Case Report - International Journal of Medical Research & Health Sciences ( 2020) Volume 9, Issue 12
Intentional Replantation with 23-Minute Extra-Oral Time: A Case Report
Ahmed Nasser1, Yazeed Alturki1*, Mohammed Alkathery1 and Khalid Alzailay22AEGD specialist, Advanced Education in General Dentistry, Ministry of Defense, Riyadh, Saudi Arabia
Yazeed Alturki, BDS, King Abdulaziz Medical City, Ministry of National Guard Health Affairs, Riyadh, Saudi Arabia, Email: yazeedcky@gmail.com
Received: 25-Nov-2020 Accepted Date: Dec 21, 2020 ; Published: 28-Dec-2020
Abstract
Non-surgical retreatment and surgical endodontics are not always applicable. Apicoectomy may be limited by anatomical variations, including buccal bone thickness and proximity to vital structures such as nerves and maxillary sinuses. Intentional replantation is considered as a procedure of last resort when non-surgical, or surgical endodontics is contra-indicated. The treatment described demonstrates intentional replantation to be considered a treatment option to preserve and maintain the tooth.
Keywords
Intentional replantation, Retrograde preparation, Root-end resection
Introduction
Grossman defines intentional replantation as the purposeful extraction of a posterior tooth to perform the extra-oral endodontic treatment and the tooth’s replacement in its socket [1]. Minimizing the extra-oral time to the shortest period possible provides the best long-term prognosis [2]. Atraumatic extraction is a crucial factor for the intentional replantation procedure’s success by minimizing the damage to cementum and periodontal ligaments [3]. Specific indications to perform the intentional replantation procedure include limited access to the posterior mandibular molars with conventional apicoectomy procedures because of the buccal bone thickness, high risk of inferior alveolar nerve injury due to its proximity to the mandibular molars apices, root resorptive defects, which does not respond to conventional treatment, endodontic retreatment procedure is not possible due to iatrogenic canal obstruction (i.e., posts, separated instruments, ledges or perforation), [4].
Case Report
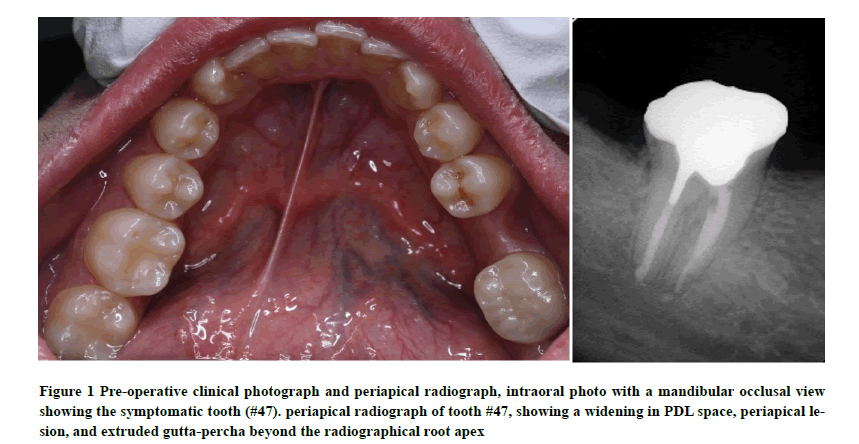
A 29-year-old male patient was referred from the primary care clinic due to persistent dull pain at the mandibular right second molar (#47). His medical history was non-contributory, with no allergies. Dental history showed that tooth #47 received non-surgical root canal retreatment. Clinical examination revealed tenderness to percussion, no mobility with 3 mm pocket depth, and no obliteration of the vestibular depth. The radiographic assessment showed apical radiolucency associated with the tooth (#47), widening periodontal ligament space, and extruded gutta-percha beyond the radiographic root apex (Figure 1). Since he had two root canal retreatments without any observable healing in the periapical tissue, the diagnosis is previously treated with symptomatic apical periodontitis. The available treatment options included tooth extraction and dental implant placement, surgical endodontics, or intentional replantation. The surgical endodontics was contraindicated because of proximity to the inferior alveolar canal. Since the patient preferred to save the tooth, the intentional replantation technique was considered, and the patient accepted this option.
Figure 1. Pre-operative clinical photograph and periapical radiograph, intraoral photo with a mandibular occlusal view showing the symptomatic tooth (#47). periapical radiograph of tooth #47, showing a widening in PDL space, periapical lesion, and extruded gutta-percha beyond the radiographical root apex
Discussion
Intentional replantation is indicated as the last resort when other endodontic treatment options are not feasible. This procedure’s success depends on many factors such as extraction conditions, extra-oral time, handling, periodontal ligament condition, and patient’s general health [5]. During the tooth extraction, the extraction forceps beaks should not go beyond the cementoenamel junction while using elevators are contraindicated to preserve cortical bone integrity [6,7]. The use of periotome implicates a little or no trauma to the root surface and periodontal ligament and decreases the root fracture [8]. Choi et al., reported the use of physics forceps as a reliable extraction instrument [9]. A new technique of using orthodontic extrusion 2 to 3 weeks before the extraction can increase the periodontal ligament volume permitting an extraction with a low risk of tooth fracture [10].
Performing a routine endodontic treatment before the tooth extraction can reduce the extra-oral time; in our case, the extra-oral time was 23-minutes; according to Kratchman, the extra-oral time should not exceed 10 minutes [11]. Cho et al., considered an extra-oral time greater than 15 minutes increases ankylosis occurrence [12]. Pohl et al., reported that if extraoral time is greater than 15 minutes for replanted teeth, root resorption is expected to occur, and the risk of complications is 1.7-fold increased, thus reducing the survival rate of the replanted tooth [13]. During the replantation procedure, the surface root may get damaged, raising the risk of postoperative complications. As reported by Andreasen et al., ankylosis comes about when more than 9 mm2 of the surface root is damaged [14]. When periodontal ligaments’ vitality is preserved by adequately managing the extra-oral time and storage conditions, favorable healing occurs. The periodontal ligament’s complete regeneration along the root surface takes about 7 to 10 days [15].
Commonly used root-end filling materials are Super EBA, GIC, composite, and MTA. MTA’s sealing ability and marginal adaptation have proven superior and not adversely affected by blood contamination. Besides, MTA promotes new cementum deposition and stimulates osteoblastic adherence to the retro-filled surface [16].
A recent evidence-based literature review indicates that splint type and duration were not significant variables with healing outcomes [17]. It should be performed if indicated, such as in teeth with short roots or lack interseptal bone [16,18]. Other studies show that suture splint appears to be more favorable than wire composite splint. Indeed, suture splinting provides physiological loading on the replanted teeth, which might facilitate periodontal healing [19,20]. The success rate ranges from 50% to 95% [21]. The clinical criteria for success include normal function, no mobility, and healthy periodontium. Also, the periapical radiograph should reveal no apical radiolucency or resorption [22].
Conclusion
With careful case selection and suitable training, intentional replantation can have a high success rate and less expensive than other treatment options.
Declerations
Conflict of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Grossman, Louis I. "Intentional replantation of teeth: a clinical evaluation." The Journal of the American Dental Association, Vol. 104, No. 5, 1982, pp. 633-9.
- Shintani, S., et al. "Intentional replantation of an immature permanent lower incisor because of a refractory peri–apical lesion: case report and 5–year follow–up." International Journal of Paediatric Dentistry, Vol. 14, No. 3, 2004, pp. 218-22.
- Messkoub, Mahnaz. "Intentional replantation: a successful alternative for hopeless teeth." Oral Surgery, Oral Medicine, Oral Pathology, Vol. 71, No. 6, 1991, pp. 743-7.
- Asgary, Saeed, Laleh Alim Marvasti, and Alireza Kolahdouzan. "Indications and case series of intentional replantation of teeth." Iranian Endodontic Journal, Vol. 9, No. 1, 2014, pp. 71.
- Deeb, E. "Reimplantation of luxated teeth in humans." Journal of California Dental Association, Vol. 28, 1965, pp. 194-206.
- Forero-López, Jorge, et al. "Surgical management with intentional replantation on a tooth with palato-radicular groove." Restorative Dentistry and Endodontics, Vol. 40, No. 2, 2015, pp. 166-71.
- Lee, Eun-Ung, et al. "Delayed intentional replantation of periodontally hopeless teeth: a retrospective study." Journal of Periodontal and Implant Science, Vol. 44, No. 1, 2014, pp. 13-9.
- Blus, Cornelio, and Serge Szmukler-Moncler. "Atraumatic tooth extraction and immediate implant placement with Piezosurgery: evaluation of 40 sites after at least 1 year of loading." The International Journal of Periodontics and Restorative Dentistry, Vol. 30, No. 4, 2010, pp. 355.
- Choi, Yong-Hoon, Ji-Hyun Bae, and Young-Kyun Kim. "Atraumatic safe extraction for intentional replantation." The Journal of the Korean Dental Association, Vol. 48, No. 7, 2010, pp. 531-7.
- Choi, Y. H., et al. "Clinical outcome of intentional replantation with preoperative orthodontic extrusion: a retrospective study." International Endodontic Journal, Vol. 47, No. 12, 2014, pp. 1168-76.
- Kratchman, Samuel. "Intentional replantation." Dental Clinics of North America, Vol. 41, No. 3, 1997, pp. 603-18.
- Cho, Sin-Yeon, et al. "Retention and healing outcomes after intentional replantation." Journal of Endodontics, Vol. 42, No. 6, 2016, pp. 909-15.
- Pohl, Yango, Andreas Filippi, and Horst Kirschner. "Results after replantation of avulsed permanent teeth. II. Periodontal healing and the role of physiologic storage and antiresorptive–regenerative therapy." Dental Traumatology, Vol. 21, No. 2, 2005, pp. 93-101.
- Andreasen, Jens O., and Lars Kristerson. "The effect of limited drying or removal of the periodontal ligament: periodontal healing after replantation of mature permanent incisors in monkeys." Acta Odontologica Scandinavica, Vol. 39, No. 1, 1981, pp. 1-13.
- Flores, M. T., et al. "Guidelines for the management of traumatic dental injuries. II. Avulsion of permanent teeth." Endodontic Topics, Vol. 14, No. 1, 2006, pp. 110-8.
- Peer, Michael. "Intentional replantation–a ‘last resort’treatment or a conventional treatment procedure? Nine case reports." Dental Traumatology, Vol. 20, No. 1, 2004, pp. 48-55.
- Hinckfuss, Susan Elisabeth, and Louise Brearley Messer. "Splinting duration and periodontal outcomes for replanted avulsed teeth: a systematic review." Dental Traumatology, Vol. 25, No. 2, 2009, pp. 150-7.
- Rouhani, Armita, et al. "Intentional replantation: a procedure as a last resort." Journal of Contemporary Dental Practice, Vol. 12, No. 6, 2011, pp. 486-92.
- Almpani, Konstantinia, Spyridon N. Papageorgiou, and Moschos A. Papadopoulos. "Autotransplantation of teeth in humans: a systematic review and meta-analysis." Clinical Oral Investigations, Vol. 19, No. 6, 2015, pp. 1157-79.
- Chung, Wen–Chen, et al. "Outcomes of autotransplanted teeth with complete root formation: a systematic review and meta–analysis." Journal of Clinical Periodontology, Vol. 41, No. 4, 2014, pp. 412-23.
- Grossman, Louis I., and Irwin I. Ship. "Survival rate of replanted teeth." Oral Surgery, Oral Medicine, Oral Pathology, Vol. 29, No. 6, 1970, pp. 899-906.
- Emmertsen, E. "Replantation of extracted molars: preliminary report." Oral Surgery, Oral Medicine, Oral Pathology, Vol. 9, No. 1, 1956, pp. 115-22.