Research - International Journal of Medical Research & Health Sciences ( 2022) Volume 11, Issue 8
Evaluation of Medication Errors in Orthopaedic and Surgery Wards in a Tertiary Care Teaching Hospital
Bala Subramaniam1, Shah Megha H2*, Desai Chetna K2 and Desai Mira K32Department of Pharmacology, B.J. Medical College, Gujarat, India
33Department of Pharmacology, Nootan Medical College, Gujarat, India
Shah Megha H, Department of Pharmacology, B.J. Medical College, Gujarat, India, Email: mkshah_80@yahoo.com
Received: 17-Jul-2022, Manuscript No. ijmrhs-22-69397; Accepted Date: Sep 17, 2022 ; Editor assigned: 19-Jul-2022, Pre QC No. ijmrhs-22-69397 (PQ); Reviewed: 04-Aug-2022, QC No. ijmrhs-22-69397 (Q); Revised: 11-Aug-2022, Manuscript No. ijmrhs-22-69397 (R); Published: 30-Aug-2022
Abstract
Background: Medication errors can result in serious morbidity or mortality and have a significant economic impact on the patient and health care system Thus, this study aimed to determine the nature and type of Medication Errors (MEs), to find out the frequency and severity of medication errors, and assess the rationality of prescription orders in a tertiary care teaching hospital. Methods: A prospective, observational study was conducted in the Surgery and Orthopaedic ward of Civil Hospital, Ahmedabad from August 2018 to July 2019. MEs were categorized as prescription errors, dispensing errors, and administration errors. The case records and treatment charts were reviewed. The investigator also accompanied the staff nurse during the ward rounds and interviewed patients or caretakers to gather information, if necessary. The rationality of prescriptions was assessed using Phadke’s criteria. The MEs were categorized using the National Coordinating Council for Medication Error Reporting and Prevention (NCC MERP) category. Results: A total number of 170 (40.47%) medication errors were detected in 420 patients. Out of 170 errors, 89 (52.35%) were in surgery and 81 (47.64%) were in orthopaedic wards. Out of the 170 errors 166 (97.64%) were prescription errors, 3 (1.76%) were dispensing errors and 1 (0.58%) administration error. The majority of the prescriptions were semirational (65%) followed by rational (33%), while (2%) were rational. Conclusions: There is a need to establish an ME reporting system to reduce its incidence and improve patient care and safety
Keywords
Medication errors, Surgery, Orthopaedics, Phadke’s criteria, NCCMERP category
Introduction
An error can be encountered in our day-to-day life in every field of work. But medicine is such a field where we cannot afford to have any errors at all. The reason is simply that we deal with human lives and not merely machines. Medication Errors (MEs), are broadly defined as any error in the prescribing, dispensing, or administration of a drug to the patient. The majority of the developed countries have accepted ME monitoring and reporting as a part of health care and patient safety. While in India, the practice of ADR monitoring and pharmacovigilance is slowly gaining momentum, the concept of medication error is yet to be born. Medication errors also result in serious morbidity or mortality and have a significant economic impact on the patient and healthcare system [1]. MEs are more common in hospitalized patients due to multidrug therapy and severe or multiple diseases. In India, very few hospitals have undertaken ME assessments. Studies done in Karnataka and Uttarakhand has documented medication error rate to be as high as 40% and 25.7% respectively in hospitalized patients [2]. A study done in the Civil hospital of Gujarat has shown the error rate to be as high as 36% in indoor patients admitted to Medicine and Paediatric department [3]. Unfortunately, most medication errors remain undetected, if clinical significance or outcome does not adversely affect the patient.
Our hospital caters to patients from the states of Gujarat, parts of Rajasthan and Maharashtra. Surgery and Orthopaedic departments form a significant proportion of those availing the hospital services. Both departments deal with a large number of medicines and patients. There have been no studies so far in our hospital related to medication errors in these departments. Therefore, the present study was carried out to assess the determinants and extent of medication errors in the indoor patients of the surgery and orthopaedic department.
Methods
This study aimed to analyze the type and frequency of Medication Errors (MEs) in hospitalized patients at a tertiary care teaching hospital. Also, to evaluate factors affecting the rate and severity of MEs and assess the rationality of prescription orders.
Study site
General Surgery and Orthopaedic wards, civil hospital, Ahmedabad
Study type
An observational, prospective, longitudinal study
Study duration
12 months
Inclusion Criteria
Patients of all age groups and both genders were admitted to general surgery and orthopaedic wards and were included in the study after obtaining informed consent.
Exclusion Criteria
Patients who were transferred to other departments during the study period, patients from the out-patient department, and patients who were not willing to give informed consent were excluded from the study.
The study unit was selected by simple randomization by the chit method. Hence, patients admitted every Tuesday in the Surgery ward and every Thursday in the Orthopaedic ward were selected for the study. The investigator visited daily to the Surgery ward from August 2018 to January 2019 followed by the Surgery ward from February 2019 to July 2019. A validated pre-formed Case Record Form (CRF) was used to collect the data. The investigator went to surgery and orthopaedic wards and baseline data of the patient like demographic details, clinical examinations, diagnosis, laboratory investigations, and details of the drug treatment in the patient’s case report file and nursing chart were recorded in CRF and the patient was followed up till discharge. The investigator also accompanied the staff nurse during the ward rounds and interviewed patients or caretakers to gather information, if necessary. The rationality of prescriptions was assessed by Phadke’s criteria [4]. According to the criteria, each prescription was allotted 30 points and grouped into rational, semi-rational, or irrational prescriptions. NCCMERP category was used to categorize the medication errors [5].
Ethical consideration
The study protocol was approved by the Institutional Ethics Committee (IEC). All writing is done by the ethical principles of the declaration of Helsinki. Informed consent was taken from all the participants before enrolling in the study. Throughout the study, consent of all participants and data were gathered in complete confidence.
Results
A total number of 170 (40.47%) medication errors were detected in 420 patients. Out of 170 errors, 89 (52.35%) were in surgery and 81 (47.64%) were in orthopaedic wards. Out of the 170 errors 166 (97.64%) were prescription errors, 3 (1.76%) were dispensing errors and 1 (0.58%) administration error. A comparison of medication errors in both wards is described in Table 1. Among the 89 MEs in the surgery ward intestinal obstruction, 8 (8.89%) was the most common diagnosis involved followed by pancreatitis 6 (6.74%), and appendicitis 4 (4.49%). Of the 81 errors in the orthopaedic ward, open fractures involved 37 (45.67%), and closed fractures involved 22 (27.16%) of the diagnosis (Table 1).
| Parameters | Surgery ward (n=220) | Orthopaedic ward (n=200) |
|---|---|---|
| Number of Medication Errors (MEs) | 89 (52.35%) | 81 (47.64%) |
| Prescription errors | 87 (97.75%) | 79 (97.53%) |
| Dispensing errors | 1 (1.12%) | 2 (2.46%) |
| Administration errors | 1 (1.12%) | 0 |
| Common age group | 13 to 33 Years (39.33%) | 34 to 54 Years (32.09%) |
| Gender | Males (63, 70.78%) | Males (58, 71.60%) |
| Route of administration involved | Intravenous (83, 93.25%) | Intravenous (73, 90.12%) |
| Common drug groups involved in MEs | IV fluids (76, 85.395) | IV fluids (65, 80.24%) |
Demographic details
The majority of MEs were observed in males (63, 70.7%) in both the surgery and orthopaedic ward (58, 71.6%). The majority of them occurred in the age group of 13 years to 33 years (35, 39.3%) followed by 34 years to 54 years (24, 26.96%) and 54 years to 74 years (23, 25.84%) in the surgery ward. While in the orthopaedic ward 34 years to 54 years age group had the highest number of medication errors (26, 32.09%) followed by 13 years to 33 years (24, 29.62%) (Table 2). The majority of medication errors were observed with the intravenous route (83, 93.2%) followed by the oral route (6, 6.74%) in the surgery ward. Similarly in the orthopaedic ward, the highest medication errors were observed with the intravenous route (75, 92.59%) followed by the oral route (6, 9.9%) (Table 3). The most common drug group involved in MEs was IV fluids in the Surgery ward (76, 85.3%) and IV fluids in the orthopaedic ward (65, 80.2%) (Table 4). Among the 89 MEs in the surgery ward, the average total number of drugs prescribed was 6.85 whereas in the orthopaedic ward the average was 5.91.
| Surgery ward (n=89) | Orthopaedic ward (n=81) | ||
|---|---|---|---|
| Age group (years) | Medication Errors (%) | Age group (years) | Medication Errors (%) |
| 0 to 12 | 5 (5.61%) | 0 to 12 | 16 (19.71%) |
| 13 to 32 | 35 (39.33%) | 13 to 32 | 24 (29.60%) |
| 33 to 53 | 24 (26.91%) | 33 to 53 | 26 (32.09%) |
| 54 to 74 | 23 (25.82%) | 54 to 74 | 14 (17.22%) |
| >75 | 2 (2.21%) | >75 | 1 (1.23%) |
| Surgery ward (n=89) | Orthopaedic ward (n=81) | ||||
|---|---|---|---|---|---|
| Route of administration | Number of Medication Errors (%) | Route of administration | Number of Medication errors (%) | ||
| Intravenous | 83 (93.25%) | Intravenous | 75 (92.59%) | ||
| Oral | Tablet | 2 (2.24%) | Oral | Tablet | 4 (4.91%) |
| Syrup | 4 (4.49%) | Syrup | 2 (2.46%) | ||
| Drug group | Surgery ward (n=89) | Orthopaedic ward (n=81) |
|---|---|---|
| IV fluids | 76 (85.31%) | 65 (80.24%) |
| Antimicrobials | 5 (5.56%) | 7 (8.60%) |
| GI drugs | 4 (4.49%) | 2 (2.49%) |
| Others | 4 (4.49%) Iron, Furosemide, Pancreatin) | 2 (2.49%) (Metformin) |
| NSAIDs | 0 | 5 (6.10%) |
| Total | 89 | 81 |
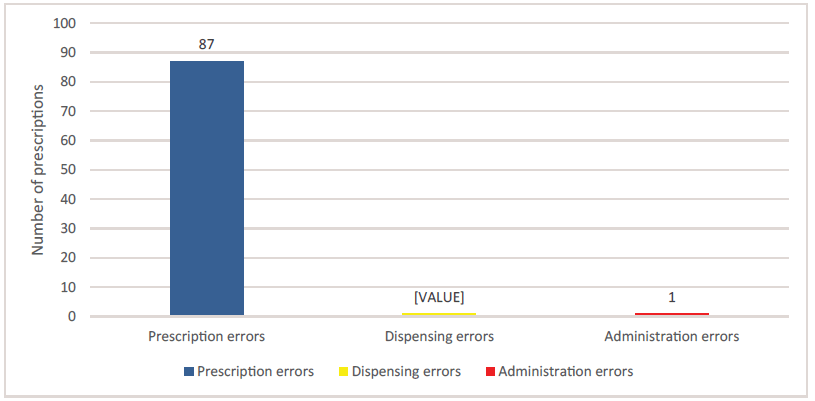
Medication errors in surgery indoor patients
Out of 220 patients enrolled during the study period, MEs were observed in 89 (40.45%) patients. Out of 89 MEs, 87 (97.7%) were in the prescription phase, 1 (1.12%) in dispensing phase, and 1 (1.12%) in the medicine administration phase (Figure 1).
Prescription errors
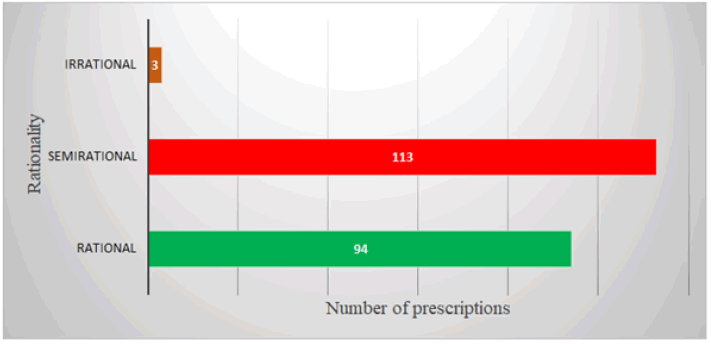
A total of 87 (93.10%) prescription errors were observed in the surgery ward. The majority of the prescription errors happened with IV fluids (80, 91.9%) where the rate of infusion was not mentioned and instead was prescribed as infuse slowly. Normal saline, ringer’s lactate, and dextrose normal saline were the IV fluids involved. The adult dose was prescribed for pediatric patients in 3 (3.4%) cases the adult dose of cefotaxime, cefosulbactam, and amoxicillinclavulanate was prescribed in pediatric cases and the dose of syrup formulation was not mentioned in 2 (2.2%) cases which involved lactulose and amoxicillin clavulanate syrups and dose prescribed as half tablets in 2 (2.2%) cases involving paracetamol and ethambutol tablets. All the errors fall under the type C category in the NCCMERP category, i.e, the error has reached the patient but has not caused any harm to the patient. The rationality of each prescription was assessed for choice of drug and selection dosage formulation, dose, frequency, and duration of treatment (Phadke’s criteria). Out of 220 prescriptions, 210 were assessed for rationality (diagnosis was not mentioned in 10 prescriptions and hence excluded). The majority of prescriptions (113, 54%) scored between 15-24 points and were categorized as semi-rational. While 3 prescriptions (1.4%) scored between 0-14 points, thus categorized as irrational where dosing of antibacterials and NSAIDs was inappropriate for the patient. However, 94 prescriptions (44.7%) scored between 25-30 points and thus were rational (Figure 2).
Dispensing errors
Out of 89 MEs in the surgery ward, one dispensing error was observed. Iron syrup (Haem up) was prescribed but the pharmacist dispensed cough syrup which the patient took for 2 days before it was noticed by the doctor and changed. However, it has not resulted in any harm to the patient and so it falls under type C category error under NCCMERP.
Medicine administration errors
Out of 89 MEs in the surgery ward, only one administration error was observed. Pantoprazole was prescribed by the doctor but the nurse had administered ranitidine and the same was written in the nurse’s order book. Though both the drugs are used to control gastric acid secretion they belong to different groups (PPI and H2 blocker) which differ in efficacy. Also, the surgeon was not aware of this. Again it has not resulted in any harm to the patient and falls under type C category error under NCCMERP.
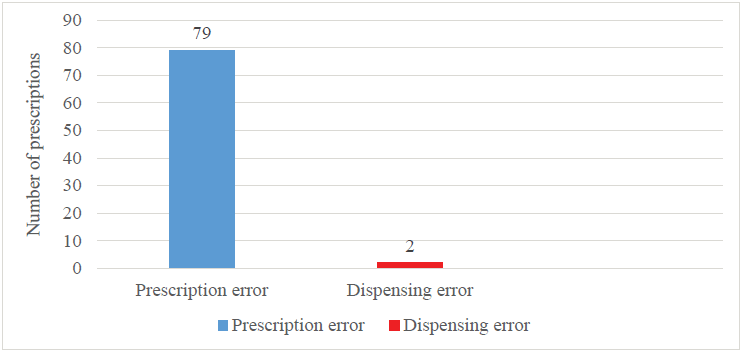
Medication errors in orthopaedic indoor patients
Out of 200 patients enrolled during the study period, medication errors were observed in 81 (40.5%) patients. Out of 84 MEs, 79 (97.5%) were prescription errors, and 2 (2.46%) dispensing errors (Figure 3)
Prescription error
Out of 81 medication errors, 79 (97.5%) were prescription errors. The rate of IV fluids administration was not mentioned in 65 (82.27) patients. The dose was not mentioned in 2 (2.5%) patients which involved amikacin and ranitidine which were prescribed as one ampule instead of mentioning the dosage. The adult dose was prescribed in 2 (2.5%) pediatric patients whereas cefosulbactam (1.5 gm) and (500 mg) were prescribed to an 11 years old and 3 years old patient. In 8 (10.10%) cases proper dosage was not mentioned instead half ampule/tablets were prescribed which included drugs like cefosulbactam, levofloxacin, amikacin, ranitidine, pantoprazole, and ondansetron. In 2 (2.5%) patients syrup dosage was not mentioned instead teaspoon was mentioned which involved ibuprofen and calcium syrups.
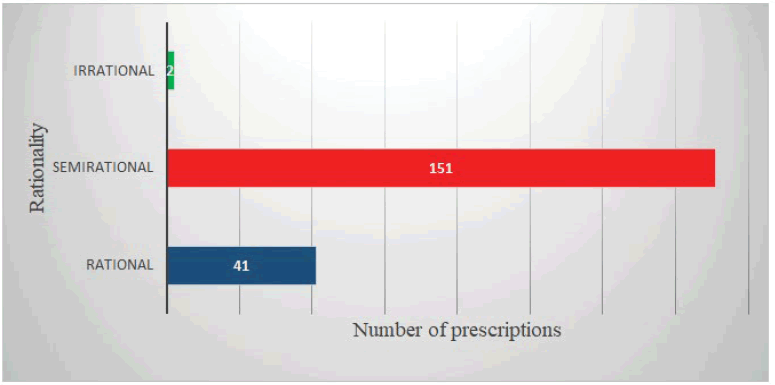
The rationality of each prescription was assessed for choice of drug and selection dosage formulation, dose, frequency, and duration of treatment (Phadke’s criteria). Out of 200 prescriptions, 194 were assessed for rationality (final diagnosis was not mentioned in 6 prescriptions and hence excluded). The majority of prescriptions (151, 77.8%) scored between 15-24 points and were categorized as semirational. While 2 prescriptions (1.03%) scored between 0-14 points, thus categorized as irrational which included wrong drug and wrong dose (antibacterial was prescribed in closed fracture and also wrong dose prescribed). However, 41 prescriptions (21.13%) scored between 25-30 points and thus were rational (Figure 4).
Dispensing errors
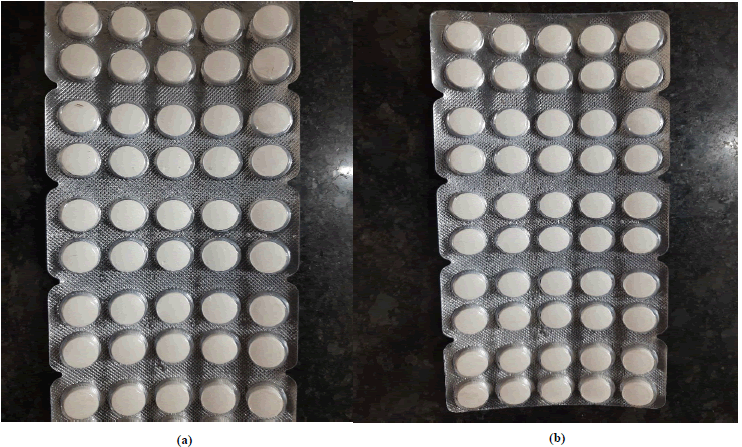
A total of 2 (2.46%) dispensing errors were observed. In both cases, Metformin was dispensed by the pharmacist instead of calcium tablets. Both these tablets were look-alike drugs and also of the same dose (500 mg) which was written on the strip which lead to the wrong dispensing by the pharmacist. The patient did take the wrong drug for 2 days before the physician noticed it and changed the drug. As there was no harm caused to the patient and this error falls under the type C category under the NCCMERP category.
Medicine administration error
There was no medication administration error in the orthopaedic ward during the study period.
Nearly everybody in the world takes medication at one time or another. Most of the time the medications are favourable or at least they root no harm but on occasion, they do harm the person taking them [6]. Sometimes these harms are due to errors occurred during the medication use process which can be prevented. In hospitals, errors can occur in every step of the medication use process starting from procuring the drug to prescribing, transcribing, dispensing, administering, and monitoring its effect [7]. Annually 7000 mortalities have been reported due to medication errors [8]. In India, medication errors and medication-related problems are mainly due to the irrational use of medications [9,10].
The present study was conducted at one of the largest hospitals in Gujarat, India. The study was intended to observe the determinants and occurrence of medication errors with their different types in these selected units. A total of 420 patients were enrolled in the study, of which 220 were in surgery and 200 were in the orthopaedic ward. Analysis was done separately for two groups. Our study observed higher medication errors (40.47%) as compared to 36% of MEs reported by Drupal et al in medicine and pediatric patients.
Our study observed 40.47% of ME which was comparable to a study done in Gujarat which reported (45.90%) of MEs [11]. This study also had a similar study population (427) as ours. While a study was done at Mangalore by Dilnasheen et al involving 200 patients who reported (20%) ME [12]. Our study showed that in the surgery ward, the 13 to 32 age group was more affected by medication errors (35, 39.32%) while a study done in Kuwait involving 203 patients reported 30 to 39 age group was commonly involved in medication errors (84, 41.4%) [13]. On the contrary, Sayali Pote et al reported that more than 60 years had a high number of MEs (69.1%) [14]. As per our observation, it can be stated that adolescents or adults are more prone to medication errors. This can be due to a high number of hospital admissions.
In the orthopaedic ward, the 34-54 age group were more affected by medication errors (26, 32%) which was comparable to a study done in the orthopaedic department in Karnataka that reported (54, 40%) error in this age group [15]. Furthermore, our study reported a high number of MEs in the 0 to 12 age group (16, 19.7%) which is higher than compared to this study (8, 6%). This difference may be attributed to improper calculation of dose as dosing was not done according to the weight of the patient in our study. In addition, the pharmacokinetics or pharmacodynamics of drugs also differ in children. This calls for a need to monitor MEs in pediatric age group patients and educate the stakeholders.
In our study males were more affected by MEs in both surgery and orthopaedic wards which is comparable to an Indian study conducted in Gujarat in medicine and pediatric wards. Similar observations have been reported in a study conducted in Delhi [16]. This could be because the study population consisted of more males than females.
In the present study intravenous route of administration was involved with MEs in surgery (93.2%) and orthopaedic (92.59%) wards which were similar to the study done by Sandip and another study by Nrupal. Our observations are supported by a study in Karnataka India having the same finding with an intravenous route (49.5%) in medicine and surgery departments. Additionally, a study done by Ross and colleagues in the pediatric department also revealed that the intravenous route of medication administration is commonly involved (109, 56%) in medication errors [17].
Majed I Al-Jeraisy also reported that half of the MEs were detected by intravenous route (50.2%) followed by the oral route of administration which is similar to the present study [18]. This suggests that medication errors are commonly associated with the intravenous route. This can be because patients are hospitalized and may require urgent drug treatment for rapid recovery. Secondly, the use of intravenous fluids (IV) and an intact i.v. the line for intravenous medications is also high in hospitalized patients.
The most common drug group involved in MEs in the surgery ward was IV fluids (85.3%) followed by antibacterial (5.6%) and gastrointestinal drugs (4.49%). This could be because a significant number of patients were hospitalized for undergoing various surgeries. While GI drugs like ranitidine and ondansetron have been prescribed inappropriately, anticipating gastritis and vomiting in these patients. This was comparable to a study done in Sydney, Australia which reported (that 69.7%) of MEs were due to IV fluids.
Our study also showed that MEs were common with IV fluids (80.24) in orthopaedic patients followed by antibacterial (8.6%) drugs and NSAIDs (28.5%). This could be because a significant number of patients were hospitalized for undergoing various traumatic surgeries. Overall it increases the use of IV fluids and antibacterials. A study done in Karnataka showed NSAIDs (31.6%) were the most commonly encountered drug group followed by gastrointestinal (31.6%) and antibacterials (30.9%). The differences can be attributed to more number of patients with trauma (requiring IV fluids and antimicrobials) being admitted to our study.
Prescription errors were most common in surgery and orthopaedic wards due to the inappropriate prescription of medicines. This was comparable to a study done in Karnataka in the medicine and orthopaedic ward by Surendra Shrestha et al reporting (62%) prescription errors. A total of 87 (97.7%) prescription errors were observed in the surgery ward in our study. It included IV fluids, antibacterials, pantoprazole, ondansetron, etc in a variety of clinical conditions. The majority of the prescription errors happened with IV fluids (83, 93.2%) where the rate of infusion was not mentioned and instead was prescribed as infuse slowly. Normal saline, ringer’s lactate, and dextrose normal saline were the IV fluids involved. The adult dose was prescribed for pediatric patients in 3 (3.44%) cases. The adult dose of cefotaxime, cefosulbactam, and amoxicillin-clavulanate was prescribed in pediatric cases and the dose of syrup formulation was not mentioned in 2 (2.29%) cases that involved lactulose and amoxicillin clavulanate syrups and dose prescribed as half tablets in 2 (2.29%) cases involving paracetamol and ethambutol tablets.
In the orthopaedic ward, IV fluids were the most commonly involved drug group in MEs followed by antibacterials. In cases of closed fractures that are not operated antibacterials are usually not needed [19]. The dose was not mentioned in 2 (2.5%) patients which involved amikacin and ranitidine which were prescribed as one ampule. Furthermore, an adult dose was prescribed in 2 (2.5%) pediatric age groups where cefosulbactam (1.5 gm) and (500 mg) were prescribed to an 11-year-old and 3-year-old patient. In 6 (7.5%) cases proper dosage was not mentioned instead half ampule/tablets were prescribed which included drugs like cefosulbactam, levofloxacin, amikacin, ranitidine, pantoprazole, and ondansetron. In 2 (2.5%) patients syrup dosage was not mentioned instead teaspoon was mentioned which involved ibuprofen and calcium syrups.
Dispensing errors were detected in both wards. Dispensing errors are difficult to compare with available literature due to different clinical settings. A wrong drug was dispensed in the surgery ward which lead to dispensing error (1.12%). This was similar to a study done in Punjab which showed (that 1.72%) of MEs were due to dispensing of the wrong drug [20]. The drug was purchased from a private pharmacy as the prescribed drug was not available in the hospital pharmacy which could be the reason for this error.
In orthopaedic ward 2 (2.46%) dispensing errors were observed. A study done in Karnataka in the orthopaedic ward reported (4%) dispensing errors. In our study metformin was dispensed by the pharmacist instead of calcium tablets leading to dispensing error. Both these tablets were look-alike drugs and also of the same dose (500 mg) which was written on the strip which lead to the wrong dispensing by the pharmacist (Figure 5). However, it resulted in no harm to the patient. A similar incident was reported by a study conducted in Vadodara where potassium chloride was given to the patient instead of sodium bicarbonate due to looking alike ampoules of the drug [21].
Our study showed (1.12%) medication administration errors in the surgery ward. This was comparable to a study done in Telengana in various departments that reported (a 2.72%) administration error [22]. Pantoprazole was prescribed by the doctor but the nurse had administered ranitidine and the same was written in the nurse’s order book.
We had undertaken a prospective study over 12 months wherein details of the occurrence of medication errors were recorded precisely. The strength of our study includes systematically exposing the extent and type of ME using chart review and direct observation, and the reasonably appropriate and sensitive methods to detect medication errors in a hospital setting. Moreover, we also had the study population i.e. number of patients admitted to the wards as the denominator during the study period. Thus we were able to evaluate ME in each phase of the medication use cycle. In addition, we also assessed prescription orders for rationality and the NCCMERP category of errors.
However, this prospective study has its limitations such as smaller sample size and only one unit from each ward (surgery and orthopaedic) was selected. The investigator could not be present all the time during medication administration to check for administration errors. Drug-drug interactions were not evaluated. Also while assessing the rationality, the clinicians’ viewpoint was not taken into account, which could have been different from ours.
Despite these limitations, our study leads to several important conclusions. MEs were frequently occurring at a rate of 40.47% in hospital settings. Prescribing errors were more common followed by dispensing errors and medication administration errors. MEs were common in patients between 0 years-12 years and males taking more than five medicines per prescription and intravenous route of administration. The most common drug group involved in MEs was IV fluids in the surgery and orthopaedic ward. The findings of this study were discussed with prescribers and nursing staff. They have advised about the storage of look-a-like medications in different places and the proper labelling of these medicines. Also, awareness and education program was undertaken to decrease MEs.
Conclusion
The rate of prescribing errors was higher than administration errors. The study also showed the occurrence of MÉ’s with iv fluids and all the MEs were of NCCMERP category C and the majority of prescriptions were semirational in surgery and orthopaedic wards.
Periodic awareness and education programs for prescribers and nursing staff should be undertaken. In addition, the adoption of clinical pharmacists/pharmacologists on ward rounds could also lower the ME rate. Regular monitoring of MEs, DDIs, and rationality should be undertaken in hospital settings. All such strategies to reduce MEs will ensure the successful delivery of the health care system to the patients and ensure patient safety.
Declarations
Acknowledgement
The writers of this publication would like to thank the study participants.
Conflict of Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Sources of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors
Abbreviations
ME- Medication errors
NCCMERP- National Coordinating Council for Medication Error and Prevention
IV fluids- Intravenous fluids
GI drugs- Gastrointestinal drugs
NSAIDs – Non-Steroidal Anti-Inflammatory drugs
References
- Williams, David JP. "Medication errors." Journal-Royal College of Physicians of Edinburgh, Vol. 37, No. 4, 2007, p. 343.
Google Scholar - Shrestha, Surendra, and K. Ramanath. "Study and evaluation of medication errors in medicine and orthopaedic wards of a tertiary care hospital." British Journal of Pharmaceutical Research, Vol. 7, 2015, pp. 183-95.
Google Scholar Crossref - Patel, Nrupal, et al. "A study of medication errors in a tertiary care hospital." Perspectives in clinical research, Vol. 7, No. 4, 2016, p. 168.
Google Scholar Crossref - Phadke, Anant. "Drug supply and use: Towards a rational policy in India." SAGE Publications Pvt. Limited, 1998.
Google Scholar - Al Mardawi, Ghada Hussain, and Rajkumar Rajendram. "Investigation of Medication Safety Incidents Using Root Cause Analysis and Action." Global Journal on Quality and Safety in Healthcare, Vol. 4, No. 1, 2021, pp. 50-52.
Google Scholar - Sreekumar, Sreevidya S., et al. "Role of pharmacy students in reducing medication error-a survey." International Journal of Research in Hospital and Clinical Pharmacy, Vol. 1, No. 4, 2019, pp. 94-96.
Google Scholar Crossref - Aspden, Philip, and Philip Aspden. "Preventing medication errors." National Academies Press, 2007.
Google Scholar - Hinojosa‐Amaya, José M., et al. "Medication errors: Electronic vs. paper‐based prescribing. Experience at a tertiary care university hospital." Journal of evaluation in clinical practice, Vol. 22, No. 5, 2016, pp. 751-54.
Google Scholar Crossref - Rajanandh, M. G., R. U. B. Y. Varghese, and C. Ramasamy. "Assessment of drug information services in a South Indian tertiary care hospital in Kanchipuram district." International Journal of Pharmacy and Pharmaceutical Sciences, Vol. 3, No. 3, 2011, pp. 273-76.
Google Scholar - Krishna, Jai, et al. "A preliminary study on profile and pattern of medication errors from a tertiary care teaching hospital." International Archives of Integrated Medicine, Vol. 2, No. 7, 2015, pp. 93-98.
Google Scholar - Patel, Sandip, et al. "Study of medication error in hospitalised patients in tertiary care hospital." Indian Journal of Pharmacy Practice, Vol. 11, No. 1, 2018.
Google Scholar Crossref - Sheikh, Dilnasheen, et al. "Assessment of medication errors and adherence to WHO prescription writing guidelines in a tertiary care hospital." Future Journal of Pharmaceutical Sciences, Vol. 3, No. 1, 2017, pp. 60-64.
Google Scholar Crossref - Ahmed, Zamzam, et al. "Medical errors: Healthcare professionals’ perspective at a tertiary hospital in Kuwait." PloS one, Vol. 14, No. 5, 2019, p. e0217023.
Google Scholar Crossref - Pote, Sayali, Pramil Tiwari, and Sanjay D'cruz. "Medication prescribing errors in a public teaching hospital in India: A prospective study." Pharmacy Practice, Vol. 5, No. 1, 2007, pp. 17-20.
Google Scholar Crossref - Shrestha, Surendra, and K. Ramanath. "Study and evaluation of medication errors in medicine and orthopaedic wards of a tertiary care hospital." British Journal of Pharmaceutical Research, Vol. 7, 2015, pp. 183-95.
Google Scholar Crossref - Agrawal, Pankaj, et al. "Statistical analysis of medication errors in Delhi, India." Indo Global Journal of Pharmaceutical Sciences, Vol. 2, No. 1, 2012, pp. 88-97.
Google Scholar - Ross, L. M., J. Wallace, and J. Y. Paton. "Medication errors in a paediatric teaching hospital in the UK: five years operational experience." Archives of disease in childhood, Vol. 83, No. 6, 2000, pp. 492-97.
Google Scholar Crossref - Al-Jeraisy, Majed I., Menyfah Q. Alanazi, and Mostafa A. Abolfotouh. "Medication prescribing errors in a pediatric inpatient tertiary care setting in Saudi Arabia." BioMed Central research notes, Vol. 4, No. 1, 2011, pp. 1-6.
Google Scholar Crossref - Frederick Azar M. et al.,"Campbell’s operative orthopaedics," 14th ed, Elsevier, Vol 2, 2020 pp. 464. 24.
- Amit, Sharma, and Arora Sandeep. "A Review on Medication Errors." Journal of pharmaceutical technology, research and management, Vol. 3, No. 2, 2015, pp. 89-96.
Google Scholar - Shah, Hetal D., and Megha Shah. "A case of look-alike medication errors." Indian Journal of Pharmacology, Vol. 43, No. 4, 2011, p. 482.
Google Scholar Crossref - Pramod Kumar, D. et al. "Assessment of medication errors in tertiary care hospital." International Journal of Pharmaceutics, Vol. 1, No. 3, 2020, pp. 1-8.