Research - International Journal of Medical Research & Health Sciences ( 2023) Volume 12, Issue 2
Identification of Microorganisms Causing Neonatal Sepsis and their Antibiotic Susceptibility
Hind A. Alzahrani2*, Khadfga Ahmed Ismail1, Manhal Shbat3, Maaid AlGhathami3, Taisir Saber1, Osama Mahmoud Khalifa4, Amani Al-Malik1, Rawan Alqarni1, Ghala Alsufyani1, Fida Johari1, Maha M. Bakhuraysah1, Amani A. Alrehaili1 and Hayaa M. Alhuthali1*2Basic Sciences, Applied Medical Sciences, Albaha University, Albaha 4781, Saudi Arabia
3Department of Laboratory, King Faisal Medical Complex, Taif, Saudi Arabia
4Ain Shams Faculty of Medicine, Cairo, Egypt
Hind A. Alzahrani, Basic Sciences, Applied Medical Sciences, Albaha University, Albaha 4781, Saudi Arabia, Email: hindalzahrani@bu.edu.sa Hayaa M. Alhuthali, Department of Clinical Laboratory Sciences, College of Applied Medical Sciences, Taif University, Taif, Saudi Arabia, Email: hmhuthali@tu.edu.sa
Received: 20-Jan-2023, Manuscript No. ijmrhs-23-87573; Editor assigned: 23-Jan-2023, Pre QC No. ijmrhs-23-87573 (PQ); Reviewed: 03-Feb-2023, QC No. ijmrhs-23-87573 (Q); Revised: 09-Feb-2023, Manuscript No. ijmrhs-23-87573 (R); Published: 28-Feb-2023
Abstract
Background: Neonatal Sepsis (NS) is the existence of microorganisms that cause hemodynamic changes and other clinical effects, as well as severe morbidity and mortality, it is caused by bacteria, viruses, or fungi. Objectives: Identification of microorganisms causing NS and their antibiotic susceptibility in neonates admitted to the neonatal intensive care unit in King Faisal Medical Complex, Taif, Saudi Arabia. Materials and Methods: Prospective crosssectional study was conducted to detect NS during the period from January to August 2021. The blood samples were collected and submitted to different investigations including blood culture, CBC, and determination of inflammatory markers such as CRP. Results: This study included 110 NS cases, EOS observed in 14 (12.7%), and LOS occurred in 96 (87.3%), the male was 62 (56.3%), female 40 (36.3%) and unknown gender 8 (7.2%), the blood culture technique showed that the most commonly detected microorganisms were CoNS 28 (25.5%) E. coli 26 (23.6%) and K. pneumoniae 22 (20.0%), in addition, the antibiotic susceptibility of isolated strains showed that the Trimethoprim-Sulfamethoxazole was found to be the highest sensitive antibiotic by (83.6%), while Ampicillin was the highest resistant antibiotic by (78.1%). Conclusion: NS is a public health problem so, it is recommended that healthcare organizations design a preventive program to prevent NS specially LOS.
Keywords
Neonatal Sepsis (NS), Early NS, Late NS, Bacterial microorganisms
Introduction
Neonatal Sepsis (NS) refers to the presence of microorganisms such as bacteria, viruses, or fungi that cause hemodynamic changes and significant morbidity and mortality. Depending on the age of onset and timing of the sepsis episode, there are two types of NS, one of them is Early-Onset Sepsis (EOS), and the other one is Late-Onset Sepsis (LOS). EOS infections occur before or after childbirth and reflect vertical mother-to-infant transmission LOS infections occur after delivery or between the ages of 3 days and 7 days and are caused by organisms found in the hospital or the environment [1].
In Saudi Arabia, prematurity is the most common cause of NS. Multiparty and Cesarean Section (CS) delivery is the key maternal risk factor for both EOS and LOS. Most commonly that GBS causes EOS among neonates, while Staphylococcus spp. was the most common organism among LOS neonates. When compared to neonates with LOS, high mortality risk was found in neonates with EOS [2].
The innate and acquired immune systems play a part in neonatal immunity. Innate immunity, which is mediated by phagocytes and the complement cascade, is the first line of defense against infection in newborns. It also controls self-tolerance and communicates with T cells and B cells from the acquired immune system to produce memory responses to antigens, the body has previously experienced. Acquired immunity is a slower but more directed immune response triggered by lymphocytes and antibodies passed down from mothers. Neonates have several immune defects in both systems, rendering them more vulnerable to infection [3].
NS signs and symptoms ranged from nonspecific or ambiguous symptoms to hemodynamic collapse. Irritability, lethargy, or poor feeding are early signs, besides poor perfusion and shock, respiratory distress, fever, hypothermia, and hypotension. Diagnosis is based only on laboratory results that may reveal hyperglycemia or hypoglycemia, acidosis, or hyperbilirubinemia [4].
Escherichia coli, Coagulase-negative Staphylococci, and Listeria monocytogenes are among the most commonly isolated bacteria in NS. Streptococci, Streptococcus pneumoniae, Streptococcus viridans, Haemophilus influenzae, Staphylococcus aureus, and Klebsiella are more or less common bacteria. Group B Streptococci have been isolated and have now been identified as the etiologic cause of NS. Many epidemiological studies on NS have confirmed the major shift from EOS to LOS, as well as a shift in the way bacterial blood culture isolates, are treated. Globally, every year, more than a million neonates die in their first month of life as a result of sepsis or a severe infection. NS has a wide variety of incidences (from less than 1% to more than 35% of live births), depending on the gestational age and time of onset (EOS<72 hours after birth or LOS>72 hours after birth). Of all age groups, preterm neonates have the highest rates of sepsis and mortality [5].
The present study aims to identify the microorganism that is causing NS in patients admitted to King Faisal Medical Complex, Taif, Saudi Arabia, in addition to the screening of their antibiotic sensitivity and resistance.
Methods
A prospective cross-section study was applied at the NICU of King Faisal Medical Complex (KFMC) in Taif, Saudi Arabia. The study period was from January 2021 to August 2021. All neonates’ cases with neonatal sepsis which was suspected by clinical diagnosis and confirmed by blood culture in the NICU were included in the study. a total of 110 neonates with a culture-confirmed diagnosis of neonatal sepsis were included in this study.
Automated Blood Culture by Using BACTEC FX
Blood culture is used to confirm the diagnosis of neonatal sepsis by isolating the causative agent, a minimum of 0·5 mL-1 mL of blood was withdrawn aseptically, preferably from two different venipunctures from two separate sites. True pathogens are more likely to be present in both culture specimens. In the presence of a central venous catheter, blood cultures ideally would be obtained simultaneously, with one from a peripheral and one from a vascular catheter so that differential time to positivity can be assessed. This facilitates the identification of peripheral bacteremia versus catheter-related bloodstream infections and has implications for clinical management. Automatic systems continuously monitor specimens and alert when positive signaling is detected, facilitating further processing for pathogen subculture on blood, MacConkey, and chocolate agar were identified and confirmed by BD Phoenix's automated identification and susceptibility testing system.
Complete blood counts were performed and C-reactive protein as a marker of inflammation was estimated.
Statistical Methods
Data were analyzed using IBM© SPSS© Statistics version 26 (IBM© Corp., Armonk, NY). Categorical variables are presented as counts and percentages. Ordinal data are compared using linear by-linear association. Continuous numerical data are presented as mean and standard deviation and between-group differences are compared using the independent-samples t-test. p-values <0.05 are considered statistically significant.
Ethical Considerations
Ethical approval for this study was obtained from the College of Applied Medical Sciences at Al-Taif University.
Results
This study included 110 NS cases, EOS was observed in 14 (12.7%), and LOS occurred in 96 (87.3%), males 62 (56.3%), females 40 (36.3%) and unknown gender 8 (7.2%).
Detection of Microorganisms After Blood Culture
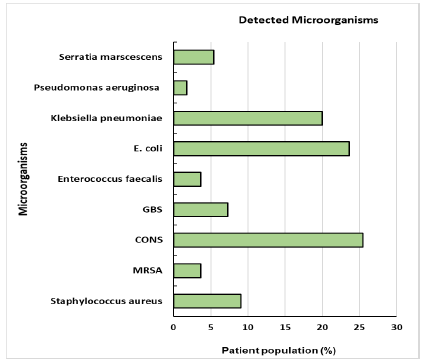
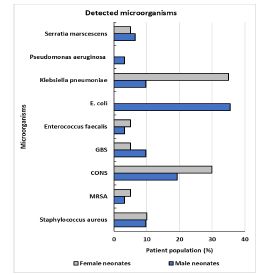
he blood culture technique was used to analyze the microbial species of all NS cases. The following Figure 1 is representing all of the detected microorganisms in all cases, while Figure 2 demonstrated the gender distribution of the detected microorganisms. In overall NS cases, the most commonly detected microorganisms were Coagulasenegative Staphylococci (CoNS) (25.5%), E. coli (23.6%), and K. pneumoniae (20%), while the least detected microorganism was P. aeruginosa (1.8%).
The gender distribution of the detected microorganisms revealed that the most commonly detected microorganisms in male patients were E. coli and then CoNS, whereas in female patients that the most commonly detected microorganisms were K. pneumoniae (Figure 2).
Detection of Antibiotic Susceptibility of Isolated Strains
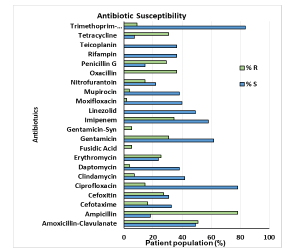
The antibiotic susceptibility of isolated strains from all NS patients was investigated. As shown in Figure 3, Trimethoprim-Sulfamethoxazole was found to be the highest sensitive antibiotic by 83.6%, while Gentamicin-Syn was the lowest sensitivity by 0%. On the other hand, Ampicillin was the highest-resistant antibiotic by 78.1% and linezolid was the lowest resistant by 0%.
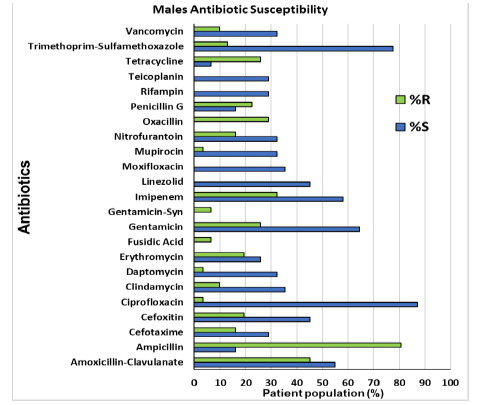
Gender-effect on antibiotic susceptibility is demonstrated in Figure 4 and revealed that ciprofloxacin was the highest sensitive antibiotic in males, while tetracycline is the lowest. Whereas ampicillin was the highest resistant antibiotic in males, mupirocin, daptomycin, and ciprofloxacin were equally the lowest.
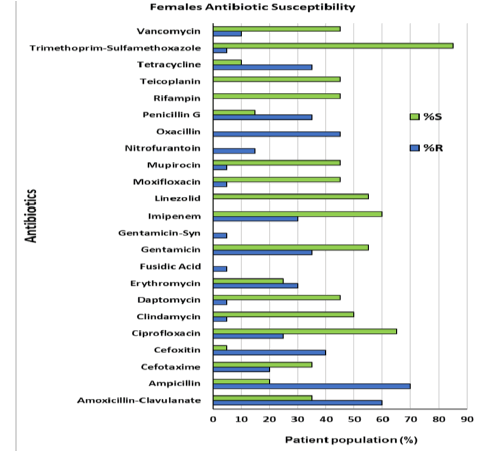
Trimethoprim-sulfamethoxazole is the highest sensitive antibiotic in females while cefoxitin is the lowest. In Figure 5, it is clear that ampicillin was the highest resistant antibiotic in females, while Trimethoprim-Sulfamethoxazole, Moxifloxacin, Gentamicin-Sy, Fusidic acid, Clindamycin, Daptomycin, and Mupirocin were equally the lowest.
Microorganism Susceptibility to Different Antibiotics
Tables 1 and 2 show the antimicrobial resistance pattern of organisms isolated from blood culture. The antibiotics with the highest susceptibility to MRSA are linezolid and moxifloxacin (100%) and Cefoperazone (50%) respectively. Cefotaxime and Ciprofloxacin have the highest CONS susceptibility rates among antibiotics (93%).
| ANTIBIOTICS | Staph aureus (9.09)% | MRSA | CONS | GBS | Enterococcus faecalis |
|---|---|---|---|---|---|
| -3.64% | -25.45% | -7.27% | -3.64% | ||
| Amx | 60 | 0 | 21 | 100 | 100 |
| Amp | 0 |
0 | 21 | 25 | 50 |
| Ctx | 0 | 0 | 93 | 100 | NA |
| Cxt | 0 | NA | NA | NA | 0 |
| Cip | 40 | 0 | 93 | NA | 100 |
| Cp | 60 | 50 | 93 | 100 | NA |
| DAP | 60 | 0 | 93 | NA | NA |
| Ery | 60 | 0 | 14 | 100 | NA |
| Ge | 80 | 0 | 14 | NA | 100 |
| Imp | 40 | 0 | 14 | NA | 100 |
| Lzd | 60 | 100 | 93 | 100 | NA |
| Mxf | 40 | 100 | 93 | 93 | NA |
| Mup | 60 | 0 | 93 | NA | NA |
| Nft | 0 | NA | NA | NA | NA |
| Ox | 0 | 0 | 0 | NA | NA |
| Pg | 60 | 0 | 0 | 100 | NA |
| Rmp | 60 | 100 | 93 | NA | NA |
| Te | 60 | 100 | 93 | NA | NA |
| Te | 60 | NA | 0 | NA | NA |
| Sxt | 80 | 0 | 86 | NA | 100 |
| Vanco | 60 | 0 | 93 | NA | 0 |
| Note: (%=n/total), n=number of sensitive isolates | |||||
| Amp, ampicillin, Amx, amoxicillin, Cip, ciprofloxacin, Cn, gentamicin, Sxt, trimethoprim-sulfamethoxazole, Cxt, cefoxitin, Pg, penicillin, Vanco, vancomycin, CTX, Cefotaxime. CIP, Ciprofloxacin DAP, Daptomycin, ERY, Erythromycin, IMP, Imipenem, LZD, Linezolid, MXF, Moxifloxacin, MUP, Mupirocin, NFT, Nitrofurantoin, OX, Oxacillin, RMP, Rifampin, TE, Teicoplanin. CP, Cefoperazone, NA: not applied | |||||
| Antibiotics | E. coli (23.64)% | Klebsiella pneumoniae (20)% | Pseudomonas aeruginosa (1.82)% | Serratia marscescens (5.45)% |
|---|---|---|---|---|
| Amx | 85 | 18 | 0 | 67 |
| Amp | 8 | 18 | 0 | 33 |
| Ctx | NA | NA | NA | 0 |
| Cxt | 92 | 9 | 0 | 100 |
| Cip | 85 | 82 | 100 | 100 |
| Cp | NA | NA | NA | 0 |
| DAP | NA | NA | NA | 100 |
| Ery | NA | NA | NA | 100 |
| Ge | 85 | 91 | 100 | 100 |
| Imp | 92 | 91 | 100 | NA |
| Lzd | NA | NA | NA | 100 |
| Mxf | NA | NA | NA | 100 |
| Mup | NA | NA | NA | 100 |
| Nft | 92 | NA | 0 | 100 |
| Ox | NA | NA | NA | NA |
| Pg | NA | NA | NA | NA |
| Rmp | NA | NA | NA | NA |
| Te | NA | NA | NA | NA |
| Te | NA | NA | NA | 0 |
| Sxt | 92 | 100 | 100 | 100 |
| Vanco | NA | NA | NA | 100 |
| Note: (%=n/total), n=number of sensitive isolates | ||||
| Amp, ampicillin; Amx, amoxicillin; CIP, ciprofloxacin; Cn, gentamicin; Sxt, trimethoprim-sulfamethoxazole; Cxt, cefoxitin; Pg, penicillin, Vanco, vancomycin, CTX, Cefotaxime. CIP, Ciprofloxacin DAP, Daptomycin, ERY, Erythromycin, IMP, Imipenem, LZD, Linezolid, MXF, Moxifloxacin, MUP, Mupirocin, NFT, Nitrofurantoin, OX, Oxacillin, RMP, Rifampin, TE, Teicoplanin. NA: not applied | ||||
These tests confirmed that CONS were sensitive to vancomycin, linezolid, rifampin, trimethoprim/sulfamethoxazole, mupirocin, and gentamycin.Trimethoprim/sulfamethoxazole and gentamicin were all effective against 80% of isolates. Amoxicillin sensitivity was seen in GBS and Enterococcus fecal. All Gram-negative bacilli isolates were susceptible to gentamicin, amikacin, and colistin whereas 90% were susceptible to cefepime and ciprofloxacin, and 85% to ceftazidime. All the Gram-negative isolates except one Pseudomonal isolate were susceptible to carbapenems (meropenem and imipenem). Data are presented as percentages of antibiotic sensitivity.
Hematological Profile of all Patients
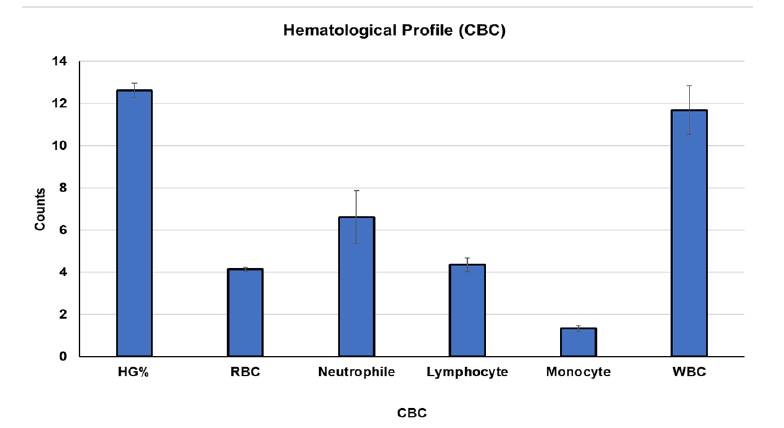
The complete blood count was carried out automatically for the blood specimens of NS patients. The analysis of the hematological profile of all patients in Figure 6 showed the mean ± SE of Hemoglobin concentration was 12.61 ± 2.51, RBC count was 4.13 ± 0.69, Neutrophil was 6.621 ± 3.29, Lymphocyte was 4.35 ± 2.425, monocyte was 1.33 ± 1.027 and WBC was 11.69 ± 8.47.
Figure 6. Evaluation of CBC of blood specimens in all of the NS cases after blood culture (n=110). Data are presented as mean ± standard error. Where the CBC parameters units were; HG%: Hemoglobin percentage; RBC: Red blood cells (M/uL); WBC: White blood cells (K/uL); neutrophils, lymphocytes, and monocytes (K/uL)
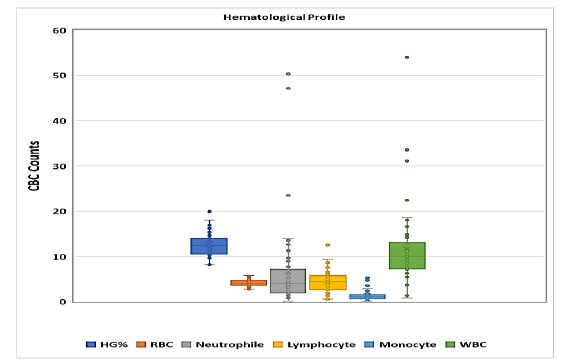
Box-and-Whisker Plot Analysis for Hematological Profile of all Patients
Due to the presence of outliers in the hematological results, the results were submitted to the box-and-whisker plot analysis, lines in the boxes signify the median values; the upper/lower border-lines of the boxes denote the 25th and 75th percentiles, respectively; and the upper/lower bars outside the boxes represent the 90th and 10th percentiles, respectively. Figure 7 indicated that there were a high number of outliers and 75th percentiles cases in neutrophils and WBCs, which may affect their mean values that are presented in Figure 7.
Figure 7. Box-and-whisker plot analysis for Hematological profile of all patients of blood specimens in all of the NS cases after blood culture (n=110). Where the CBC parameters units were HG%: Hemoglobin percentage; RBC: Red blood cells (M/uL); WBC: White blood cells (M/uL); neutrophils, lymphocytes, and monocytes (K/uL)
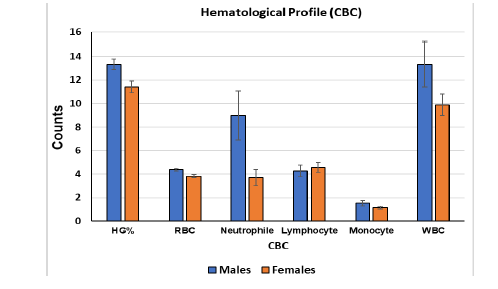
Hematological Profile According to Gender
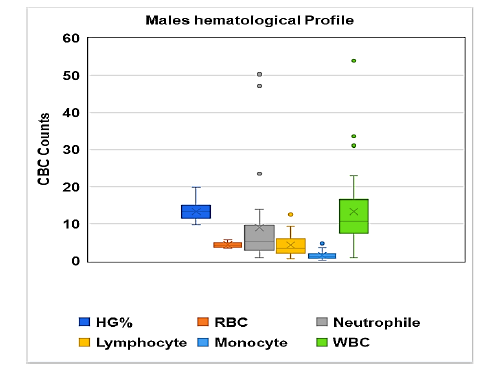
The analysis of the hematological profile in NS patients on a gender basis indicated that the mean ± SE of HG% were (13.32 ± 2.46; 11.42 ± 2.19), RBC count was (4.37 ± 0.67; 3.8 ± 0.60), neutrophils were (8.99 ± 11.64; 3.67 ± 3.07), lymphocyte was (4.26 ± 2.79; 4.57 ± 1.92), monocyte was (1.52 ± 1.27; 1.13 ± 0.49) and WBC was (13.32 ± 5.56; 9.88 ± 4.05) for males and females, respectively. There was a significant increase in WBC and neutrophils in male versus female neonates; p=0.04 and p=0.03, respectively Figure 8.
Figure 8. Evaluation of CBC of blood specimens in all of the NS cases after blood culture (n=110). Data are presented as mean ± standard error. Where the CBC parameters units were; HG%: Hemoglobin percentage; RBC: Red blood cells (M/uL); WBC: White Blood Cells (K/uL); Neutrophils, Lymphocytes, and Monocytes (K/uL)
Box-and-Whisker Plot Analysis for Deference CBC Count Between Males and Females of NS Patients
The analysis indicated that in male patients there were a high number of outliers in neutrophils and WBCs, which may affect their mean values that are presented in Figure 9 and that the female results are more homogenous and the mean values in Figure 10 represent the real findings.
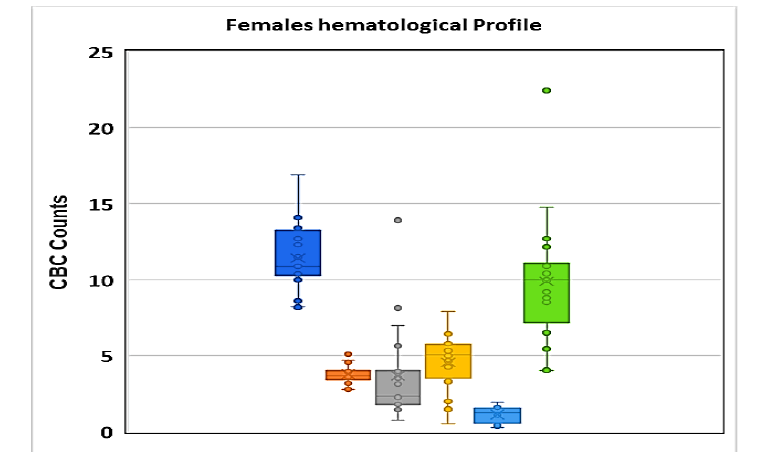
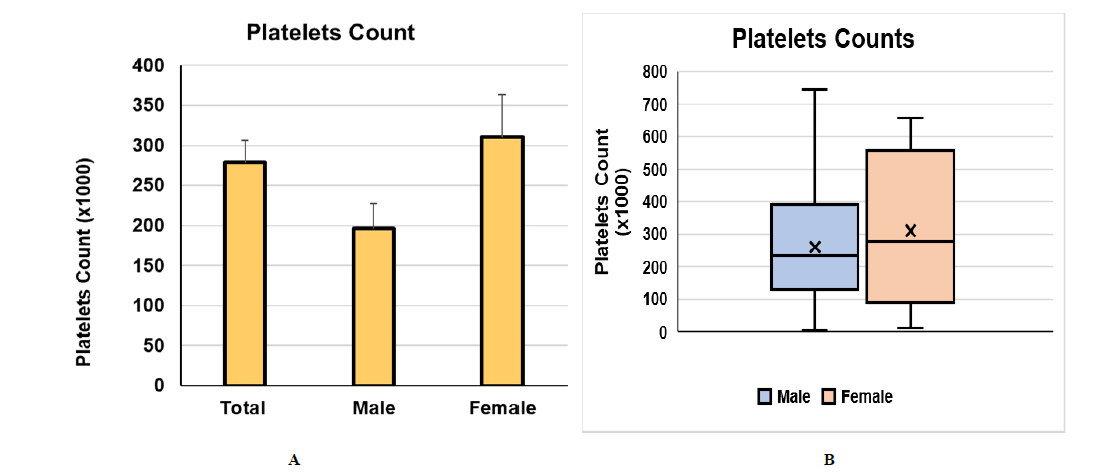
Platelets Count
The complete blood count was carried out automatically in all of the blood specimens of NS patients. Figure 11 showed a non-significant enhancement in platelet count value with a p-value of 0.209. The mean ± SE value in females was 310.3 ± 235.6 and in the male, the mean ± SE was 260.58 ± 196.64. The mean ± SE was 278.81 ± 205.24.
The analysis of platelet counts of all patients indicated that the mean platelet count was lower in males than in females. Box-and-whisker plot analysis revealed the absence of outliers.
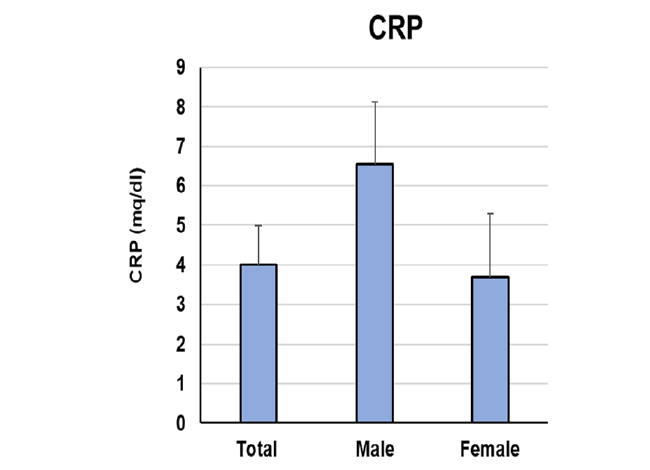
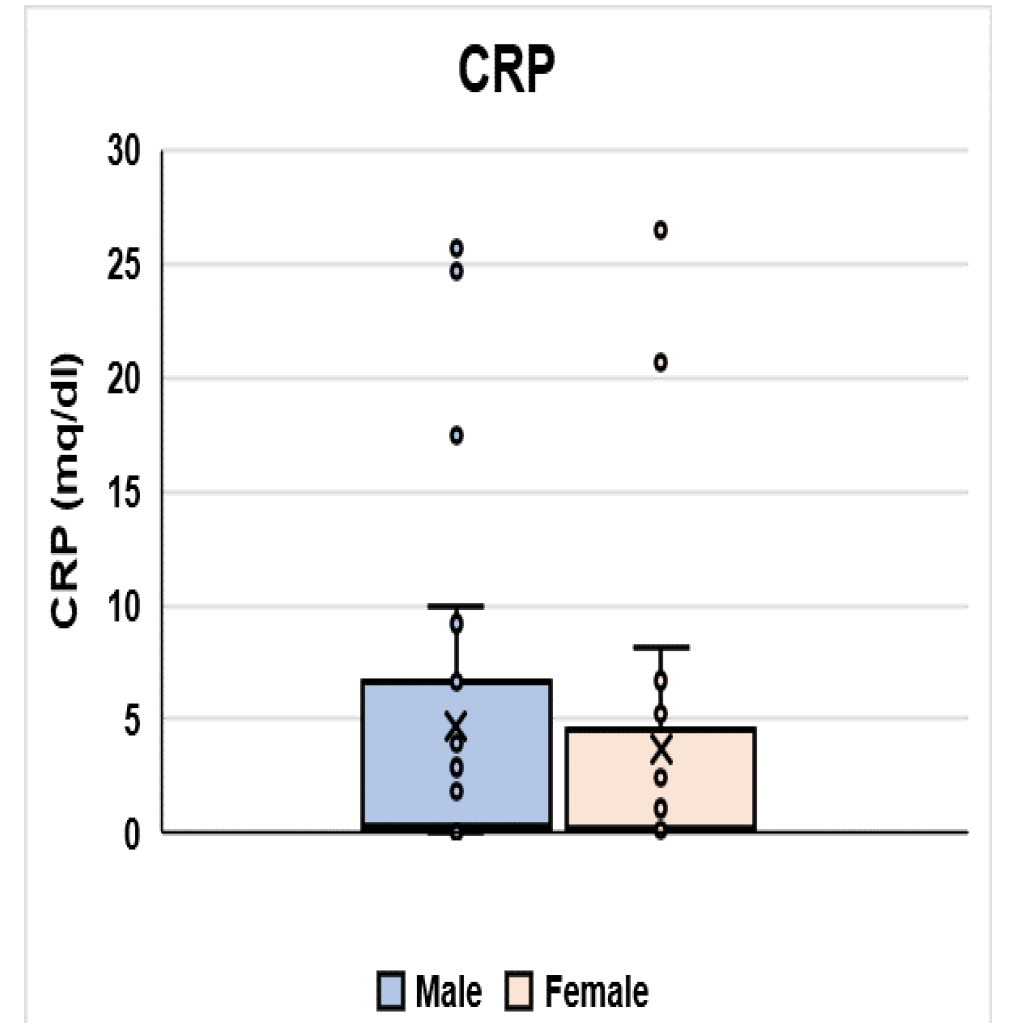
Inflammatory Marker CRP
CRP is an important inflammatory marker was found in all of the NS patients. The results in Figure 11 demonstrated that: the mean value of CRP for the total was 4.00 ± 2.30 (Figure 12).
There was an increased difference in CRP profile, where it showed a higher mean ± SE (6.55 ± 3.7) in males than in females (3.68 ± 1.2) but non-significant (p=0.24).
Box-and-whisker plot analysis revealed the presence of outliers in both males and females groups, a finding that may affect the mean values (Figure 13).
Discussion
Neonatal sepsis is a phrase used to describe the presence of microorganisms that induce significant morbidity and mortality, hemodynamic abnormalities, and other clinical consequences. It can be brought on by bacteria, viruses, or fungi.
n the newborn intensive care unit of the King Faisal Medical Complex in Taif city, this study was done to examine the hematological, chemical, and bacteriological profiles of NS. 110 NS patients were included in this investigation,of whom 14 (12.7%) had EOS and 96 (87.3%) had LOS. Males made up 62 (56.3%), females 40 (36.3%), and 8 (7.2%) were of unspecified gender.
In this study, the blood culture technique was used to analyze the microbial species of all NS cases, which showed in Figure 1, 2 that the most commonly detected microorganisms were CoNS 28 (25.5%), E. coli 26 (23.6%), and k. pneumonia 22 (20.0%), while the least detected microorganism was P. aeruginosa 2 (1.8%).
More or less in agreement with our findings, studies revealed that S. aureus was the most prevalent bacterium associated with NS [6,7]. In contrast to our study, demonstrated that the Streptococcus agalactiae or GBS was the major cause of bacterial infections in the perinatal period, including sepsis which is under study, that showed GBS EOS- infection was the main cause of neonatal sepsis [8,9]. The study of Al-Mazroea, 2017 showed that grampositive bacteria such as CoNS and Staph aureus were the most common culture isolates among sepsis patients, which agrees with our results, gram-negative bacteria were klebsiella Pneumonia, E. coli, and Acinetobacter and Pseudomonas [10].
The keys to effective therapy include immediate supportive care and appropriate antibiotic delivery [11]. According to this study, Gentamicin-Syn had the lowest sensitivity, with Trimethoprim-Sulfamethoxazole having the maximum sensitivity at 83.6%.
In contrast, Ampicillin was the most resistant antibiotic by 78.1%, and linezolid was the least resistant by 0%, as shown in Figures 3-5. Table 2 also revealed that the antibiotics with the highest susceptibility to MRSA are linezolid and moxifloxacin (100%) and Trimethoprim-Sulfamethoxazole (80%) respectively [12]. Cefotaxime and Ciprofloxacin have the highest CONS susceptibility rates among antibiotics (93%). These tests confirmed that CONS were sensitive to vancomycin, linezolid, rifampin, trimethoprim/sulfamethoxazole, clindamycin, and gentamycin. Vancomycin, linezolid, rifampin, and clindamycin were all effective treatments for S. aureus isolates. Trimethoprim/sulfamethoxazole and gentamicin were all effective against 80% of isolates. Penicillin sensitivity was seen in GBS and Enterococcus faecalis.
All Gram-negative bacilli isolates were susceptible to gentamicin, amikacin, and colistin whereas 90% were susceptible to cefepime and ciprofloxacin, and 85% to ceftazidime. All the Gram-negative isolates except one Pseudomonal isolate were susceptible to carbapenems (meropenem and imipenem). The present study showed Streptococci sensitive to Timethoprim-Sulfamethoxazole (Bactrim) [13]. All Gram-negative bacteria were sensitive to Amikacin. P. aeruginosa and Acinetobacter (Gram-negative non-fermenting bacteria,) were sensitive to amikacin and gentamycin. All Gram-positive bacteria were sensitive to gentamycin.
In Neonatology, CBC was the accepted protocol for infants with a suspicion of sepsis. In our investigation, CBC was automatically carried out on individuals with NS. A shift in the HG%, RBCs, Neutrophil, Lymphocyte, Monocyte, WBCs, and platelets was seen in the hematological profile. The mean of WBCs ± SE was 11.69 ± 8.47, Neutrophile was 6.621 ± 3.29, Lymphocyte was 4.35 ± 2.425, and Monocyte was 1.33 ± 1.027, all of which are considerably increased.
The results of platelets showed that females have substantially higher values than males ( p=0.209). The mean ± SE for females was 310.3 ± 235.6 and for males, it was 260.58 ± 196.64. The total mean was 278.81 ± 205.24 as shown in Figures 6-10. Contrasting with the complete blood count results in our study, another study showed a retrospective cross-sectional study (n=67, 623) evaluating the CBC. Although there were lower mean values in some of the components of the CBC, immature neutrophils were higher in neonates with infection, with no difference in platelet counts [14]. Another study showed that males with sepsis have a higher mortality rate, indicating that sexrelated factors can play a role in host susceptibility. Hematological results such as Hb%, WBC, and PLT have been reported, and the latest research found that neonates with anemia, thrombocytopenia, leukopenia, and neutropenia have a higher mortality risk [15]. Late preterm males had a higher risk of composite extreme neonatal morbidity, NICU admission for >3 days, hypothermia, and feeding difficulty as compared to females. Gender variations in late preterm neonatal outcomes may be attributed to unmeasured biologic factors or placental metabolic differences requiring further research [16].
The acute inflammatory protein CRP raises in infected or inflamed areas to 1000 fold [17]. Our results showed in Figure 11 that the total mean value of CRP was 4 mg/dL (The normal value is 0.3 mg/dL to 1.0 mg/dL), and CRP was higher in male than female patients. In male patients, the mean value of CRP is 6.5 mg/dL and this is due to the presence of microorganisms in high percentage in male cases which are E. coli 35.48% and CoNS 19.35%, using the blood culture technique, while in female patients the most common microorganism was K. pneumonia 35% resulting in elevation of the inflammatory marker CRP and the mean value is around 3.85 mg/dL [18-20].
With 168 neonates altogether, only 102 of whom had sepsis in the previous prospective case-control study, the CRP mean in this one was 24.97 mg/dL ± 15.58 mg/dL. (Rashwan et al, 2019). The total CRP was 2.2 mg/dL ± 0.959 mg/ dL in another perspective cross-sectional trial with 75 newborns, although only 9 had sepsis [21].
Conclusion
The most prevalent bacteria in all NS cases were CoNS (predominantly in females), E. coli (only in men), and K. pneumoniae (mainly in females). The most sensitive antibiotic was Trimethoprim-Sulfamethoxazole, while the least sensitive was Gentamicin-Syn. Linezolid had the lowest resistance level while ampicillin had the highest. The most effective antibiotics against CoNS were Cefotaxime and Ciprofloxacin, Trimethoprim-Sulfamethoxazole against K. pneumoniae, and Cefoxitin and Imipenem against E. coli. Males had considerably higher levels of WBCs, neutrophils, and CRP than females, which may be related to the higher prevalence of (E. coli and CoNS) in males.
Declarations
Conflict of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
RECOMMENDATION
A prospective cohort study is recommended to study the risk factors for NS and epidemiological factors, Stewardship Program should be followed.
References
- Al-Matary, Abdulrahman, et al. "Characteristics of neonatal Sepsis at a tertiary care hospital in Saudi Arabia." Journal of infection and public health, Vol. 12, No. 5, 2019, pp. 666-72.
Google Scholar Crossref - Al-Mazroea, Abdulhadi H. "Neonatal sepsis in preterm neonates, Almadina Almunawara, Saudi Arabia, Background, Etiology." Pharmacophore, Vol. 8, No. 1, 2017, pp. 6-10.
Google Scholar - Al-Mouqdad, Mountasser M., et al. "A retrospective cohort study patient chart review of neonatal sepsis investigating responsible microorganisms and their antimicrobial susceptibility." Journal of Clinical Neonatology, Vol. 7, No. 3, 2018, p. 141.
Google Scholar Crossref - Arain, Farzana R., Nisreen A. Al-Bezrah, and Khadijah Y. Al-Aali. "Prevalence of maternal genital tract colonization by group B streptococcus from Western Province, Taif, Saudi Arabia." Journal of Clinical Gynecology and Obstetrics, Vol. 4, No. 3, 2015, pp. 258-64.
Google Scholar Crossref - Battarbee, Ashley N., et al. "538: Gender differences in late preterm neonatal outcomes." American Journal of Obstetrics & Gynecology, Vol. 218, No. 1, 2018, pp. S321-S22.
Google Scholar Crossref - Bhandari, Vineet. "Effective biomarkers for diagnosis of neonatal sepsis." Journal of the Pediatric Infectious Diseases Society, Vol. 3, No. 3, 2014, pp. 234-45.
Google Scholar Crossref - Camacho-Gonzalez, Andres, Paul W. Spearman, and Barbara J. Stoll. "Neonatal infectious diseases: evaluation of neonatal sepsis." Pediatric Clinics, Vol. 60, No. 2, 2013, pp. 367-89.
Google Scholar Crossref - Charles, Marie V.P., et al. "Evaluation of procalcitonin as a diagnostic marker in neonatal sepsis." Indian Journal of Pathology and Microbiology, Vol. 61, No. 1, 2018, pp. 81-84.
Google Scholar Crossref - Ershad, Muhammed, et al. "Neonatal sepsis." Current emergency and hospital medicine reports, Vol. 7, 2019, pp. 83-90.
Google Scholar - Glaser, Margaret A., et al. "Neonatal sepsis: a review of pathophysiology and current management strategies." Advances in neonatal care, Vol. 21, No. 1, 2021, pp. 49-60.
Google Scholar Crossref - Sabeeh Jumah, D., and Kadhum Hassan. "Predictors of mortality outcome in neonatal sepsis." The Medical Journal of Basrah University, Vol. 25, No. 1, 2007, pp. 11-18.
Google Scholar - Mahmoud, Ahmed M., et al. "Effect of COVID-19 Pandemic on Neonatal Sepsis." Clinical labereary, 2022.
Google Scholar Crossref - Nasr, Amre, et al. "Neonatal infections in Saudi Arabia: association with C-reactive protein, CRP-286 (C>T>A) gene polymorphism and IgG antibodies." BMC immunology, Vol. 14, 2013, pp. 1-11.
Google Scholar Crossref - Odabasi, Ilkay O., and Ali Bulbul. "Neonatal sepsis." Sisli Etfal Hastanesi Tip Bulteni, Vol. 54, No. 2, 2020, pp. 142-58.
Google Scholar - Rashwan, Nagwan I., et al. "Validity of biomarkers in screening for neonatal sepsis–a single center–hospital based study." Pediatrics & Neonatology, Vol. 60, No. 2, 2019, pp. 149-55.
Google Scholar Crossref - Shane, Andi L., Pablo J. Sanchez, and Barbara J. Stoll. "Neonatal sepsis." The lancet, Vol. 390, No. 10104, 2017, pp. 1770-80.
Google Scholar Crossref - Singh, Meenakshi, Mahdi Alsaleem, and Cory P. Gray. "Neonatal sepsis." StatPearls Publishing, 2022.
Google Scholar - Sobaih, B. Hasan, and H. Al-Mandeel. "Early and late onset neonatal sepsis in very low birth weight infants in a tertiary center in Saudi Arabia." Journal of Neonatal Biology, Vol. 3, No. 5, 2014, pp. 2-4.
Google Scholar Crossref - Sproston, Nicola R., and Jason J. Ashworth. "Role of C-reactive protein at sites of inflammation and infection." Frontiers in immunology, Vol. 9, 2018, p. 754.
Google Scholar Crossref - Wynn, James L., and Hector R. Wong. "Pathophysiology of neonatal sepsis." Fetal and Neonatal Physiology, 2017, p. 1536.
Google Scholar Crossref - Zamzami, Tarik Y., Anas M. Marzouki, and Hassan A. Nasrat. "Prevalence rate of group B streptococcal colonization among women in labor at King Abdul-Aziz University Hospital." Archives of gynecology and obstetrics, Vol. 284, 2011, pp. 677-79.
Google Scholar Crossref