Research - International Journal of Medical Research & Health Sciences ( 2020) Volume 9, Issue 10
Hospital Readmission after Surgery: Rate and Predisposing Factors (Retrospective Study)
Sultan H Alsaigh1, Khadijah R Airuwaili2*, Lujain I Alsaleh2 and Maram A Alghadoni22Qassim University, College of Medicine, Buraidah, Saudi Arabia
Khadijah R Airuwaili, Qassim University, College of Medicine, Buraidah, Saudi Arabia, Tel: +966 16 380 0050, Email: 351204511@qu.edu.sa
Received: 08-Sep-2020 Accepted Date: Oct 08, 2020 ; Published: 15-Oct-2020
Abstract
Background: Readmission after surgery has become an important topic. Several studies have addressed this issue in different ways. One study assessed the risk factors of readmission 30 days after general surgery and found that many factors can result in readmission and postoperative complications.
Methods: In this retrospective study, we reviewed the medical records of 13,800 patients who underwent surgery between 1/1/2016 and 31/3/2019 at King Fahad Specialist Hospital in Buraidah and documented the operative report, course of admission, and post-discharge records.
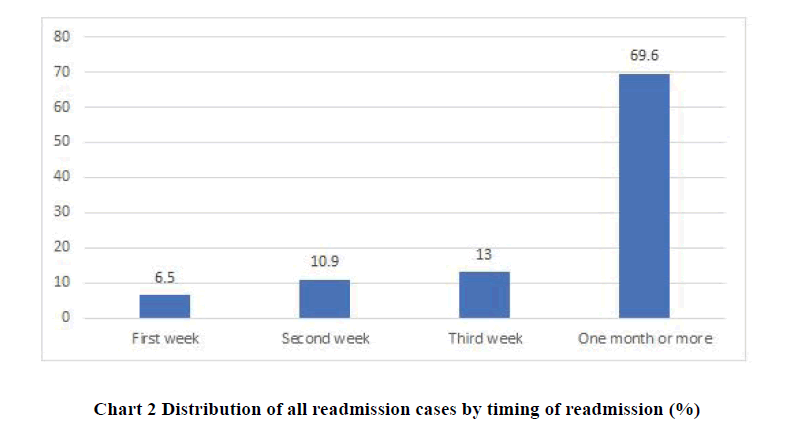
Results: A total of 46 patients were readmitted (readmission rate, 0.33%). The mean age and body mass index did not differ significantly between the planned readmission and unplanned readmission cases (p=0.050). Sex was not associated with readmission type (planned vs. unplanned). The American Society of Anesthesiologists (ASA) grades for readmitted cases were as follows: ASA 1 (37.0%), ASA 2 (47.8%), ASA 3 (10.9%), and ASA 4 (4.3%). The most common cause for readmission was completion of management plan (n=14 30.4%). The majority of patients were readmitted after 1 month (69.6%). Only a few (6.5%) patients were readmitted within the first week.
Conclusion: Readmissions after surgical procedures have multifactorial risk factors; however, postoperative complications appear to be among the most common causes of readmission in surgical patients. Taking appropriate steps to decrease postoperative complications will help minimize postoperative readmissions, and a better understanding of the causes of readmissions after surgery will allow hospitals to develop programs to decrease their rates.
Keywords
General surgery patient, Rate of readmissions, Risk factor of readmission, Predisposing factor
Introduction
Readmission after surgery has become an important issue. Readmission not only affects patients, it cost hospitals considerably; in fact, it costs the United States government more than $17 billion per year. Furthermore, a study measured readmission rates after colorectal surgery and showed that each case costs nearly $9000 [1,2]. Several studies have investigated this issue in different ways. One study assessed the risk factors of readmission 30 days after general surgery and found that many can result in readmission and postoperative complications. Quality of care can be influenced by readmission rate, as another study showed that poor patient care increases early readmission rates [3,4].
Despite the burden of readmission, few studies have examined it in Saudi Arabia, and international studies have not been all-inclusive regarding the underlying causes and factors associated with readmission after surgical hospitalization. The limitations of existing studies include a lack of clinical details that result in the inability to determine a specific valid reason for readmission. Another limitation is the lack of understanding between the complications occurring during the course of admission and causes of readmission (that is, whether the readmission is related to a complication occurring during the course of admission or is a new issue occurring after discharge). Understanding the causes of readmission is essential to identifying risk factors and lowering the readmission rate [5,6].
A study conducted in the United States aiming to understand the reasons for readmission reported that the most common overall reason was Surgical site infection (SSI) (19.5%). In another study, ileus was the most common reason for readmission after bariatric surgery (24.5%) and the second most common reason overall (10.3%). Only 2.3% of patients were readmitted for the same complication that they had experienced during hospitalization. There was no time pattern for readmission, and both early (≤ 7 days post-discharge) or late (>7 days post-discharge) were related to the same most common reasons of SSI, ileus or obstruction, and bleeding [5].
Factors associated with readmission depend on patient condition and surgery type. Different factors are associated with early versus late readmission. Risk factors for readmission after general surgery are multifactorial; nevertheless, postoperative complications seem to drive the readmission of surgical patients. Therefore, applying appropriate measures to minimize postoperative complications will decrease postoperative readmission rates [3,5].
Thomas reported no association between care quality and readmission rates [7]. In addition, a study in the United States reported that surgery type could be related to readmission and that SSI was frequent (19.5%) but varied among surgery types (11.4% for bariatric surgery, 36.4% for lower extremity vascular bypass) [5]. Surgery type is not always the cause, but general anesthesia and insufficient pain management after surgery can affect readmission rates [8].
During hospitalization after surgery, patients may develop undesirable complications leading to a prolonged length of stay, which increases the probability of readmission. The most common complications during the course of hospitalization are SSI, graft failure, myocardial infarction, pneumonia, stroke, and bleeding complications depending on the surgical procedure and method of identifying the complications [9,10].
The American Society of Anesthesiologists (ASA) classification is used in many hospitals to assess patient risk before surgical procedures and help predict postoperative complications. The most frequently reported risk factor associated with an increased risk of 30-day readmissions on multivariate analysis was an ASA score of 4+. Thus, ASA scoring minimizes postoperative complications and readmissions [11].
A study in the United States revealed a significant and independent association between a high ASA class (class 4), cardiac comorbidities, and prior stroke with 30-day unplanned readmissions after anterior cervical discectomy and fusion. The ASA score may be a valuable tool for the preoperative assessment of patients with after anterior cervical discectomy and fusion for the risk of unplanned readmissions [12].
This study aimed to identify the rate and main causes of readmissions after surgery in Qassim and avoid these causes and associated risk factors.
Methodology
This was a retrospective chart review analytic study in which all medical records of patients who underwent surgery between 1/1/2016 and 31/3/2019. During this time, a total of 13,800 surgeries were performed at King Fahad Specialist Hospital, the largest hospital in Buraidah, the capital of the Al-Qassim region in Saudi Arabia, within which almost 600,000 people live. We included all patients who underwent any type of surgery. Patients for whom readmission was planned were excluded. With regard to sample size, we included all patients who met the criteria in the chosen period, which was around 200 patients. For any patient who met the criteria, we reviewed the medical record to review the operative report, course of admission, and post-discharge record.
Data were retrospectively collected from the medical records. We then applied the inclusion and exclusion criteria. We labeled the readmitted patients numerically from 1 to 200 to anonymize their identities. The collected data were entered into an Excel database and then transferred to SPSS version 18 for Windows (IBM, Armonk, NY, USA) for the statistical analysis.
The χ2 test was used to examine categorical variables and the Mann-Whitney U test was used to examine continuous variables. Values of p<0.5 were considered statistically significant. The data were checked for completeness and correctness. Descriptive statistics were used to present the data in tables and charts. Continuous data (age and Body mass index (BMI)) were checked for normality using the Shapiro-Wilk test and Kolmogorov-Smirnov test. These two tests revealed a normal data distribution. The age and BMI of patients for whom readmission was planned versus unplanned were compared using the independent samples t-test. ASA grades were compared between these two groups by one-way analysis of variance. The association between sex and readmission type was observed using the chi-square test.
The analysis was performed in 95% confidence intervals using SPSS version 24.0 (IBM).
Results
A total of 46 of 13,800 patients were readmitted after surgery, a readmission rate of 0.33%. The number of readmissions between 2016 and 2019 by surgery type are presented in (Table 1). The mean age of all readmitted patients was 47.78 ± 17.83 years, while the mean BMI was 28.36 ± 7.65 kg/m2. Neither measure differed significantly between planned and unplanned readmission cases (p>0.050). Among the 46 readmitted patients, 34 (61.8%) were men. Sex was not associated with readmission type (planned vs. unplanned). The ASA grades were as follows: ASA 1 (37.0%), ASA 2 (47.8%), ASA 3 (10.9%), and ASA 4 (4.3%). Most of the planned readmission cases were ASA 2 (65.0%) versus half of the unplanned cases (p=0.198) (Tables 2 and 3).
| Surgical Specialty | Total Cases | Readmission Cases |
|---|---|---|
| GS | 3682 | 26 |
| Maxillofacial | 267 | 2 |
| Dental | 247 | 0 |
| ENT | 57 | 1 |
| Neuro | 18 | 0 |
| Opthal | 824 | 3 |
| Orthopedic | 86 | 2 |
| Oncology | 838 | 2 |
| Plastic | 613 | 2 |
| Thoracic | 120 | 0 |
| Urology | 736 | 7 |
| Vascular | 495 | 1 |
| Total | 13800 | 46 |
| Characteristics | All cases | Planned readmission | Unplanned readmission | p-value | |||
|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | ||
| Age in years | 47.78 | 17.83 | 47.5 | 14.62 | 48 | 20.25 | 0.926 |
| BMI (kg/m2) | 28.36 | 7.65 | 28.85 | 7.86 | 27.98 | 7.61 | 0.708 |
| Characteristics | All cases | Planned readmission | Unplanned readmission | p-value | |||
|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | ||
| Gender | |||||||
| Female | 20 | 43.5% | 9 | 45% | 11 | 42.3% | 0.855 |
| Male | 26 | 56.5% | 11 | 55% | 15 | 57.7% | |
| ASA grade | |||||||
| 1 | 17 | 37% | 4 | 20% | 13 | 50% | 0.198 |
| 2 | 22 | 47.8% | 13 | 65% | 9 | 34.6% | |
| 3 | 5 | 10.9% | 2 | 10% | 3 | 11.5% | |
| 4 | 2 | 4.3% | 1 | 5% | 1 | 3.8% | |
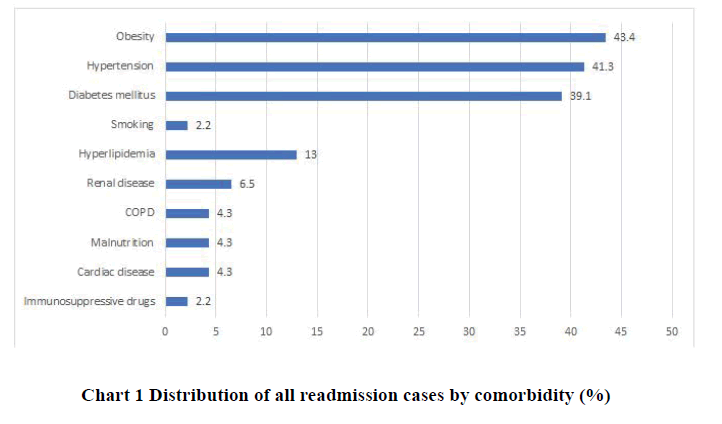
The most common cause of readmission was completion of the management plan (n=14 [30.4%]). All causes of readmission are presented in Table 4. The most frequent type of surgery was Examination under anesthetic (EUA) and fistulotomy (n=7 [15.2%]). All other surgery types are presented in Table 5. The most common comorbidity was obesity (43.4%) (Chart 1).
| Cause | N | % |
|---|---|---|
| Completion of management plan | 14 | 30.4% |
| Completion of thyroidectomy | 3 | 6.5% |
| Redo surgery | 4 | 8.7% |
| Fistula after perianal abscess drainage | 1 | 2.2% |
| Hyperemia after cataract surgery | 1 | 2.2% |
| Hypocalcemia after thyroidectomy | 1 | 2.2% |
| Surgical site infection | 10 | 21.7% |
| Minor amputation | 1 | 2.2% |
| Other causes | 12 | 26.1% |
| Type of Surgery | N | % |
|---|---|---|
| Incision and drainage | 7 | 15.2% |
| PNS excision | 2 | 4.3% |
| DJ stent | 3 | 6.5% |
| Mesh repair | 5 | 6.5% |
| Cataract surgery | 3 | 13% |
| Thyroid surgery | 4 | 8.7% |
| EUA and fistulotomy | 7 | 15.2% |
| Urological stenting | 6 | 13% |
| Post cholecystectomy for stent removal | 3 | 6.5% |
| Minor amputation | 2 | 4.3% |
| Other surgery | 3 | 6.5% |
The majority of the readmitted cases had a clean wound (n=24 [52.2%]). Primary wound closure was performed in 44 (95.7%) cases. A preoperative antibiotic was administered to 32 (69.7%) patients, while a postoperative antibiotic was prescribed in 29 (63.0%) cases. There was only 1 complication (eye pain and decreased vision during hospitalization). One patient received oral antibiotics preoperatively; the rest of the patients received intravenous antibiotics. In contrast, only 6 (13.0%) patients received intravenous antibiotics during the postoperative period. The mean duration of postoperative antibiotics was 6.29 ± 1.68 days (Table 6). The majority of patients (69.6%) were readmitted at more than 1 month after surgery. Only a few (6.5%) patients were readmitted within the first week (Chart 2).
| Course of Hospitalization | N | % |
|---|---|---|
| Type of wound | ||
| Clean | 24 | 52.2% |
| Clean contaminated | 5 | 10.9% |
| Contaminated | 8 | 17.4% |
| Dirty | 9 | 19.6% |
| Type of closure | ||
| Primary | 44 | 95.7% |
| Secondary | 2 | 4.3% |
| Preoperative antibiotic | ||
| Yes | 32 | 69.7% |
| No | 14 | 30.3% |
| Preoperative antibiotic name | ||
| Cefazolin | 28 | 60.9% |
| Other | 4 | 8.7% |
| Postoperative antibiotic | ||
| Yes | 29 | 63% |
| No | 17 | 37% |
| Postoperative antibiotic name | ||
| Cephalosporins | 24 | 52.2% |
| Others | 5 | 10.9% |
Discussion
Hospital readmission has been used as an indicator of care quality. As in several studies of different patient groups and conditions, a decrease in care quality leads to a higher number of readmissions [13,14]. In April 2012, the Centers for Medicare and Medicaid Services presented a new practice to accommodate hospital repayments based on the number of readmissions, with excessive readmissions leading to decreased payments [3]. Furthermore, the Agency for Healthcare Research and Quality initiated a program named Re-Engineered Discharge that targets patient education to aid successful hospital discharge [3]. In agreement with earlier studies, our study found that surgical patients are at a greater risk for readmission than other patients. A study in 2012 that measured the readmission rate observed 11.3% readmission rate among surgical patients at 30 days after surgery [3]. Jencks, et al. also found a 30-day readmission rate of 15.6% among a sample of 11,855,207 media care patients following surgery [15]. As in our study, the readmission rate was around 23% after 30 days of readmission following surgery. With the current increased consideration of hospital readmission, it is necessary to focus on understanding its risk factors and prevention.
Readmissions after surgery are considered multifactorial. Our study results demonstrate that the most common reasons were completion of the management plan (30.4%), postoperative complications (21.7%), and others (26.1%). However, completion of the management plan, such as removal of the foreign body and stinting in our result, is planned and should not be considered a preventable cause. A study in 2015 assessed the contributions of planned readmissions and patient comorbidities to high readmission rates in vascular surgery patients and reported a 24% readmission rate after vascular surgeries since most were planned or scheduled for completion or the removal of a foreign body [16]. Moreover, planned readmissions for completion of a procedure would not be considered a decrease in care quality and hence should not be penalized [16].
On the other hand, unplanned readmission was mostly associated with postoperative complications such as SSI, which showed a high readmission rate in our study. Prior studies demonstrated that postoperative complications are the most notable independent risk factor for surgical readmission [3]. A recent study in the United States investigated the underlying reasons for readmission following surgery and reported the highest rate for postoperative complications, particularly SSI [5].
Various risk factors such as procedure type, hospitalization course, and length of stay are associated with readmission risk. In our analysis, the most frequent procedures performed were EUA and fistulotomy (15.2%), incision and drainage (15.2%), and urological stenting (13%), rates of which cannot be reduced. Likewise, ASA scores also appear to influence the readmission rate among surgical patients [11]. As stated in earlier studies, most readmissions occurred more than 30 days after surgery, and our study acknowledges that. Multiple comorbidities such as obesity, hypertension, and diabetes, as shown in our analysis, also affect a patient’s risk of readmission. Consistent with a previous study, patients with dyspnea, immunosuppression, and poor wound healing were associated with a higher risk of readmission [3]. Another study demonstrated that female sex, AIDS, anemia, chronic kidney disease, collagen vascular disease, diabetes mellitus, hypertension, pulmonary hypertension, congestive heart failure, and atrial fibrillation were independent predictors of 30-day readmission [17].
Conclusion
Readmissions after surgical procedures involve multiple risk factors; however, postoperative complications appear to be among the most common causes of readmission in surgical patients. Taking appropriate steps to decrease postoperative complications may help minimize postoperative readmissions, while increasing our understanding of the causes of readmissions after surgery will allow hospitals to develop programs to decrease readmission rates. Our study demonstrated the readmission rates of postoperative patients and identified the main causes of readmission. Future studies must focus on specifically targeting high-risk patients with multiple medical comorbidities to decrease the 30-day readmission rate because reducing readmissions even by small amounts will have a large impact on hospital budgets and operations.
Limitation
The first limitation of our study is its retrospective nature. Second, the data were collected locally for a single hospital, and the small study size led to deficiencies in statistical power. Future studies with larger sample sizes should be conducted to build and validate predictive models for 30-day readmission risk.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Lucas, Donald J., and Timothy M. Pawlik. "Readmission after surgery." Advances in Surgery, Vol. 48, 2014, pp. 185-99.
- Wick, Elizabeth C., et al. "Readmission rates and cost following colorectal surgery." Diseases of the Colon and Rectum, Vol. 54, No. 12, 2011, pp. 1475-79.
- Kassin, Michael T., et al. "Risk factors for 30-day hospital readmission among general surgery patients." Journal of the American College of Surgeons, Vol. 215, No. 3, 2012, pp. 322-30.
- Ashton, Carol M., et al. "The association between the quality of inpatient care and early readmission: A meta-analysis of the evidence." Medical Care, Vol. 35, No. 10, 1997, pp. 1044-59.
- Merkow, Ryan P., et al. "Underlying reasons associated with hospital readmission following surgery in the United States." JAMA, Vol. 313, No. 5, 2015, pp. 483-95.
- Tayne, Samantha, et al. "Risk factors for 30-day readmissions and modifying postoperative care after gastric bypass surgery." Journal of the American College of Surgeons, Vol. 219, No. 3, 2014, pp. 489-95.
- Thomas, J. William. "Does risk-adjusted readmission rate provide valid information on hospital quality?" Inquiry, Vol. 33, No. 3, 1996, pp. 258-70.
- Salas, B. Jiménez, et al. "Causes of unplanned admission after orthopaedic procedures in ambulatory surgery." Revista Española de Cirugía Ortopédica y Traumatología, Vol. 64, No. 1, 2020, pp. 50-6.
- Tahhan, Georges, et al. "Characterization of planned and unplanned 30-day readmissions following vascular surgical procedures." Vascular and Endovascular Surgery, Vol. 51, No. 1, 2017, pp. 17-22.
- Khan, Nadia A., et al. "Association of postoperative complications with hospital costs and length of stay in a tertiary care center." Journal of General Internal Medicine, Vol. 21, No. 2, 2006, pp. 177-80.
- Park, Jae-Hyun, et al. "The American Society of Anesthesiologists score influences on postoperative complications and total hospital charges after laparoscopic colorectal cancer surgery." Medicine, Vol. 97, No. 18, 2018, p. e0653.
- Phan, Kevin, et al. "Relationship between ASA scores and 30-day readmissions in patients undergoing anterior cervical discectomy and fusion." Spine, Vol. 42, No. 2, 2017, pp. 85-91.
- Rosen, Amy K., et al. "Examining the impact of the AHRQ Patient Safety Indicators (PSIs) on the Veterans Health Administration: The case of readmissions." Medical Care, Vol. 51, No. 1, 2013, pp. 37-44.
- Maeda, Jared Lane K. "Evidence-based heart failure performance measures and clinical outcomes: a systematic review." Journal of Cardiac Failure, Vol. 16, No. 5, 2010, pp. 411-8.
- Jencks, Stephen F., Mark V. Williams, and Eric A. Coleman. "Rehospitalizations among patients in the Medicare fee-for-service program." New England Journal of Medicine, Vol. 360, No. 14, 2009, pp. 1418-28.
- Glebova, Natalia O., et al. "Contributions of planned readmissions and patient comorbidities to high readmission rates in vascular surgery patients." Journal of Vascular Surgery, Vol. 63, No. 3, 2016, pp. 746-55.
- Kim, Luke K., et al. "Thirty‐Day readmission rates, timing, causes, and costs after ST‐Segment-Elevation myocardial infarction in the United States: A national readmission database analysis 2010-2014." Journal of the American Heart Association, Vol. 7, No. 18, 2018, p. e009863.