Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 9
Intra Partum Transperineal Ultrasound to Assess the Progress of Labour and to Predict the Mode of Delivery-A Hospital Based Study
S Senthil Priya1* and R Shankar22Department of Preventive Medicine, VMKVMCH (VMRF-DU), Salem, Tamil Nadu, India
S Senthil Priya, Department of Obstetrics and Gynecology, VMKVMCH (VMRF-DU), Salem, Tamil Nadu, India, Email: senthilpriya200@gmail.com
Received: 18-Aug-2021 Accepted Date: Sep 23, 2021 ; Published: 30-Sep-2021, DOI: O
Abstract
Background: In our country, the rate of emergency cesarean section is increasing year after year by quoting the fetal head station and failure of progress during labor as the major reason for cesarean surgery. The digital vaginal examination is more subjective, the more objective type of assessing the progression of labor by using transperineal ultrasound was recently being used by most of the obstetrician. Aim: To assess the validity of measuring fetal head station, and decent during labor using transperineal ultrasound in assessing the progress of labor. Methodology: A prospective longitudinal study was conducted for one year. A total of 200 study subjects were included as our study subjects with inclusion criteria being singleton with at least 37 weeks of pregnancy and with the longitudinal cephalic type of presentation. Using GE ultrasound machine transperineal ultrasound was performed and the angle of progression was measured by two different obstetricians and the average for two was taken as the final reading. Results: Using the transperineal ultrasound the angle of progression was measured in the first stage of labor for all the antenatal mothers and it was found that the mean angle of progression among the mothers delivered through normal vaginal delivery was 116° and for the cesarean section it was 89° and a statistically significant difference was observed between the two groups. A receiver operator curve was plotted between the angle of progression and normal vaginal delivery and it was shown that antenatal mothers with AOP greater than 99.6° are more prone to deliver by normal vaginal delivery. Conclusion: The angle of progression is the most reproducible ultrasound parameter for the assessment of fetal head descent during labor and it is directly proportional to the probability of vaginal delivery.
Keywords
Transperineal ultrasound, Angle of progression, Vaginal delivery, Caesarean section
Introduction
Digital Vaginal Examination (digital VE) was the only traditional tool available for assessing the progress of labor and it includes cervical dilatation, head station, and its position [1]. This procedure was considered to be highly subjective and was found to be more painful for mothers and has a high risk of developing infection [2,3].
Identifying the antenatal mothers who are at risk of cesarean section is very important to avoid major perinatal complications during the second stage of labor in the form of chorioamnionitis and low umbilical cord pH, and as well as to satisfy the mothers in their experience of childbirth [4]. In our country, the rate of emergency cesarean section is increasing year after year by quoting the fetal head station and failure of progress during labor as the major reason for cesarean surgery [5].
Previously done studies had quoted that digital pelvic examination at the time of labor is not an accurate procedure and it could be misleading in deciding the actual mode of delivery. Misinterpretations in the presence of fetal head molding and caput succedaneum are very common [6,7]. So an ideal assessment tool for assessing the fetal head station and the parturient ability in effective pushing would help us to assess the timing and likelihood of successful pushing. Few of the recently conducted studies had mentioned that the use of intrapartum transperineal ultrasound was found to be a more objective type of imaging technique that was used for monitoring labor with a potency of minimal risk of infection and discomfort to the mothers [8,9]. In this transperineal ultrasound, the two most important parameters that are measured were the angle of progression and the angle of descent. Transperineal ultrasound was in use from 1983 and it was initially used in neonates for examining the anorectal region for diagnosing imperforate anus. It is usually performed with conventional probes, where the probe is directly positioned above the anus, and it captures the images of the anal canal, rectum, puborectalis muscle, vagina, uterus, urethra, and urinary bladder [10].
In TPUS the angle of head progression was first defined by Henrich, et al. as the angle between the infra pubic line of the pelvis, in which a line drawn perpendicular to the longest diameter of the pubis from the lower border and another line drawn perpendicular to the widest diameter of the fetal head and later Barbera described the angle of descent with the degree of midline rotation of the fetal head along with the direction of the fetal head [11,12].
As of today in India, not many studies had been conducted to assess the effectiveness of transperineal ultrasound during labor and so the present study was aimed to assess the validity of measuring fetal head station, and decent during labor using transperineal ultrasound in assessing the progress of labor.
Methodology
A prospective longitudinal study was conducted for a period of one year from Jan 2020 to Dec 2020 in the department of OBG at Vinayaka Missions Kirupananda Variyar Medical College and Hospital, Salem. The study was started after getting clearance from the Institutional ethical committee. A total of 200 study subjects were included in our study. The inclusion criteria for our study were singleton with at least 37 weeks of pregnancy and the presentation of the fetus should be longitudinal cephalic type. Multiple pregnancies, other than the longitudinal cephalic type of presentation, pre-term mothers, antenatal mothers with uterine anomalies, and mothers not willing to participate were excluded from the study. Informed consent was obtained from all the study subjects involved in the study. Patients coming with labor pain, the first and second stages were monitored using both per vaginal examination, and ultrasound was done during the first stage of labor. Ultrasonogram was performed for all subjects using a GE machine. The transducer of the ultrasound was placed between the labia below the symphysis of the pubis in a mid-sagittal position. Sagittal view of the long axis was obtained by just giving a small lateral movement to the transducer, without changing the plane, and a leading portion of the fetal head was detected in the sagittal view and a line was drawn. Calipers were placed between the two ends of the long axis of the symphysis pubis and a second line was drawn from the distal point of the pubic symphysis tangentially to the fetal skull contour. The angle between these two lines was measured to derive the Angle of Progression (AOP). To avoid the subjective variation among the obstetrician, two obstetricians were made to do the measurement and the average between the two readings was taken as the final measurement. All data were entered and analyzed using SPSS version 24. Mean and standard deviation was derived for all parametric variables and the percentage was calculated for frequency variables. Student t-test was used to derive the statistical inference.
Results
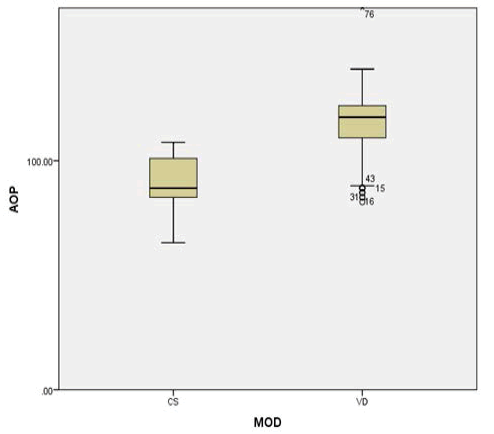
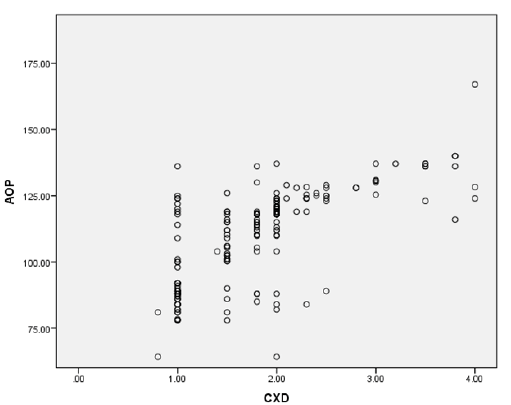
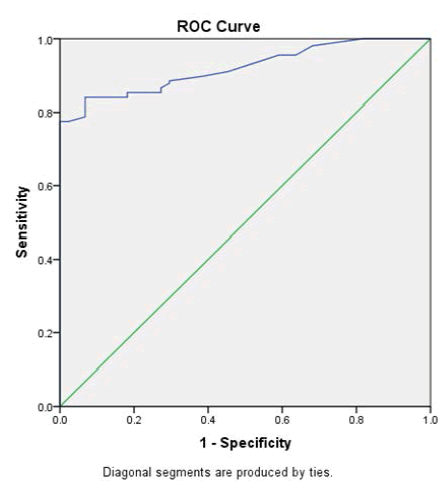
A total of 200 study subjects were included in our study to assess the transperineal ultrasound in the progress of labor. In our study out of 200 antenatal mothers, 156 mothers delivered through normal vaginal delivery and the remaining 44 had undergone cesarean section. We made the comparison of various obstetric variables between the mothers delivered through vaginal delivery and by cesarean section. The mean age of the antenatal mother, gestational age, and maternal weight were almost similar in both groups. Primigravida mothers were more among the mothers delivered by normal vaginal delivery and multigravida mothers were more in cesarean delivery. More than 90% of the mothers had a history of spontaneous conception in both groups. History of medical illness in the form of gestational diabetes, hypertension, hypothyroidism was almost similar in both groups. The mean weight of the newborn and the APGAR score was almost the same among the mothers delivered by normal vaginal delivery as well as mothers delivered by cesarean section (Table 1). Using the transperineal ultrasound the angle of progression was measured in the first stage of labor for all the antenatal mothers and it was found that the mean angle of progression among the mothers delivered through normal vaginal delivery was 116° and for the cesarean section it was 89° and a statistically significant difference was observed between the two groups (p<0.05) (Table 2). A plot diagram also showed that out of 156 normal vaginal delivery mothers only 4 mothers had the angle of progression similar to the mean AOP of mothers delivered by cesarean section (89°) (Figure 1). A scatter plot was made to show the comparison of values between the angle of progression and cervical dilatation and it highlights that cervical dilatation of more than 2 cm was found to have a better correlation with the values of angle of progression compared to the values of <2 cm of cervical dilatation. This proves that the digital vaginal examination would be more sensitive in detecting the progress of labor only when the cervix is well dilated (Figure 2). A receiver operator curve was plotted between the angle of progression and normal vaginal delivery and it was shown that antenatal mothers with AOP greater than 99.6° are more prone to deliver by normal vaginal delivery with the area under the curve of 0.920 and is found to be statistically significant (p<0.0001) and so it can be inferred that the cut-off point for AOP for antenatal mothers who have more chance of normal vaginal delivery is >99.5° (Figure 3 and Table 3).
| Variable | FTND (n=156) | Caesarean (n=44) | p-value |
|---|---|---|---|
| Age | 25.9 ± 3.2 | 25.6 ± 2.9 | 0.819 |
| Gestational age | 38.4 ± 0.4 | 38.6 ± 0.3 | 0.915 |
| Maternal weight | 61.4 ± 7.1 | 60.6 ± 6.8 | 0.764 |
| Primi gravida | 112 (71.7%) | 23 (52.2%) | 0.129 |
| Multi gravida | 44 (28.2%) | 21 (47.7%) | 0.0791 |
| Spontaneous conception | 148 (94.8%) | 40 (90.9%) | 0.684 |
| Induced conception | 8 (5.1%) | 4 (9%) | 0.387 |
| History of medical illness | 31 (19.8%) | 9 (20.4%) | 0.866 |
| New born weight | 2.82 ± 0.6 | 2.79 ± 0.51 | 0.818 |
| APGAR score (1 min/5 min) | 7.8/9.1 | 7.7/9.1 | 0.938 |
| AOP | Vaginal delivery | Caesarean section | p-value (student t-test) |
|---|---|---|---|
| Mean | 116 | 89.5 | <0.0001 |
| SD | 14.2 | 10.2 |
| Area | Std. Errora | Asymptotic Sigb | Asymptotic 95% Confidence Interval | |
|---|---|---|---|---|
| Lower Bound | Upper Bound | |||
| 0.920 | 0.018 | 0.000 | 0.884 | 0.956 |
| Angle of Progression >99.6° -More favourable for normal vaginal delivery | ||||
Discussion
Traditionally ultrasonogram was used in antenatal mothers mainly to assess the growth of the fetus and to rule out congenital anomalies but now as a newer concept transperineal ultrasound was used to assess the progress of labor and it helps the obstetrician to decide on the mode of delivery. The ultrasonogram helps determine the position of the fetal head and its main advantage over digital vaginal examination is that it helps in diagnosing cases of posterior and transverse presentations and its use is more warranted in cases presenting with caput succedaneum and asynclitism [13,14]. Moreover, the antenatal mothers in labor would feel more comfortable using ultrasonograms rather than digital vaginal examinations. A study done by Souka AP, et al. in 2003 found that assessing the fetal head position using digital vaginal examination differs from person to person, and in her study, the reproducibility was only 61% during the first stage of labor and it was reduced to 30% in the second stage of labor and so they found that the subjective error was more in digital vaginal examination [15].
A study done by Molina, et al. in 2010 had evaluated various ultrasound parameters to assess the process of labor and finally quoted that angle of progression is the most reproducible parameter for assessing the descent of the head of the fetus during labor, and a similar finding was also mentioned in the study done by Tutschek B, et al. and Dietz HP, et al., whereas Duckelmann, et al. had shown that though the angle of progression is a reliable ultrasonogram indicator still it depends on professional experience and there is a possibility of inter-observer variation [16-19].
As mentioned in the previous studies done by Silvia Pina Perez, et al. and Zuniga, et al. we also observed a negative correlation between the angle of progression and the expulsion time which means greater the angle lesser the expulsion time but those studies had been done with the angle being measured during the second stage of labor but in our study, we measured the angle of progression only in the first stage of labor [20,21]. In a study done by Amin et al, it was shown that the “angle of progression” ≥ 120° was correlated with an 85.5% probability of vaginal delivery and similarly, another study done by Malik and Singh estimated an angle of progression ≥ 116° as a predictive angle for vaginal delivery in the late first and second stages and it was almost similar to the mean angle of progression for vaginal delivery in our study [5,9].
In our study, the probability of vaginal delivery is 90% if the angle of progression is >99.6° in the first stage of labor and a similar type of results was also shown in the studies done by Silvia Pina Perez, et al. and Kalache, et al., and this shows a strong relationship between the echographic measurement of the angle of descent and the type of delivery [20,22].
In the present study, the ROC curve for the angle of progression for vaginal delivery showed an Area Under the Curve (AUC) of 0.920 (95% Confidence Interval (CI), 0.88-0.95) for the value of the angle of progression that optimizes the curve at 99.60 and more or less a similar type of findings was shown in the study done by Silvia Pina Perez, et al. [20]. Further in their study, they have also found that there was no difference in the angle of progression between vaginal delivery and forceps assisted delivery, whereas in our study we haven’t used forceps for any of the patients. One of the limitations in the present study was, we had measured the angle of progression only in the first stage of labor and it wasn’t measured during the second stage.
Conclusion
Intrapartum transperineal ultrasound examination is a more useful and reliable tool to assess the progress of labor. The angle of progression is the most reproducible ultrasound parameter for the assessment of fetal head descent during labor and it is directly proportional to the probability of vaginal delivery. From the experience of the present study, we would be able to prove that, there has been no cesarean section with an angle of progression equal or greater than 116° during the first stage of labor and the cut-off limit derived through ROC was 99.6°. Further RCTs need to be conducted in comparing the angle of progression values both in the first and second stages of labor to substantiate the importance of performing transperineal ultrasound for deciding the mode of delivery during labor.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
References
- Buchmann, Eckhart, and Elena Libhaber. "Interobserver agreement in intrapartum estimation of fetal head station." International Journal of Gynecology & Obstetrics, Vol. 101, No. 3, 2008, pp. 285-89.
- Eggebo, T. M. "Ultrasound is the future diagnostic tool in active labor." Ultrasound in Obstetrics & Gynecology, Vol. 41, No. 4, 2013, pp. 361-63.
- Wiafe, Yaw Amo, et al. "The effectiveness of intrapartum ultrasonography in assessing cervical dilatation, head station and position: A systematic review and meta-analysis." Ultrasound, Vol. 24, No. 4, 2016, pp. 222-32.
- Yeo, Lami, and Roberto Romero. "Sonographic evaluation in the second stage of labor to improve the assessment of labor progress and its outcome." Ultrasound in Obstetrics and Gynecology, Vol. 33, No. 3, 2009, pp. 253-58.
- Malik, Renuka, and Swati Singh. "Measurement of Angle of Descent (AOD) by transperineal ultrasound in labour to predict successful vaginal delivery." The Journal of Obstetrics and Gynecology of India, Vol. 70, No. 2, 2020, pp: 126-32.
- Barbera, A. F., et al. "Anatomic relationship between the pubic symphysis and ischial spines and its clinical significance in the assessment of fetal head engagement and station during labor." Ultrasound in Obstetrics and Gynecology, Vol. 33, No. 3, 2009, pp. 320-25.
- Wiafe, Yaw Amo, et al. "Acceptability of intrapartum ultrasound by mothers in an African population." Journal of Ultrasound, Vol. 23, No. 1, 2020, pp. 55-59.
- Kreiser, D., et al. "Determination of fetal occiput position by ultrasound during the second stage of labor." Journal of Maternal-Fetal Medicine, Vol. 10, No. 4, 2001, pp. 283-86.
- Amin, Mohamed A., Mohamed A. Eltomey, and Ayman A. El-Dorf. "Role of transperineal ultrasound measurements in women with prolonged second stage of labor as predictors of the mode of delivery." The Egyptian Journal of Radiology and Nuclear Medicine, Vol. 45, No. 4, 2014, pp. 1295-99.
- Akmal, S., et al. "Comparison of transvaginal digital examination with intrapartum sonography to determine fetal head position before instrumental delivery." Ultrasound in Obstetrics and Gynecology: The Official Journal of the International Society of Ultrasound in Obstetrics and Gynecology, Vol. 21, No. 5, 2003, pp. 437-40.
- Henrich, Wolfgang, et al. "Intrapartum Translabial Ultrasound (ITU): Sonographic landmarks and correlation with successful vacuum extraction." Ultrasound in Obstetrics and Gynecology: The Official Journal of the International Society of Ultrasound in Obstetrics and Gynecology, Vol. 28, No. 6, 2006, pp. 753-60.
- Barbera, A. F., et al. "A new method to assess fetal head descent in labor with transperineal ultrasound." Ultrasound in Obstetrics and Gynecology, Vol. 33, No. 3, 2009, pp. 313-19.
- Sherer, D. M., and O. Abulafia. "Intrapartum assessment of fetal head engagement: Comparison between transvaginal digital and transabdominal ultrasound determinations." Ultrasound in Obstetrics and Gynecology: The Official Journal of the International Society of Ultrasound in Obstetrics and Gynecology, Vol. 21, No. 5, 2003, pp. 430-36.
- Yuce, Tuncay, Erkan Kalafat, and Acar Koc. "Transperineal ultrasonography for labor management: Accuracy and reliability." Acta Obstetricia ET Gynecologica Scandinavica, Vol. 94, No. 7, 2015, pp. 760-65.
- Souka, A. P., et al. "Intrapartum ultrasound for the examination of the fetal head position in normal and obstructed labor." The Journal of Maternal-Fetal & Neonatal Medicine, Vol. 13, No. 1, 2003, pp. 59-63.
- Molina, F. S., et al. "What is the most reliable ultrasound parameter for assessment of fetal head descent?" Ultrasound in Obstetrics and Gynecology, Vol. 36, No. 4, 2010, pp. 493-99.
- Tutschek, Boris, et al. "A study of progress of labour using intrapartum translabial ultrasound, assessing head station, direction, and angle of descent." BJOG: An International Journal of Obstetrics & Gynaecology, Vol. 118, No. 1, 2011, pp. 62-69.
- Dietz, H. P., V. Lanzarone, and J. M. Simpson. "Predicting operative delivery." Ultrasound in Obstetrics and Gynecology: The Official Journal of the International Society of Ultrasound in Obstetrics and Gynecology, Vol. 27, No. 4, 2006, pp. 409-15.
- Dückelmann, A. M., et al. "Measurement of fetal head descent using the ‘angle of progression’on transperineal ultrasound imaging is reliable regardless of fetal head station or ultrasound expertise." Ultrasound in Obstetrics and Gynecology: The Official Journal of the International Society of Ultrasound in Obstetrics and Gynecology, Vol. 35, No. 2, 2010, pp. 216-22.
- Perez, Silvia Pina, et al. "Role of intrapartum transperineal ultrasound: Angle of progression cut-off and correlation with delivery mode." linical Obstetrics, Gynecology and Reproductive Medicine, Vol. 3, No. 4, 2017, pp. 1-4.
- Zúñiga, Renato, et al. "Intrapartum translabial ultrasound in determining the duration of the second stage." Peruvian Journal of Gynecology and Obstetrics, Vol. 59, No. 4, 2013, pp. 255-60.
- Kalache, Karim Djaffar, et al. "Transperineal ultrasound imaging in prolonged second stage of labor with occipitoanterior presenting fetuses: How well does the ‘angle of progression’predict the mode of delivery?" Ultrasound in Obstetrics and Gynecology, Vol. 33, No. 3, 2009, pp. 326-30.