intracytoplasmic vacuolation and reduction of brush border; D): Increased intraepithelial T lymphocytes “intraepithelial lymphocytosis”; Original magnifications. A: 2x, B: 4x, Inset: 10x, C: 20x and D: 40x
CT abdomen was done and showed abundant fluid within the colon, prominent portal vein, an increased number of lymph nodes within the root of the mesentery, no small bowel pathology, and rest of study was normal.
The patient was diagnosed with celiac disease with the crisis. The patient was started on a gluten-free diet; micronutrient deficiencies were corrected along with dietician follow-up for further diet education. The patient was discharged home with follow-up in our clinic after 3 months with labs and celiac serology, but unfortunately patient doesn’t appear again at our hospital.
Discussion
Celiac disease, also known as gluten-sensitive enteropathy, is a chronic systemic autoimmune genetically predisposing disease with a wide diverse range of intestinal and extra-intestinal manifestations triggered by dietary gluten ingestion. Celiac disease affects 1% of the general population, but up to 60% of celiac disease diagnosis in adults is due to the atypical manifestations of the disease [1]. The acute, life-threatening form of celiac disease has been described in the literature as a “celiac crisis” [3].
Celiac crisis is a rare manifestation of celiac disease and is considered a medical emergency in which patients with celiac disease have profuse diarrhea and severe metabolic disturbances. The celiac crisis was reported among the pediatric age group, but rare and not well documented among adults2. Nearly 20 adult celiac crisis patients were reported in the literature. Female patients are predominant than male patients [4].
In 1953, the term “celiac crisis” was first reported in the literature when a case series of 35 cases of children presented with persistent or recurrent diarrhea with a fatality rate of 9% [1].
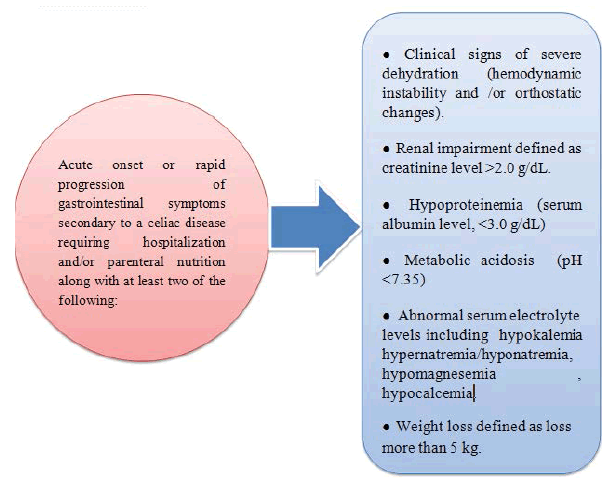
The celiac crisis was defined as rapid progression or acute onset of gastrointestinal symptoms that could be secondary to celiac disease and which required hospitalization and/or parenteral nutrition, with signs or symptoms of malnutrition or dehydration [2].
The celiac crisis should be considered within a context of severe profuse diarrhea, hypoproteinemia, electrolyte, and metabolic disturbances significant enough to require hospitalization [5]. In some cases, the electrolyte imbalances led to cardiologic or neurologic manifestations, which could be the main presenting feature in a patient with a celiac crisis [6].
The mechanism of celiac crisis is unclear, but the combination of immune system hypothesis, an immune stimulus like gluten-included diet, infection, and severe inflammation can start the crisis [4].
Generally, the celiac crisis is not very well documented in the literature and no available guidelines included this aspect in children or adults [6].
Criteria that were used to diagnose a patient with a celiac crisis were seen in Figure 3.
Figure 3. Criteria for the diagnosis of celiac crisis [1]
In our first case report, the patient is already diagnosed with celiac disease, but in the second case report, the patient was not known to have the celiac disease before her presentation which supports that celiac crisis can be the first presentation of celiac disease. A high index of suspicion is needed among clinicians regarding these atypical and very rare presentations of celiac disease.
The main points of celiac crisis management are the initiation of a gluten-free diet, parenteral fluid and electrolyte repletion, and nutritional support. In some cases, corticosteroids may be used [7]. Nutritional support often is required in the short term but most patients will respond to a gluten-free diet [2]. Corticosteroids and appropriate antibiotic coverage should be considered once there is no rapid response to a gluten-free diet [7]. Regarding steroids for celiac crisis treatment, there are different drugs and dosages reported. In the literature, successful results and treatment for the celiac crisis were reported completely [4].
Re-feeding syndrome should be observed clinically and biochemically during the treatment of celiac crisis to prevent and treat this complication once happen [5].
Conclusion
Celiac crisis is a rare, life-threatening condition and medical emergency in which patients with celiac disease have profuse diarrhoea and severe metabolic disturbances. The patient can be treated and managed smoothly if the patient is diagnosed early. A high index of suspicion is needed among clinicians regarding these atypical and very rare presentations of celiac disease. So, the improvement of awareness about this condition is essential for early diagnosis and proper management initiation.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
References
- do Vale, Rômulo Ribeiro, et al. "Celiac Crisis: An unusual presentation of gluten-sensitive enteropathy." Autopsy & Case Reports, Vol. 8, No. 3, 2018.
- Jamma, Shailaja, et al. "Celiac crisis is a rare but serious complication of celiac disease in adults." Clinical Gastroenterology and Hepatology, Vol. 8, No. 7, 2010, pp. 587-90.
- Ferreira, Rogerio, et al. "A celiac crisis in an adult: raising awareness of a life-threatening condition." European Journal of Case Reports in Internal Medicine, Vol. 3, No. 2, 2016.
- Karahan, İrfan, et al. "Celiac crisis: A rare and serious condition resulting in death." Turkiye Klinikleri Journal of Case Reports, Vol. 27, No. 3, 2019, pp. 146-48.
- de-Almeida-Menezes, Marcela, Vírginia Lucia Ribeiro-Cabral, and Sonia S. Lorena. "Celiac crisis in adults: A case report and review of the literature focusing on the prevention of refeeding syndrome." Spanish Journal of Digestive Diseases, Vol. 109, No. 1, 2017, pp. 67-68.
- Balaban, Daniel Vasile, et al. "Celiac crisis, a rare occurrence in adult celiac disease: A systematic review." World Journal of Clinical Cases, Vol. 7, No. 3, 2019, pp. 311-19.
- Jameshorani, Maryam, et al. "Celiac crisis in a young woman: Raising awareness of a life-threatening condition." Middle East Journal of Digestive Diseases, Vol. 11, No. 4, 2019, pp. 230-33.