Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 9
Green Approach Using T. aestivum and P. betel in Treatment of Haloperidol and Phenyl Hydrazine Induced Anemia in Rats
Sonia Johri* and Neha KhanSonia Johri, Department Of Life Sciences, ITM University, Gwalior, India, Email: soniajohari@itmuniversity.ac.in
Received: 18-Aug-2021 Accepted Date: Sep 23, 2021 ; Published: 30-Sep-2021, DOI: O
Abstract
Plants have been a source of vital pharmaceutical drugs for the treatment of many diseases. The present study aims to examine the antioxidant and antianemic potential of T. aestivum and P. betel extract. The FTIR and HPLC were performed for the characterization studies and revealed the presence of catechin (Flavonol) and many other flavonoids. Hematological and ferrokinetic parameters were performed using standard laboratory methods in haloperidol and phenylhydrazine induced anemia in rat model In phenylhydrazine induced anemia, twenty-five female albino rats weighing 110 ± 10 g were divided into five groups of 5 animals each. The liver was excised for determination of Lipid Peroxidation (LPO), reduced glutathione (GSH) levels, Superoxide Dismutase (SOD), Catalase (CAT), Glutathione S-Transferase (GST), Glutathione Reductase (GR) glutathione peroxidase (GPx). Results revealed that TBARS level is significantly increased in the phenyl hydrazine group and decreased in the treatment group. GSH, SOD, CAT, GST, GR and GST level is decreased in toxicant group and significantly increased in the therapy group. Results concluded that combination (TA+PB) therapy showed the best results in comparison to TA and PB therapy individually.
Keywords
Antianemic, Antioxidant, Hematology, Hepatoprotection HPLC, Phenylhydrazine, Piper betel, Triticum aestivum
Introduction
Plants are a rich source of natural antioxidants. The herbal medicines are comparatively safe and environmentally friendly. They play an important role in health care programmed worldwide and there is a recovery of interest in herbal medicines for the treatment of various hepatopathies [1]. Oxidative balance is defined to be a state when the rate of production and removal of free radicals is balanced. Any change in the decrease rate of removal or increase production of free radicals leads to the generation of ROS which finally results in oxidative stress. An antioxidant can scavenge the free radicals due to their redox hydrogen donators and singlet oxygen quencher [2]. Due to the insufficient number of antioxidants, free radicals cannot be neutralized and results in oxidative stress are generated. Oxidative stress leads to several diseases like cardiovascular diseases, cancer, and aging [3]. Many researchers supported the study of the mechanism of hemolytic actions of several agents on RBCs and it has been reported that hemolytic injury is related to oxidative stress. Hemolytic agents have been reported to cause membrane lipid peroxidation and denaturation of cytoskeletal protein [4]. Cellular glutathione and related enzymes such as glutathione peroxidase, glutathione S-transferase and glutathione reductase are among the principal protective mechanisms against endogenous and exogenous toxic substances and free radical-mediated damage in all tissues mainly hepatocytes [5,6].
Wheat (Triticum aestivum), the grass is generally called ‘wheatgrass’ germinated over 6-10 days, belongs to the family Gramineae (Poaceae) [7,8]. Piper betel belongs to the Piperaceae family Piper betel (Paan). Studies have reported the biological benefits of P. betel which include inhibition of platelet aggregation and immune-modulatory properties [9,10]. This is attributed to the high antioxidant activities of this plant [11,12]. Wheatgrass fresh juice is used as a nutritional supplement for decades [13]. The present study aims to examine the antianemic, antioxidant and hepatoprotective activity of T. aestivum and P. betel extract in a rat model with the help of marker enzymes.
Materials and Methods
Fresh Piper betel (paan) leaves were procured from village Sandalpur Antri of Gwalior, M.P. Triticum aestivum was cultivated in ITM University, Gwalior, Turari Campus. The leaves were cut into small pieces and dried in shade at room temperature, followed by grinding into fine powder. Powdered leaves (50 g) were extracted with n-butanol solvent by using the soxhlet apparatus.
Characterization Studies
High-Performance Liquid Chromatography (HPLC): The plant’s extract was exposed to HPLC analysis using HPLC system with C18 column, liquid pump, system controller, UV-Vis detector (Shimadzu, 02059), and the detection at 267 nm with mobile phase methanol. Identification of the peaks was done with respective references [13]. 1 ppm of the sample was dissolved in 10 ml HPLC grade methanol. 1 ml of the sample was injected into the HPLC and a chromatogram was obtained for each sample.
In vivo Studies
Animals: Twenty-five healthy female albino rats of Sprague dawley strain weighing 110 ± 20 g were used for the study. The animals were procured from Defence Research Development Establishment (DRDE), Gwalior, Madhya Pradesh. The rats were housed in polypropylene cages, at (25 ± 3)℃, temperature and 12 hrs light and 12 hrs dark cycles. The animals had free access to a commercial rat pellet diet and water ad libitum. They were housed in the animal facility of ITM University, Gwalior which is registered (Re/S/16/CPCSEA).
Experiment 1
In vivo study in haloperidol-induced iron deficiency anemia: All the animals were divided into five groups of five animals each. Hematological parameters WBC, RBC, HGB, HCT, MCV, MCH, MCHC, and PLT were estimated by using a blood analyzer (Horiba ABX, MICROS 60).
Induction of iron deficiency anemia: Anaemia was induced in rats by inducing Haloperidol (HP) intraperitoneally at 0.2 mg/Kg for 4 consecutive days in Group II, III, IV, V followed by a rest of one day. Treatment with extract sustained in Group from III to V with 20 mg/kg for 21 days [14].
Group I (Normal) maintained a standard iron-rich diet.
Group II (Experimental) received HP 0.2 mg/Kg intraperitoneally once daily for 4 days.
Group III (Treatment I) received HP 0.2 mg/Kg intraperitoneally once daily for 4 days and 20 mg/kg PB extract orally for 21 days.
Group IV (Treatment II) received HP 0.2 mg/Kg intraperitoneally once daily for 4 days and 20 mg/kg TA extract orally for 21 days.
Group V (Treatment III) received PHZ 0.2 mg/Kg intraperitoneally once daily for 4 days and 20 mg/kg PB+TA extract orally for 21 days.
Experiment 2
In vivo study in PHZ induced hemolytic anemia
Induction of hemolytic anemia: Anaemia was induced in rats by inducing Phenyl Hydrazine (PHZ) intraperitoneally at 20 mg/Kg for 6 consecutive days in Group II, III, IV, V followed by a rest of one day [15]. Treatment with extract sustained in Group from III to V with 20 mg/kg for 14 days. Group II was given the rest of 14 days.
All the animals were divided into five groups of five animals each.
Group I (Normal) received normal saline for 6 days.
Group II (Experimental) received PHZ 20 mg/Kg, once daily for 6 days.
Group III (Treatment I) received PHZ 20 mg/Kg, once daily for 6 days, and 20 mg/kg PB extract orally for 14 days.
Group IV (Treatment II) received PHZ 20 mg/Kg, once daily for 6 days and 20 mg/kg TA extract orally for 14 days.
Group V (Treatment III) received PHZ 20 mg/Kg, once daily for 6 days and 20 mg/kg PB+TA extract orally for 14 days.
Phenyl Hydrazine (PHZ) was injected intraperitoneally at 20 mg/Kg for 6 consecutive days in Group II, III, IV, V followed by a rest of one day. Treatment with extract sustained in Group from III to V with 20 mg/kg for 14 days. Experimental Control Group II was given the rest of 14 days.
On the 22nd day, the rats were weighed and anesthetized with diethyl ether and blood was withdrawn from the orbital plexus of the rat eye in heparinized vials. Animals were sacrificed and liver tissues were excised for biochemical parameters. Hematological parameters WBC, RBC, HGB, HCT, MCV, MCH, MCHC, and PLT were estimated by using a blood analyzer (Horiba ABX, MICROS 60).
Tissue Homogenate Preparation
The liver was homogenized with a homogenizer in 1% sucrose solution for reduced glutathione (GSH), 0.15 M KCl for lipid peroxidation, normal saline for Superoxide Dismutase (SOD) and Catalase activity, 1.15% KCl for Glutathione-S-Transferase (GST), Glutathione Reductase (GR) and Glutathione peroxidase activity (GPx).
Tissue Biochemistry
Lipid Peroxidation (LPO): Lipid peroxidation levels were measured by the Thiobarbituric Acid (TBA) reaction using the method of Sharma and Krishnamurthy [16]. 1 ml homogenate in a test tube was incubated at 37℃ for 30 min. 1 ml TCA was added and centrifuged at 2000 rpm for min. To 1 ml supernatant, 1 ml thiobarbituric acid TBA was added and incubated at 100ºC for 10 min cooled, and optical density was measured at 535 nm.
Reduced Glutathione (GSH): To 1 ml of 0.1% homogenate, 1 ml sulphosalysilic acid was added and then centrifuged at 5500 rpm for 10 min. 4.5 ml tris buffer was added in supernatant followed by adding 0.5 ml DTNB. Optical density was recorded at 412 nm [17].
Superoxide Dismutase (SOD): The activity of Superoxide Dismutase (SOD) was estimated by following the procedure of Marklund and Marklund [18]. A 3 ml aliquot of assay mixture composed of 50 mM Tris-HCl buffer, 1 mM diethylene triamine penta-acetic acid, 45 ml of 10 mM pyrogallol in 10 mM HCl, and 10 ml of tissue supernatant. The SOD activity was expressed in units per mg protein of tissues [18].
Catalase: 20 μl tissue homogenate was taken and mixed with 1 ml potassium phosphate buffer (50 mM) followed by adding 1 ml H2O2. Optical density was measured for 3 min at 240 nm [19].
Glutathione-S-Transferase (GST): GST enzyme activity was measured by reaction mixture containing a cocktail of 0.05 ml homogenate, 0.5 ml phosphate buffer, 0.05 ml CDNB and 0.85 ml distilled water. It was incubated for 10 min at room temperature followed by the addition of 25 μl GSH in each tube. Absorbance was measured for 5 min at 340 nm [20].
Glutathione Reductase (GR): To 0.1 ml homogenate 0.7 ml phosphate buffer (pH 7) and 0.1 ml GSSG (oxidised glutathione) was added. The reaction mixture was incubated for 10 min at room temperature followed by the addition of 0.1 ml NADPH. Changes in absorbance for 5 min were recorded at 340 nm [21].
Glutathione Peroxidase (GPx): GPx enzyme activity was measured by the method of Paglia and Valentine [22]. The reaction cocktail was prepared by adding 0.05 ml homogenate, 0.3 ml phosphate buffer, 0.1 ml GSH, 0.05 ml sodium azide, 0.01 ml NADPH, and 0.05 ml glutathione reductase. It was incubated for 10 min at room temperature. After incubation, 0.05 ml H2O2 was added to each tube. Change absorbance was recorded for 5 min. at 340 nm (time scan).
Statistical Analysis
The results were expressed as the mean ± SE (n=6) and the p-value by using the student t-test p<0.05 was considered as significant. One-way ANOVA was used for statistical analysis.
Results
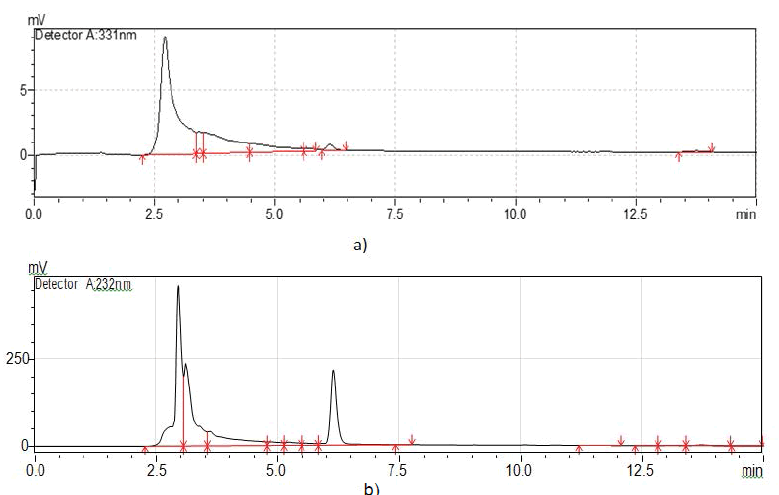
High-Performance Liquid Chromatography (HPLC): Figure 1a of Triticum aestivum showed one peak at 2.7 min which indicates the presence of catechin. HPLC chromatogram of n-butanol extracts of P. betel leaves showed three peaks at 2.9 min chlorogenic acid, at 3.1 min epicatechin, and at 3.5 min 3,4 Dihdroxy benzaldehyde (Figure 1b).
In vivo Study in Haloperidol Induced Iron Deficiency Anaemia
Hematological and ferrokinetic parameters: Table 1 represents the hematological and ferrokinetic parameters in various groups of rats. On day 7 hematological data showed a significant reduction in hemoglobin concentration, RBCs, and hematocrit value as compared to normal control. RBCs count, and hemoglobin concentration was significantly decreased in HP control in comparison to normal control. The combination therapy (TA+PB) showed the highest RBCs count and Hb concentration in comparison to TA and PB therapy. The concentration of serum iron is significantly decreased in HP control in comparison to normal control and increased in therapeutic control. The highest concentration of serum iron was observed in combination therapy (PB+TA). Antianemic activity was evaluated by using phenylhydrazine anemia in rats. On day 7 hematological data showed a significant reduction in hemoglobin concentration, RBC count, and hematocrit value as compared to normal control.
| Blood parameter | Group-I (Normal control) | Group-II (HP control) | Group-III (HP+PB) | Group-IV (HP+TA) | Group-V (HP+PB+TA) |
|---|---|---|---|---|---|
| WBC (10c3/mm3) | 13 ± 0.73 | 9.75 ± 0.93 | 10.26 ± 0.36 | 9.97 ± 0.26* | 12.87 ± 0.49 |
| RBC (10c3/mm3) | 6.13 ± 0.83 | 4.84 ± 0.10# | 5.03 ± 0.30* | 3.5 ± 0.47* | 5.91 ± 0.44 |
| HGB(g/dl) | 15.1 ± .082 | 12.45 ± 0.04# | 13.16 ± 0.24* | 13 ± 0.36 | 13.53 ± 0.32* |
| Serum protein(g/dl) | 38.9 ± 0.24 | 34.4 ± 1.2 | 35 ± 0.18 | 35.8 ± 2.34 | 36.7 ± 0.98 |
| Serum iron (μg/dL) | 50.2 ± 0.12 | 38.4 ± 2.67# | 41.02 ± 2.4 | 40.4 ± 0.45 | 43.1 ± 1.09* |
| TIBC (μg/dL) | 70.23 ± 0.68 | 145.8 ± 0.56 | 65.5 ± 2.06 | 52.3 ± 0.8 | 68.09 ± 1.6 |
| TS (μg/dL) | 29.8 ± 0.92 | 5.9 ± 0.65 | 15.6 ± 0.38 | 10.8 ± 2.06 | 17.6 ± 0.38 |
| Values are mean ± SE, N=5 #p ≤ 0.05 vs. control group, *p ≤ 0.05 vs. HP administered group | |||||
In vivo study in PHZ induced hemolytic anemia
Bodyweight: Table 2 represents the bodyweight of rats. The initial body weight of the rats before being given the toxicant was similar in all groups. At the end of the toxicant, there is a loss in body weight in all groups. After treatment increase in body weight of all groups was observed.
| S. No. | Animals | Weight before toxicant (g) | Weight after toxicant (g) | After therapy (g) |
|---|---|---|---|---|
| 1 | Control | 195 ± 2.3 | 195 ± 1.3 | 200 ± 2.3 |
| 2 | PHZ | 183 ± 1.3 | 154 ± 1.3 | 172 ± 1.1 |
| 3 | TA | 192 ± 1.3 | 162 ± 2.3 | 177 ± 1.1 |
| 4 | PB | 190 ± 2.3 | 165 ± 2.3 | 180 ± 2.3 |
| 5 | TA+PB | 200 ± 2.3 | 180 ± 2.3 | 185 ± 2.3 |
Liver weight: Table 3 depicts the liver weight of rats. The liver weight of toxicant (PHZ) is 4.98 g in comparison to normal is 3.2 g and therapy TA is 4.41 g, PB is 4.64 g and TA+PB is 3.50 g. Combination therapy (TA+PB) liver weight is like normal weight.
| S.No. | Animals | Liver weight (g) |
|---|---|---|
| 1 | Normal | 3.2 ± 0.04 |
| 2 | PHZ | 4.98 ± 0.08 |
| 3 | TA | 4.41 ± 0.04 |
| 4 | PB | 4.64 ± 0.06 |
| 5 | TA+PB | 3.50 ± 0.17 |
Hematological and ferrokinetic parameter: Antianemia activity was evaluated by using phenylhydrazine anemia in rats. On day 7 hematological data showed a significant reduction in haemoglobin concentration, RBCs, and hematocrit value as compared to normal control. Table 4 represents hematological data of normal control (Group I), PHZ control (Group II), and treatment (Group III to V). Comparison of Group III, IV, and V with Group II showed a reduction of haemoglobin concentration, RBCs, and hematocrit value. Group III, IV, V received PB, TA, and PB+TA butanolic extract at doses of 20 mg/Kg body weight orally for 14 days. Comparisons of Group III, IV, and V with Group II showed significant (p<0.05) recoupment in the hematological parameters. Hematological data showed that there was a significant drop in hemoglobin concentrations, RBCs counts, and Hematocrit (HCT) values in the rats on the 7th day. On the other hand, treatment with PB, TA, and PB+TA had significantly reversed the deteriorating effects of PHZ on the values of RBCs, HGB, and HCT at each time point of analysis. Moreover, intravascular hemolysis of RBCs is associated with the release of their hemoglobin with subsequent accumulation of free heme. In support, an increased serum concentration of heme was significantly observed in PHZ-received rats, particularly at 7 days and it was significantly reversed by combination supplementation therapy TA and PB.
| Blood parameter | Group-I (Normal control) | Group-II (PHZ control) | Group-III (PHZ+PB) | Group-IV (PHZ+TA) | Group-V (PHZ+PB+ TA) |
|---|---|---|---|---|---|
| WBC (10c3/mm3) | 7.7 ± 0.73 | 9.75 ± 0.93# | 8.8 ± 0.36** | 8.97 ± 0.26** | 8.77 ± 0.49 |
| RBC (10c3/mm3) | 6.13 ± 0.83 | 2.24 ± 0.10# | 5.83 ± 0.30** | 4.8 ± 0.47** | 6.71 ± 0.44 |
| HGB (g/dl) | 15.1 ± .082 | 5.45 ± 0.04# | 13.06 ± 0.24** | 10.9 ± 0.36** | 13.53 ± 0.32 |
| HCT (%) | 39.8 ± 0.24 | 18.9 ± .081# | 34.53 ± 1.82** | 31.1 ± 0.65** | 35.53 ± 0.94 |
| MCV (µm3) | 53.5 ± 2.04 | 76.67 ± 10.8# | 53.67 ± 3.85 | 59 ± 2.94 | 49 ± 2.94 |
| MCH (pg) | 20.83 ± 0.12 | 24.25 ± 0.85# | 21.03 ± 1.29 | 21.23 ± 1.10 | 17.3 ± 0.89 |
| MCHC | 36.8 ± 0.57 | 28.7 ± 0.12# | 36.7 ± 0.5** | 35.7 ± 0.63* | 35.5 ± 0.85 |
| PLT (10c3/mm/3) | 417.8 ± 2.24 | 329.5 ± 11.9# | 644 ± 2.16** | 367.3 ± 3.85* | 333.3 ± 3.29 |
| Serum iron (μg/dL) | 130 ± 2.11 | 65 ± 0.95 | 73 ± 0.98 | 89 ± 1.04 | 95 ± 0.68 |
| TIBC (μg/dL) | 280 ± 3.24 | 350 ± 3.67 | 224 ± 1.23 | 257 ± 0.98 | 278 ± 2.09 |
| TS (μg/dL) | 40 ± 0.97 | 10 ± 0.04 | 39 ± 0.87 | 29 ± 1.36 | 45 ± 0.63 |
Table 5 represents the oxidative marker enzymes in various groups of PHZ treated rat liver. The TBARS level was estimated in PHZ (toxicant) liver is increased (9.3) in comparison to control (1.5). The TBARS level in treatment groups is decreased i.e. TA (5.8), PB (7.2), and TA+PB (1.8) in comparison to PHZ (9.3). The lowest TBARS level was observed in combination therapy (TA+PB) as compared to TA and PB therapy. GSH level in the PHZ group (3.8) decreased in comparison to the control group (9.3). The GSH level is increased in therapy groups such as TA (7.6), PB (5.9), and TA+PB (7.9). The highest GSH level was observed in the TA+PB therapy group followed by TA. PB therapy was the least effective. Superoxide Dismutase (SOD) level in PHZ toxicant (36.9) is decreased in comparison to control (94.7). In the therapy group i.e. TA (39.8), PB (90.3), and TA+PB (91.5) the enzyme level recouped when compared to PHZ. The highest SOD level was observed in combination therapy TA+PB (91.5) followed by Piper betel (90.3) therapy. Catalase (CAT) level in PHZ toxicant decreased in comparison to control. In treatment groups, TA (66.5), PB (38.5), and TA+PB (54.7) catalase levels increased towards control. The highest catalase level was observed in TA therapy followed by a combination of TA+PB therapy 54.7. Glutathione-S-Transferase (GST) level declined in the PHZ group (3.7) in comparison to the control (7.3). In the treatment group, GST levels were recouped with TA (6.9), PB (6.8), and TA+PB (7.2) in comparison to PHZ. The highest GST level was observed in the TA+PB group. Glutathione Reductase (GR) level is decreased in the PHZ group as compared to the control. In the therapy group, the GST level recovered the highest GST level near control was observed in the TA+PB group. Glutathione Peroxidase (GPx) level decreased in experimental control and was 1.5 in comparison to control which was 5.4. In the therapy group, the GPx level increased with TA (4.7), PB (3.3), and TA+PB (5.7) in comparison to PHZ. The highest GST level was observed in the TA+PB group followed by TA therapy. PB therapy was the least effective.
| S. No. | Name of the parameter | Control Group I | PHZ Group II | PHZ+TA Group III | PHZ+PB Group IV | PHZ+PB+TA Group V |
|---|---|---|---|---|---|---|
| 1 | Lipid Peroxidation (LPO) micro mole/L | 1.57 ± 0.4 | 9.3 ± 0.71# | 5.8 ± 0.41 | 7.29 ± 0.62 | 1.87 ± 0.56* |
| 2 | Reduced Glutathione (GSH) IU/L | 9.35 ± 0.72 | 3.89 ± 0.29# | 7.68 ± 0.6 | 5.99 ± 0.42 | 7.97 ± 0.65* |
| 3 | SOD IU/L | 94.37 ± 8.9 | 36.97 ± 2.8# | 39.8 ± 2.7 | 90.33 ± 8.8 | 91.5 ± 8.8* |
| 4 | Catalase IU/L | 71 ± 0.59 | 18 ± 0.9# | 66.5 0.56 | 38.5 ± 0.35 | 54.75 ± 0.48 |
| 5 | Glutathione-S-Transferase (GST) IU/L | 7.35 ± 0.68 | 3.74 ± 0.25# | 6.97 ± 0.58 | 6.88 ± 0.57 | 7.28 ± 0.69 |
| 6 | Glutathione Reductase (GR) IU/L | 6.52 ± 0.59 | 1.55 ± 0.6 | 4.7 ± 0.3 | 3.3 ± 0.24 | 5.7 ± 0.44 |
| 7 | Glutathione peroxidase (GPx) IU/L | 5.4 ± 0.35 | 1.55 ± 0.42 | 4.7 ± 0.38 | 3.37 ± 0.29 | 5.7 ± 0.48 |
Discussion
Phenyl hydrazine is a powerful oxidant. Its reactive metabolites namely “phenyldiazene,” “phenylhydrazyl radical,” and “benzene diazonium ion” undergo automatic systematic oxidation that causes damage to RBCs by virtue of oxidizing hemoglobin [23].
Thus, prevention of such oxidation of hemoglobin could be a skillful strategy against phenyl hydrazine-induced hemolytic anemia. The antianemic potential of extracts has been established in earlier studies [24,25]. Phenyl hydrazine produces both aryl and hydroxyl radicals when incubated with rat liver microsomes and oxidized by hydrogen peroxide at pH 7.4 and at 37°C where the involvement of superoxide hydroxyl and phenyl radicals in PHZ induced toxicity has been proposed [26,27].
Our body has an effective defense system against free radical-induced damage. It consists of a set of endogenous antioxidant enzymes, which is Catalase (CAT), Superoxide Dismutase (SOD), Glutathione Peroxidase (GPx), etc. Regarding non-enzymic antioxidants, reduced glutathione (GSH) is a critical determinant of tissue susceptibility to oxidative damage. It is an intracellular reductant that is extensively found in cells. It protects cells against electrophilic attacks by xenobiotics such as free radicals’ peroxides.
The level of lipid peroxidation is a measure of membrane damage alterations in its structure-function. In the present study, the level of lipid peroxidation was significantly decreased in combination therapy (TA+PB) in comparison to the toxicant (PHZ) group. This study is supported by Naskar, et al. where the level of MDA, which is one of the end products of lipid peroxidation in liver tissue, was found to be high in the CCl4 control group [2]. It indicates enhanced lipid peroxidation leading to tissue damage failure of antioxidant defense mechanisms against free radicals.
The ability of GST to alter the level of intracellular GSH in the liver in response to the generation of ROS in the protection of cells against free-radicals-inducing agents [27]. GSH serves as an oxygen radical scavenger and stabilizes the biological membrane. The deficiency of cellular GSH increases prooxidant production. In the present study, the GSH level is significantly decreased in toxicant group. Ohta, et al. reported that a significant decrease was observed in the GSH content of the liver in mice, which were injected with CCl4 [28].
Within mammalian tissues, the most significant antioxidant is Superoxide Dismutase (SOD), which catalyzes the dismutation of superoxide (O2 .), an oxygen radical that is released in inflammatory pathways and causes connective tissue breakdown. In the present study SOD level is significantly increased in combination therapy (TA+PB) and decreased in toxicant-induced subjects. The decrease in the liver SOD activity is possibly an expected result that occurs due to lipid peroxyl radicals and from the inactivation of their destruction products.
Catalase is one of the important enzymes in the supportive team of defense against Reactive Oxygen Species (ROS). Catalase is a hemoprotein containing four haem groups that catalysis the decomposition of H2O2 to water and O2 and thus, protects the cell from oxidative damage by H2O2 and OH [29].
Cellular glutathione and related enzymes such as glutathione peroxidase, glutathione S-transferase and glutathione reductase are among the principal protective mechanisms against endogenous and exogenous toxic substances and free radical-mediated damage in liver tissue as well as in other tissues [30]. The GST level is significantly increased in combination therapy. The GR level is significantly increased in TA and TA+PB therapy. The GPx level is significantly increased in TA, PB, and TA+PB therapy in comparison to the toxicant group.
Conclusion
In the present study, the evaluation of n-butanol extract of T. aestivum grass (TA) and P.betel leaves (PB) and combination (TA+PB) showed the significant reversal effect against haloperidol and PHZ induced toxicity. In all three therapies, combination therapy (TA+PB) showed the highest hepatoprotective, antianemic, and antioxidant effects against PHZ toxicants.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
Acknowledgment
The authors are highly obliged to Madhya Pradesh Council of Science and Technology, Bhopal (MPCST) (No 1117/ CST/R&D(BS)2016) for providing financial assistance for carrying out the work. The authors are also thankful to ITM University for providing lab and animal house facility. The support from the Central Instrumentation facility of Jiwaji University, Gwalior is highly acknowledged.
References
- Venukumar, M. R., and M. S. Latha. "Antioxidant activity of curculigo orchioides in carbon tetrachloride-induced hepatopathy in rats." Indian Journal of Clinical Biochemistry, Vol. 17, No. 2, 2002, pp. 80-87.
- Naskar, S., et al. "In vitro and in vivo antioxidant potential of hydromethanolic extract of Phoenix dactylifera fruits." Journal of Scientific Research, Vol. 2, No. 1, 2010, pp. 144-57.
- Borneo, R., et al. "Antioxidant capacity of medicinal plants from the Province of Córdoba (Argentina) and their in vitro testing in a model food system." Food Chemistry, Vol. 112, No. 3, 2009, pp. 664-70.
- Jollow, David J., and David C. McMillan. "Oxidative stress, glucose-6-phosphate dehydrogenase and the red cell." Biological Reactive Intermediates VI, Vol. 500, 2001, pp. 595-605.
- Murphy, Michael E., Heiner Scholich, and Helmut Sies. "Protection by glutathione and other thiol compounds against the loss of protein thiols and tocopherol homologs during microsomal lipid peroxidation." European Journal of Biochemistry, Vol. 210, No. 1, 1992, pp. 139-46.
- Peng, R. X., et al. "Glutathione-related enzyme activities in human fetal adrenal, liver, and kidney." Acta Pharmacologica Sinica, Vol. 19, No. 2, 1998, pp. 167-71.
- Tirgar, P. R., B. L. Thumber, and T. R. Desai. "Isolation, characterization and biological evaluation of iron chelator from Triticum aestivum (wheat grass)." International Journal of Pharma and Bio Sciences, Vol. 2, 2011, pp. 288-96.
- Hanninen, Otto, et al. "Vegan diet in physiological health promotion." Acta Physiologica Hungarica, Vol. 86, No. 3-4, 1999, pp. 171-80.
- Jeng, Jiiang-Huei, et al. "Modulation of platelet aggregation by areca nut and betel leaf ingredients: Roles of reactive oxygen species and cyclooxygenase." Free Radical Biology and Medicine, Vol. 32, No. 9, 2002, pp. 860-71.
- Singh, Meghna, et al. "The n-hexane and chloroform fractions of Piper betle L. trigger different arms of immune responses in BALB/c mice and exhibit antifilarial activity against human lymphatic filarid Brugia malayi." International Immunopharmacology, Vol. 9, No. 6, 2009, pp. 716-28.
- Dasgupta, Nabasree, and Bratati De. "Antioxidant activity of Piper betle L. leaf extract in vitro." Food Chemistry, Vol. 88, No. 2, 2004, pp. 219-24.
- Majumdar, Biswajit, et al. "Potent antiulcerogenic activity of ethanol extract of leaf of Piper betle Linn by antioxidative mechanism." Indian Journal of Clinical Biochemistry, Vol. 17, No. 1, 2002, pp. 49-57.
- Celeghini, Renata, Janete HY Vilegas, and Fernando M. Lancas. "Extraction and quantitative HPLC analysis of coumarin in hydroalcoholic extracts of Mikania glomerata Spreng:(" guaco") leaves." Journal of the Brazilian Chemical Society, Vol. 12, No. 6, 2001, pp. 706-09.
- Ben‐Shachar, Dorit, and Moussa BH Youdim. "Neuroleptic‐induced supersensitivity and brain iron: I. iron deficiency and neuroleptic‐induced dopamine D2 receptor supersensitivity." Journal of Neurochemistry, Vol. 54, No. 4, 1990, pp. 1136-41.
- Yeshoda, K. M. "Phenylhydrazine anaemia in rats." Current Science, Vol. 11, No. 9, 1942, pp. 360-63.
- Sharma, S. K., and CR Krishna Murti. "Production of lipid peroxides by brain." Journal of Neurochemistry, Vol. 15, No. 2, 1968, pp. 147-49.
- Brehe, Jacqueline E., and Helen B. Burch. "Enzymatic assay for glutathione." Analytical Biochemistry, Vol. 74, No. 1, 1976, pp. 189-97.
- Marklund, Stefan, and Gudrun Marklund. "Involvement of the superoxide anion radical in the autoxidation of pyrogallol and a convenient assay for superoxide dismutase." European Journal of Biochemistry, Vol. 47, No. 3, 1974, pp. 469-74.
- Aebi, H. "Catalase in vitro." Methods in Enzymology, Vol. 105, 1984, pp. 121-26.
- Habig, William H., Michael J. Pabst, and William B. Jakoby. "Glutathione S-transferases: The first enzymatic step in mercapturic acid formation." Journal of Biological Chemistry, Vol. 249, No. 22, 1974, pp. 7130-39.
- Tayarani, Ivan, et al. "Antioxidant enzymes and related trace elements in aging brain capillaries and choroid plexus." Journal of Neurochemistry, Vol. 53, No. 3, 1989, pp. 817-24.
- Paglia, Donald E., and William N. Valentine. "Studies on the quantitative and qualitative characterization of erythrocyte glutathione peroxidase." The Journal of Laboratory and Clinical Medicine, Vol. 70, No. 1, 1967, pp. 158-69.
- Berger, Josef. "Phenylhydrazine haematotoxicity." Journal of Applied Biomedicine, Vol. 5, No. 3, 2007, pp. 125-30.
- Johri, S., and N. Khan. "In vitro antioxidant and antihaemolytic potential of Triticum aestivum grass." International Journal of Complementary & Alternative Medicine, Vol. 9, No. 5, 2017, p. 00310.
- Johri, Sonia, Neha Khan, and Nasir Khan. "Phytochemical screening, biochemical estimations and spectroscopic analysis of various extracts of Piper betel leaves." International Journal of Pharma Research and Health Sciences, Vol. 5, No. 6, 2017, pp. 1939-44.
- Hill, H. A. O., and P. J. Thornalley. "Phenyl radical production during the oxidation of phenylhydrazine and in phenylphydrazine‐induced haemolysis." FEBS Letters, Vol. 125, No. 2, 1981, pp. 235-38.
- Sherman, Morris, et al. "Glutathione S‐transferase in human hepatocellular carcinoma." Hepatology, Vol. 3, No. 2, 1983, pp. 170-76.
- Ohta, Yoshiji, et al. "Therapeutic effect of melatonin on carbon tetrachloride‐induced acute liver injury in rats." Journal of Pineal Research, Vol. 28, No. 2, 2000, pp. 119-26.
- Tolbert, N. E. "Metabolic pathways in peroxisomes and glyoxysomes." Annual Review of Biochemistry, Vol. 50, No. 1, 1981, pp. 133-57.
- Hayes, John D., and Lesley I. McLellan. "Glutathione and glutathione-dependent enzymes represent a co-ordinately regulated defence against oxidative stress." Free Radical Research, Vol. 31, No. 4, 1999, pp. 273-300.