Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 4
Evaluation of the In-patient Therapeutic Feeding Program Used for Children Admitted with Severe Protein Energy Malnutrition in El-Obied Specialized Pediatric Hospital
Najlaa Adam Musa1 and Alam Eldin Musa Mustafa2,3*2Department of Pediatrics, Faculty of Medicine and Health Sciences, University of Kordofan, Sudan
3Department of Child Health, College of Medicine, King Khalid university, Abha, Saudi Arabia
Alam Eldin Musa Mustafa, Department of Child Health, College of Medicine, King Khalid university, Abha, Saudi Arabia, Email: alameldinmustafa641@gmail.com
, DOI: o
Abstract
This hospital-based retrospective analytical study was done during the year 2018 in El-Obied specialized pediatric hospital in Sudan and included the 296 children under the age of 5 years who were admitted to the inpatient center for treating acute severe malnutrition. This center is the main center in the whole state of Kordofan in Sudan with under 5-year children in the whole state approaching about 700,000 children. The center is a very crowded center containing only 25 beds with sometimes more than one patient on the same bed. The objectives of the study were to evaluate the use of the standard protocol of inpatient management of severe malnutrition in this center which is under the supervision of the federal and state ministry of health and also to assess aspects of the duration of therapy and outcome of management. A prepared questionnaire was used to fill in all information about the patient’s nutritional and clinical condition on admission and with a concentration on the nutritional management and follow up during the hospital stay and the outcome of the hospital management. All the necessary information was obtained using the designed WHO register for inpatient treatment of severe malnutrition in children; the CCP (Critical Care Pathway register). Ethical approval and hospital and Ministry of health permissions were obtained. The results show that most of the patients (80%) were in the younger age group of 6-24 months and 72% have a z-score less than 3SD with 87.5 sufferings severe wasting and 75.7% having a MUAC indicating severe wasting. Nutritional edema was detected in 24.3% on admission diarrhea in 60.8% and signs of vitamin A deficiency in 68.2% F-75 were the starter feeding for all children in the group and appetite test performed in all. Most of the children did not take the proper prescribed amount of F-75 and 30.7% of those with diarrhea were not given re-so-mal. About 85% of patients took more than 3 days to transfer to F-100 milk. And about 55% stayed in the hospital for 8-14 days. The mortality rate was 5.4% and the escape from inpatient care was high at 12.5%. The rest of the patients were referred for outpatient care. Significant relationships were found with the presence of diarrhea and the duration of hospital stay.
The study recommended improvements in some of the parts of protocol implementation like giving re-so-mal to all patients with diarrhea and addressing the problem of escaping from hospital treatment. Also, to raise the number of acting nutritionists in the center and to improve both under and postgraduate training in nutritional therapy of SAM for all of the health personnely.
Keywords
Severe Acute Malnutrition (SAM), Inpatient therapeutic feeding, z-score, F-75 and F-100, Edematous malnutrition, Severe wasting, Mid-Upper Arm Circumference (MUAC)
Introduction
Adequate nutrition is essential in early childhood to ensure healthy growth, proper organ formation and function, a strong immune system, and neurological and cognitive development. Malnutrition defined as underweight is a serious public-health problem that has been linked to a substantial increase in the risk of mortality and morbidity.
Child malnutrition was associated with 54% of child deaths (10.8 million children) in developing countries in 2001 [1-3]. In Sudan, the treatment of malnutrition problems in children of fewer than five years of old is prone to a unique protocol. Undernutrition often used interchangeably with malnutrition, results primarily from inadequate intake of dietary energy but may also be caused by infections that limit the absorption of key nutrients [4-6]. Acute malnutrition is the most visible form of malnutrition and is typified by severe wasting (disproportional weight for height) and/or edema (the retention of fluid). Acute malnutrition can lead to reductions in age-appropriate growth, depressed immune functioning, fluid overload, heart failure, infection, and death [1,7]. Chronic malnutrition is the result of inadequate nutrition over a long period and is not always as visible as acute malnutrition. It can begin in the uterus with poor maternal nutrition and persists through inadequate feeding practices and suboptimal food quality [8]. Malnutrition is among the four leading causes of child mortality around the globe. In 2013, the World Health Organization (WHO) reported malnutrition was linked to 45% of all childhood deaths [9]. Malnutrition is a contributing factor in the deaths of 60.7% of children diagnosed with diarrheal diseases,57.3% of deaths associated with malaria, 52.3% deaths associated with pneumonia, and 44.8% of deaths from measles [10]. The UN Standing Committee on Nutrition estimated 26.5% of children in developing countries were stunted in 2005 and one year later, the United Nations Children’s Fund (UNICEF) reported South Asia had a 46% prevalence of stunting in children under five. Children are particularly vulnerable to malnutrition during the first 1,000 days following conception [11].
Inadequate nutrition during this period can lead to delayed and impaired cognitive and physical development [11,12]. This malnutrition-based damage is largely irreversible and can lead to poor school and work achievement and an increased risk for developing diseases later in life [8]. In 2007, the International Child Development Steering Group found that children raised with limited access to nutritional resources were less likely to be socially and economically productive adults [13]. This finding supported the inextricable link between childhood malnutrition and poverty later in life [13]. Usually, there is not one single cause of malnutrition, but various factors at both the individual and communal levels contribute. At the most fundamental level, a body becomes malnourished when it does not obtain a sufficient quantity and/or quality of food and nutrients. In addition to water, six different nutrient groups are critical for the body to sustain itself and grow: proteins, carbohydrates, minerals (e.g., zinc, calcium, and sodium), fats, vitamins, and indigestible and non-absorbable particles such as fiber [13,14]. In children, repeated bacterial infections flatten intestinal linings, reducing the body’s ability to absorb nutrients by 33%, as well as decrease levels of normal digestive bacteria [15].
Feeding the child with RUTF
RUTF is an energy-dense, mineral/vitamin-enriched food that is equivalent to F-100. RUTF is an integral part of Outpatient Care.
ReSoMal is a modification of the standard or low-osmolality Oral Rehydration Solution (ORS) recommended by the World Health Organization (WHO). ReSoMal contains less sodium, more sugar, and more potassium than standard ORS and is intended for children with SAM with diarrhea [16,17].
Daily Care Treatment for an inpatient severely mal-nourished child should include also these four important daily care treatments giving ReSoMal lowly, giving antibiotics prescribed, giving folic acid, and giving vitamin A if needed [18].
Materials and Methods
Study Area
This study area was conducted in El-Obeid Pediatric Specialized Hospital, El-Obeid, Sheikan, locality, North Kordofan state, Sudan during the period January to December 2018.
Sample Collection
A 296 of severe acutely malnourished are selected randomly from the records of El-Obeid Pediatric Specialized Hospital. The chosen patients were selected according to Krejcie and Morgan Equation (1970) for every month (January-December, 2018).
Data Collection
Primary data: Primary data were collected from the records of the Hospital. A questionnaire was designed to collect such information from the records of the selected patients some anthropometric measurements were also recorded from the records of selected patients both at the admission and discharge periods. Secondary data were collected from comparable previous studies, references, and internet networks.
Anthropometric measurement: was taken by the trained nutritionists in the ward as follows
Weight: The weights of the patients were recorded in Kg at admission and discharge using the Solar Electronic Scale.
Height/Length: The heights of the patients were measured in cm at the admission period using the length board. If the child is less than 2 years old (or less than 87 cm height if the age is not available) or unable to stand, recumbent length was measured. But if the child is aged 2 years or older and able to stand, standing height was measured.
Weight for Height (z-score): A z-score is a way of comparing a measurement; in this case, a child’s WFH, to an ‘average’ (median). The ‘averages’ used are the WHO 2006 child growth standards (WHO standards) In the WHO standard population, all children of the same height are distributed around the median weight, some heavier and some lighter. For each height group, there is a standard deviation among the children of the WHO standard population. This standard deviation is expressed as a certain number of kilograms at each height. The z-score of a child being measured is the number of standard deviations the child is away from the median weight of the WHO standard population at that height group. Find the child’s length or height in the middle of the table.
If the length or height is between those listed, round up or down as follows: If the height/length is 0.5 cm or greater than the next lower height/length, round up. Otherwise, round down. Then look in the left columns for boys or the right columns for girls to find the child’s weight. Look at the top of the column to see what the child’s z-score is. The child’s weight may be between two z-scores. If so, indicate that the weight is between these scores by writing less than (<). For example, if the score is between 1 z-score and 2 z-score, write <1 z-score.
Mid Upper Arm Circumference (MUAC): MUAC was taken on the left arm. The length of the child’s upper arm, between the bone at the top of the shoulder and the tip of the elbow is measured. The midpoint of the upper arm was determined. The MUAC tape was being wrapped around the child’s arm. For numbered tapes, the end of the tape was fed through the first opening and then through the third opening. The measurement was read from the middle window where the arrows point inward. The end was then sliding through the first opening and then through the second opening. The color was read through the window at the point the two arrows indicate.
Statistical Analysis
The results were analyzed using Statistical Packaging for Social Sciences (SPSS), software; version 16 (frequency, percentage, and cross-tabulation). The results were presented in tables and figures. Some of the results were analyzed by cross-tabulation between two specific factors using the Chi-Square Test (test of independence).
Ethical Consideration
The Administration and Scientific Council of Elobeid Specialized Pediatric Hospital approved the ethical consideration of this research on 20 November 2018.
Results
A total of 296 patients were enrolled in this hospital-based study. The patient’s age categories in the study ranged as follows (6-24), (25-42), and (43-59) months were found to be 80.1%, 18.6%, and 1.4% respectively.
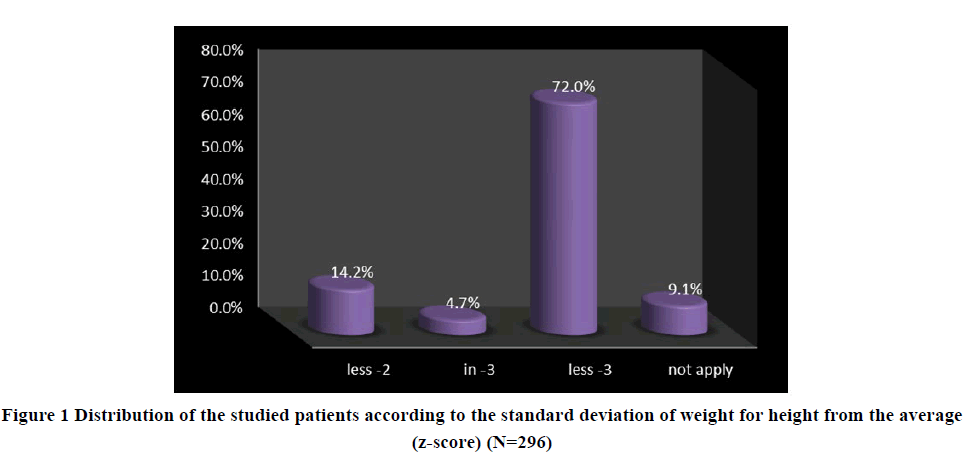
Weight for the height of patients (Z-score): The Z-scores of 14.2% of the patients were less than 2 (<2), 4.7% were in 3, 72.0% were less than 3, and 9.1% of the patients were not applied due to the existence of edema. The majority of the patients (72.0%) were suffered from severe acute malnutrition with a z-score less than 3 SD (Figure 1). The weight for height was found to have a significant association with taking breast milk in children below 2 years in this study group (p-value 0.005).
MUAC of patients at Admission: Those not applicable for MUAC measurements were had edema. Most of the patients (75.7%) were severe acutely malnourished.
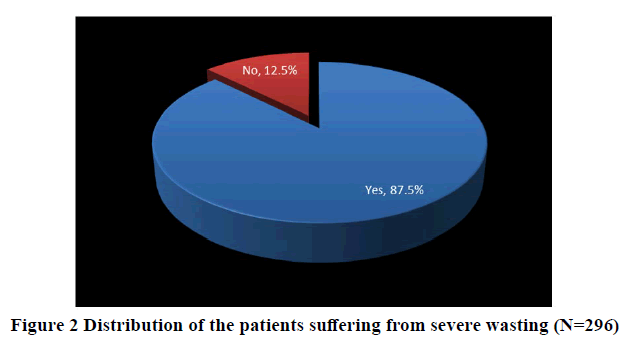
Patients suffering from severe wasting: 87.5% of the patients suffered from severe wasting as a consequence of malnutrition, while 12.5% of them did not suffer (Figure 2).
Patients suffering from edema: (24.3%) suffered some grade of edema (edematous malnutrition) (Table 1). This result may explain that the affected children suffered from marasmus more than Kwashiorkor. And also, may be attributed to insufficient intake of food or early cessation of breastfeeding. The relationship between child age and the presence of edema was statistically significant (p-value 0.007). The presence of edema was found to have no significant relationship with the standard outcome of inpatient management (p-value 0.192).
| Frequency | Percent | |
|---|---|---|
| 0 | 224 | 75.7 |
| grade + | 26 | 8.8 |
| grade ++ | 18 | 6.1 |
| grade +++ | 28 | 9.5 |
| Total | 296 | 100.0 |
Signs of Vitamin A deficiency: Were seen in 68.2% of the affected children. According to the WHO inpatient protocol of management of SAM; all children with SAM without eye signs of vitamin A deficiency or recent measles will receive vitamin A after 4 weeks in treatment or upon discharge. Also, children with edema will receive vitamin A after the edema has completely subsided.
Giving Folic Acid: 91.9% of the patients had been given folic acid at admission, besides 8.1% of them received no folic acid dose.
As the results reported, 35.5% of the targeted patients were not breastfed, 44.6% breastfed, and 19.9% of them were not breastfed because their ages were over two years.
The results of the research showed that all targeted patients had been started feeding with F-75 milk. The results of the study also reported that all of the affected children 100% received F-75milk prescribed according to their weights at the admission time till the stabilization was reached (Table 1). 60.8% of the patients reported that they were affected with diarrhea on their admission. The results showed, 69.3% of the patients who suffered from diarrhea or vomiting had been given ReSoMal. On the other hand, the remaining 30.7% of the patients were not given ReSoMal. The presence of diarrhea has a strong statistical relationship with the duration of hospital stay (Table 2).
| Diarrhea | The period of staying in the hospital | Total | |||
|---|---|---|---|---|---|
| 1-7 days | 8-14 days | 15-21 days | more than 21 days | ||
| No | 44 | 58 | 12 | 2 | 116 |
| Yes | 36 | 104 | 37 | 3 | 180 |
| Total | 80 | 162 | 49 | 5 | 296 |
The duration of hospital stays: According to the results of the research, the patients who had to stay in the hospital between 1-7 days were (27%) of the patients, between 8-14 days were (54.7%), between 15-21 days were (16.5%), but only (1.7%) of the patients had been staying more than 21 days (Table 3).
| Frequency | Percent | |
|---|---|---|
| 1-7 days | 80 | 27 |
| 8-14 days | 162 | 54.7 |
| 15-21 days | 49 | 16.6 |
| more than 21 days | 5 | 1.7 |
| Total | 296 | 100 |
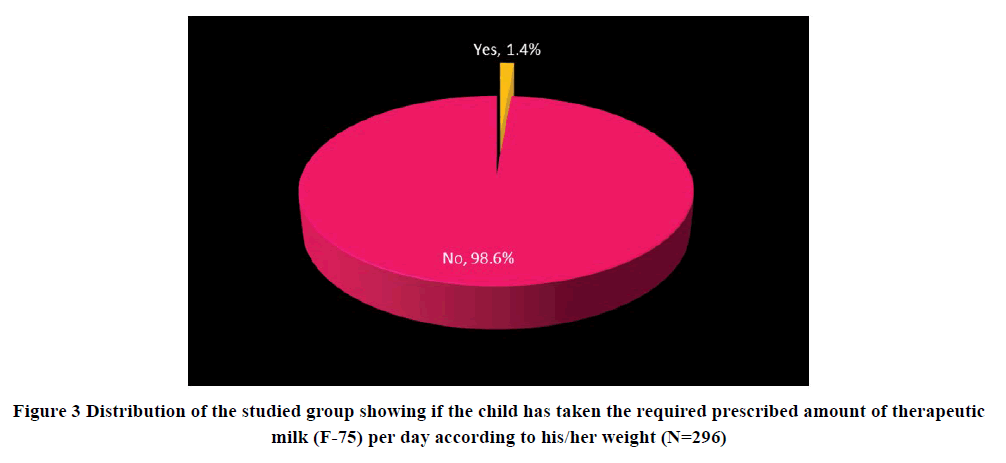
Transference of patients from F-75 to F-100: 84.8% of the patients took more than 3 days to be transferred from F-75 to F-100 milk, on other hand 15.2% of them transferred during the period of 2 to 3 days. This long-staying in F-75 could be attributed to insufficient therapeutic milk taken given to the patients before the transference, as only 1.4% of the malnourished children took their prescribed amount (Figure 3). Despite that, no significant statistical relationship was found between taking a lesser amount of therapeutic milk and the overall duration of hospital stay (Table 4) (p-value 0.270) but a significant relationship was found between taking the proper amount of F-75 and duration of stay (p=0.000).
Appetite Test: The results of the research revealed that the appetite was tested for all of the patients before giving the therapeutic food (RUTF).
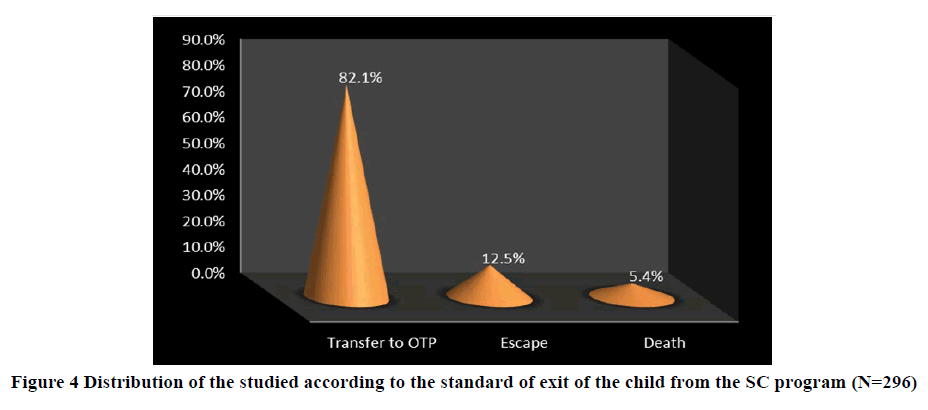
The Standard of patients exit: As regards the results of this study as shown in Table 4, 12.5% of the patients escaped from stabilizing center, 5.4% died and the rest (82.1%) were transferred to outpatient centers (OTP) (Figure 4). presence of vitamin A deficiency signs and diarrhea did not affect the standard outcome in this study group (p-values 0.133 and 0.976 respectively). The feeding plan has a significant statistical relationship with the standard outcome in the group (p-value 0.001). The duration in days for the transition from F-75 to F-100 has no significant statistical relation with the standard outcome of management (Table 5) (p-value 0.942).
| Amount of milk per/day | The period of staying in the hospital | Total | |||
|---|---|---|---|---|---|
| 1-7 days | 8-14 days | 15-21 days | more than 21 days | ||
| No | 80 | 160 | 47 | 5 | 292 |
| Yes | 0 | 2 | 2 | 0 | 4 |
| Total | 80 | 162 | 49 | 5 | 296 |
| Transfer to F100 | Standard of exit | Total | ||
|---|---|---|---|---|
| Escape | OTP | death | ||
| 2-3 days | 6 | 37 | 2 | 45 |
| More than 3 days | 31 | 206 | 14 | 251 |
| Total | 37 | 243 | 16 | 296 |
Discussion
This is a hospital-based analytical study on the evaluation of the use for the inpatient management protocol which was developed by the WHO for reduction of both mortality and morbidity due to acute severe malnutrition the study was conducted in El-Obied specialized pediatric hospital center for treating SAM (severe acute malnutrition) [3,16,17,19,20]. Severe Acute Malnutrition (SAM) focuses on the severe form of acute malnutrition, SAM, which is a nutrition condition defined by severe wasting (thinness) and/or presence of bilateral pitting edema. The milder form of acute malnutrition, Moderate Acute Malnutrition (MAM), is defined by moderate wasting. A child with SAM is highly vulnerable to illness and has a high mortality risk. A medical complication in the presence of SAM further increases the risk of death and needs immediate specialized Inpatient Care Clinical signs and anthropometric indicators are used to determine whether or not a child has SAM and should be admitted for treatment, and whether the child should be treated in Outpatient Care or Inpatient Care.
A medical complication in the presence of SAM further increases the risk of death and needs immediate specialized Inpatient Care [16]. All children with SAM and poor appetite (failed the appetite test) and/or medical complications should be admitted for treatment of SAM in Inpatient Care. Children with SAM and medical complications are in danger of death from hypoglycemia, hypothermia, fluid overload, and undetected infections.
Infants under 6 months with acute malnutrition should all be treated in Inpatient Care. Children over 6 months of age but with a weight less than 4 kg should also be treated in Inpatient Care [17,19,20]. Breastfeeding has an important role in the prevention of different forms of childhood malnutrition, including wasting, stunting, over and underweight, and micronutrient deficiencies [21]. Early and sudden weaning methods were seen as risk factors in a considerable percentage of this study group and should be addressed by the health workers in the area.
According to this study it was found in the hospital the treating team generally follow well the two phases of inpatient treatment as it is recommended that patients meeting regionalized anthropometric admission criteria should undergo two treatment phases:
Phase 1: Includes intensive care designed to stabilize patients and prevent further status degradation using nutritional supplementation, including fortified milk and meals, and lasted until a patient’s appetite returned and edema was eliminated. F-75 is the ‘starter’ therapeutic formula milk to use during initial management, beginning as soon as possible and continuing for 2-7 days until the child is stabilized. The child will be offered a total of 130 ml/kg/day of F-75. This amount of F-75 will give the child 100 kcal/kg/day and 1-1.5 g protein/kg/day. The feeding of a child with F-75 could be orally or by nasogastric tube, if necessary [22,23].
Phase 2: Involves rehabilitation and supplementary feedings to improve the patient’s nutritional status before discharge [24]. When the child has stabilized, one can begin to offer F-100, the higher calorie, higher protein “catch up” feed intended to rebuild wasted tissue. Eventually, the child will be offered F-100 freely. F-100 contains more calories and protein: 100 kcal and 2.9 g protein per 100 ml.
The protocol for admission criteria was found to be followed in this center to a good extent although areas for improvement of protocol implementation are also required. All of the children admitted fulfilled one or more of the admission criteria [16,17]. The information about the clinical and measurement findings of each child was registered on the CCP (Critical Care Pathway record that is filled to all patients admitted) although some of the follow-up information was missed in some children [16,17,19,20]. Also, the feeding plan was put, the appetite test was performed in all suitable patients, and 100% of the children were started with the F-75 prescribed properly but unfortunately, most of the children do not take the whole prescribed amount during the day [22,23,25]. Other criteria and signs to recognize in the admission of children with SAM were also used in the hospital these include recognition of the following; clinical signs, anthropometric indicators, and presence of medical complications to determine whether or not a child has SAM and should be admitted for treatment [16,17]. The clinical signs associated with severe acute malnutrition include the following [16,17].
• Visible Severe Wasting with a prominence of body bones
• Various degrees of nutritional bilateral pitting edema
• Poor Appetite (failed appetite test) A child passes the appetite test if he or she eats an adequate amount of RUTF provided in an adequate environment within half an hour [16,17,19,20]
• Eye signs representing eye infection and/or vitamin A deficiency differing in severity
• The medical complications in the presence of SAM that need immediate medical intervention are anorexia, poor appetite-intractable vomiting, convulsions-lethargy, not alert, unconsciousness-hypoglycemia,-high feverhypothermia, Severe dehydration-lower respiratory tract infection, severe anemia-eye signs of vitamin A deficiency, and skin lesion [19,20]. Most malnourished children are not diagnosed until a health crisis, such as an infection, leads them to seek medical attention
There are four methods to assess a person’s nutritional status: anthropometry, biochemical assessment, clinical assessment, and dietary intake assessment anthropometric indicators are commonly used to objectively and promptly classify the nutritional condition of children and are therefore used as key criteria for admission to treatment (and discharge) [16,17,19]. These include Mid-Upper Arm Circumference (MUAC) used for children between 6 to 59 months, weight, length or height, and body mass index Also Weight for height z-Score to expected values for a person of the same sex and age [16,17,19,20].
A z-score is a way of comparing a measurement, in this case, a child’s WFH, to an ‘average’ (median). The ‘averages’ used are the WHO 2006 child growth standards (WHO standards) (Table 6).
It is critical to keep these children in Inpatient Care until the medical conditions have stabilized and are resolving and the appetite has returned. Any health problem and infection should be treated while in Inpatient Care [16].
The protocol for admission criteria was found to be followed in this center to a good extent although areas for improvement of protocol implementation are also required. All of the children admitted fulfilled one or more of the admission criteria [16,17]. The information about the clinical and measurement findings of each child was registered on the CCP (critical care pathway register) although some of the follow-up information was missed in some children [16,17,19,20]. Also, the feeding plan was put, the appetite test was performed in all suitable patients and 100% of the children were started with the F-75 prescribed appropriately but unfortunately, most of the children do not take the whole prescribed amount during the day.
Comparing with a similar study done in the capital of Sudan; Khartoum In Al-Turkey hospital on admitted children with SAM poor adherence to the WHO protocol was found z-scores not measured in more than 61% of patients; edema, mid-upper arm circumference, and z-score were neglected as tools of classification. Blood sugar, hemoglobin concentration, and malaria film/rapid diagnostic tests were the only requested tests Appropriate treatment was documented in 68 (40.2%) children for Intravenous (IV) dextrose for hypoglycemia, and 25 (14.8%) for kangaroo technique, 32 (18.9%) covering with a blanket for hypothermia, 106 (62.7%) for F-75 milk formula and 115 (68%) for F100 milk formula feeding; and there were no records of receiving oral/IV rehydration. The case fatality rate was 5.9%, which is lower than in this study may be due to more severe forms of malnutrition seen in the states [26].
A study in Ethiopia showed good adherence to the WHO protocol inpatient management of SAM children but higher default from treatment [27], while a comparative study was done in Colombia showed that application of the WHO program for one group with SAM has significantly improved their response to treatment and the study recommended the implementation of the protocol in the countries with a high prevalence of childhood malnutrition [28].
Still, there is a high level of defaulting and stopping the therapy and escaping of the mother taking her child before completion of the management. The death rate of 5.4% is within the acceptable WHO rate of inpatient SAM mortality but this does not include those who escape the full treatment program [9,10].
Recommendations
It is highly recommended to strengthen the availability and quality of the treating personnel in this center as it is the largest center for inpatient management of SAM in the whole Kordofan states in Sudan and SAM is a very major contributor to under 5 years child mortality in the country. That support must be through the governmental provision and supply with more nutritional therapists to cover the day and night shifts and also with collaboration with the UNICEF in Sudan and the federal and state ministry of health to provide extensive training on the program to the whole health workers in the state about the inpatient and outpatient detection and management of acute severe malnutrition in children [29]. The escape rate from therapeutic feeding and medical protocol is high and the underlying social and other factors including overcrowding in the center should be seriously addressed to improve the overall outcome of the inpatient care for SAM in the whole state [29].
Inclusion of the CMAM and SAM management training during the undergraduate study of the medical students and health staff is very important to raise awareness and develop the later practice in this section.
The ccp form filling although is satisfactory but needs improvement especially in the follow-up part and this should be taken into consideration.
It is essential to give re-so-mal to all children with SAM admitted to inpatient care which was not fully applied in this center and this may increase the duration of hospital stay. Also, it should be assured that the precise amount of prescribed milk is given to the SAM child including the night shifts [18,29].
Risk factors associated with poor outcome of SAM inpatient management should be looked for constantly by the treating doctors, the nurses, the nutritionists, and the mothers of children to intervene early against these factors [30].
If the recent death rate of 5.4% and other short and long term complications and undesired outcomes of inpatient management of SAM in EL-Obied specialized pediatric hospital, in the center of therapeutic feeding more attention, should be paid to the diagnosis and treatment of the underlying medical conditions and to all factors that increase the mortality from severe malnutrition in children below five years, also thorough more care should be given to following the guidelines of the management protocol and re-evaluation then should be carried out to detect any improvements in the mortality from severe malnutrition and associated complications in this center [31-33].
Conclusion
From this study, we conclude the following that most of the admitted children with SAM were of the age group 6-24 months. Severe wasting was noticed in 87.5% of these children 24.7% showed edematous malnutrition which showed a significant relationship with the age of the child 68.2% showed signs of vitamin A deficiency. F75 was the initial feeding milk in all of the patients included significant relationship was found between taking the proper amount of F-75 and duration of stay.
12.5% of the patients escaped from stabilizing center, 5.4% died and the rest (82.1%) were transferred to Outpatient centers (OTP).
The protocol for admission criteria was found to be followed in this center to a good extent although areas for improvement of protocol implementation are also required.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
References
- Blossner, Monika, Mercedes De Onis, and Annette Prüss-Üstün. "Malnutrition: Quantifying the health impact at national and local levels." World Health Organization, 2005.
- Wagnew, Fasil, et al. "A meta-analysis of inpatient treatment outcomes of severe acute malnutrition and predictors of mortality among under-five children in Ethiopia." BMC Public Health, Vol. 19, No. 1, 2019, pp. 1-11.
- Rytter, Maren JH, et al. "Risk factors for death in children during inpatient treatment of severe acute malnutrition: A prospective cohort study." The American Journal of Clinical Nutrition, Vol. 105, No. 2, 2017, pp. 494-502.
- Coulter, J. B. S. "Nutrition and malnutrition in low-and middle-income countries." Paediatrics and International Child Health, Vol. 34, No. 4. 2014, pp. 233-35.
- Kanan, Shaza OH, and O. Elkhalifa Abd Elmoneim. "Prevalence and causes of undernutrition among under-five Sudanese children: A mini-review." Journal of Advances in Medicine and Medical Research, Vol. 32, No. 15, 2020, pp. 12-20.
- Jomah, J. A. S. "Determinants of child malnutrition in Sudan." International Journal of Multidisciplinary Approach and Studies, Vol. 5, No. 2, 2018, pp. 47-56.
- World Health Organization. "Nutrition Landscape Information System (NLIS) country profile indicators: Interpretation guide." 2019.
- Reinhardt, Kristina, and Jessica Fanzo. "Addressing chronic malnutrition through multi-sectoral, sustainable approaches: A review of the causes and consequences." Frontiers in Nutrition, Vol. 1, 2014, p. 13.
- Lopez, Alan D. "Levels and trends in child mortality: Report 2014, estimates developed by the UN inter-agency group for child mortality estimation." United Nations Inter-agency Group for Child Mortality Estimation (UN IGME), 2014.
- Sartorius, Benn KD, and Kurt Sartorius. "Global infant mortality trends and attributable determinants-An ecological study using data from 192 countries for the period 1990-2011." Population Health Metrics, Vol. 12, No. 1, 2014, pp. 1-15.
- Rice, Amy L., et al. "Malnutrition as an underlying cause of childhood deaths associated with infectious diseases in developing countries." Bulletin of the World Health Organization, Vol. 78, No. 10, 2000, pp. 1207-21.
- Duggan, Maureen B. "Prevention of childhood malnutrition: immensity of the challenge and variety of strategies." Paediatrics and International Child Health, Vol. 34, No. 4, 2014, pp. 271-78.
- Pridmore, Pat, and Roy Carr Hill. "Addressing the underlying and basic causes of child undernutrition in developing countries: What works and why?" Danida, 2009.
- Mehta, Nilesh M., et al. "Defining pediatric malnutrition: A paradigm shift toward etiology‐related definitions." Journal of Parenteral and Enteral Nutrition, Vol. 37, No. 4, 2013, pp. 460-81.
- Schaible, Ulrich E., and H. E. Stefan. "Malnutrition and infection: Complex mechanisms and global impacts." PLoS Medicine, Vol. 4, No. 5, 2007, p. e115.
- Karaolis, Nadina, et al. "WHO guidelines for severe malnutrition: Are they feasible in rural African hospitals?" Archives of Disease in Childhood, Vol. 92, No. 3, 2007, pp. 198-204.
- World Health Organization. "Guideline: Updates on the management of severe acute malnutrition in infants and children." World Health Organization, 2013.
- Houston, Kirsty A., Jack G. Gibb, and Kathryn Maitland. "Oral rehydration of malnourished children with diarrhoea and dehydration: A systematic review." Wellcome Open Research, Vol. 2, 2017, p. 66.
- Tickell, Kirkby D., and Donna M. Denno. "Inpatient management of children with severe acute malnutrition: A review of WHO guidelines." Bulletin of the World Health Organization, Vol. 94, No. 9, 2016, pp. 642-51.
- Ashworth, Ann, et al. "Guidelines for the inpatient treatment of severely malnourished children." World Health Organization, 2003.
- Scherbaum, Veronika, and M. Leila Srour. "The role of breastfeeding in the prevention of childhood malnutrition." Hidden Hunger, Vol. 115, 2016, pp. 82-97.
- World Health Organization. "Nutrition for health and development. Severe malnutrition: Report of a consultation to review current literature." 2010.
- World Health Organization. "Guideline: Updates on the management of severe acute malnutrition in infants and children." World Health Organization, 2013.
- Ministry of Health and Family Welfare Government of India. "Participant Manual for Facility Based Care of Severe Acute Malnutrition, 2013." Government of India Ministry of Health and Family Welfare Nirman Bhawan, New Delhi, India. https://www.nhm.gov.in/images/pdf/programmes/child-health/IEC-materials/PARTICIPANT-MANUAL_FBCSA-Malnutrition.pdf
- Zangenberg, Mike, et al. "Critical evaluation of the appetite test for children with severe acute malnutrition." Tropical Medicine and International Health, Vol. 25, No. 4, 2020, pp. 424-32.
- Bilal, Jalal A., et al. "Poor adherence to the World Health Organisation guidelines of management of severe acute malnutrition in children 6 to 59 months of age at Kalakla Turkish Hospital in Khartoum, Sudan." Sudanese Journal of Paediatrics, Vol. 18, No. 1, 2018, pp. 63-70.
- Shiferaw, Wegen, et al. "Treatment outcome and predictors of severe acute malnutrition using the WHO guideline at a referral Hospital in Southern Ethiopia." Ethiopian Journal of Pediatrics and Child Health, Vol. 11, No. 1, 2015, pp. 29-37.
- Prada, D. Ramírez, et al. "Using of WHO guidelines for the management of severe malnutrition to cases of marasmus and kwashiorkor in a Colombia children's hospital." Nutrition Hospital, Vol. 26, No. 5, 2011, pp. 977-83.
- Dale, Nancy M., et al. "Recovery and relapse from severe acute malnutrition after treatment: A prospective, observational cohort trial in Pakistan." Public Health Nutrition, Vol. 21, No. 12, 2018, pp. 2193-99.
- Rytter, Maren JH, et al. "Risk factors for death in children during inpatient treatment of severe acute malnutrition: A prospective cohort study." The American Journal of Clinical Nutrition, Vol. 105, No. 2, 2017, pp. 494-502.
- Saaka, Mahama, et al. "Treatment outcome of severe acute malnutrition cases at the tamale teaching hospital." Journal of Nutrition and Metabolism, Vol. 2015, 2015.
- Abate, Biruk Beletew, et al. "Treatment outcome of severe acute malnutrition and associated factors among under-five children in outpatient therapeutics unit in Gubalafto Wereda, North Wollo Zone, Ethiopia, 2019." PloS One, Vol. 15, No. 9, 2020, p. e0238231.
- Schwinger, Catherine, et al. "Severe acute malnutrition and mortality in children in the community: Comparison of indicators in a multi-country pooled analysis." PloS One, Vol. 14, No. 8, 2019, p. e0219745.