Research - International Journal of Medical Research & Health Sciences ( 2022) Volume 11, Issue 8
Enhanced Recovery After Surgery(ERAS) Protocols vs Standard Care in Patients with Peptic Ulcer Perforation
Anandaravi BN, Manjunath RD and Vidhya Shree N*Vidhya Shree N, Department of General Surgery, Mysore Medical College and Research Institute, Karnataka, India, Email: nvid9080@gmail.com
Received: 22-Jul-2022, Manuscript No. ijmrhs-22-67309; Accepted Date: Aug 22, 2022 ; Editor assigned: 25-Jul-2022, Pre QC No. ijmrhs-22-67309 (PQ); Reviewed: 26-Jul-2022, QC No. ijmrhs-22-67309 (Q); Revised: 27-Jul-2022, Manuscript No. ijmrhs-22-67309 (R); Published: 30-Aug-2022, DOI: J-67309
Abstract
Background: To compare the efficacy of Enhanced Recovery After Surgery (ERAS) protocol vs standard care in patients with Perforated Peptic Ulcer (PPU). Materials: This single-center, retrospective, cross-sectional study was carried out from January 2021 to January 2022. Patients with PPU undergoing Graham’s repair were divided into standard care and ERAS groups. The primary outcome was the duration of stay. Secondary outcomes were functional recovery parameters and morbidity. Results: A total of 120 cases of PPU were admitted to our hospital, among which 60 patients each were included in the standard care and ERAS groups, respectively. Patients in ERAS group had a significantly early functional recovery for the time to first flatus (1.41 vs 2.38; p<0.001), first stool (2.65 vs 3.78; p<0.001), first fluid diet (2.75 vs 6.1; p<0.001), and solid diet (4.08 vs 7.11; p<0.001). Duration of stay in the ERAS group was significantly shorter (6.2 vs 8.53; p<0.001). There was a significant reduction in postoperative morbidities such as postoperative nausea and vomiting (RR 0.43, p-value=0.005), superficial SSI (RR 0.4, p=0.005), and pulmonary complications (RR 0.45, p=0.002). ERAS group showed better primary and secondary outcomes. Conclusions: In conclusion, ERAS protocols, are feasible and safe for application in selected patients undergoing Graham’s repair of perforated peptic ulcer without an increase in the rate of complications.
Keywords
Peptic ulcer, Perforation, Duration of stay, Enhanced Recovery After Surgery, ERAS
Introduction
In the late 1900s, Professor Henrik Kehlet and other pioneers put forward a concept of multimodal surgical care to attenuate physiological and psychological stress, thus accelerating patients’ recovery [1].
The key principles of the ERAS protocol include pre-operative counseling, preoperative nutrition, avoidance of perioperative fasting and carbohydrate loading up to 2 hours preoperatively, and standardized anesthetic and analgesic regimens (epidural and non-opioid analgesia) and early mobilization [2]. However, despite its success in the elective setting, perioperative care in the emergency setting continues to utilize the traditional principles [3].
Perforated Peptic Ulcer (PPU) is a serious complication of PUD and patients with PPU often present with an acute abdomen that carries a high risk for morbidity and mortality. The lifetime prevalence of perforation in patients with PUD is about 5%. PPU carries mortality ranging from 1.3% to 20% [4].
The application of the evidence-based ERAS protocols has the potential to improvising the outcomes in the perioperative period. Hence, this study was carried out to evaluate the safety, efficacy, and feasibility of ERAS protocol in patients who underwent simple closure of perforated duodenal ulcers.
Methods
This study was a single-center, retrospective cohort study carried out in the Department of Surgery of K.R hospital from January 2021 to January 2022. A total of 123 cases of gastro-duodenal perforation were admitted to our hospital, among which 60 patients each were included in the standard care and ERAS groups, respectively. Three malignant perforation cases were excluded as their management was changed based on intra-operative findings. Written informed consent was taken from all the participants. Ethical approval was taken from the Institutional Ethical committee.
Sample size calculation
• Confidence interval 95
• The margin of error 5
• Population size 180
• Z score 1.96
• Sample size 123
Inclusion criteria
All patients of age 18 years and above with perforated duodenal ulcer.
Exclusion criteria
Age <18 years, ASA (American Society of Anesthesiologists) class 3 or 4, coexistent psychiatric or neurological illness, patients with refractory septic shock at presentation, and patients with a history of chronic steroid use.
Preoperative preparation was identical in both the groups in the placement of Nasogastric (NG) tube at admission and administration of crystalloids, Intravenous (IV) Antibiotics, and IV pantoprazole. All patients underwent closure of the peptic ulcer perforation by the Grahams patch technique under general anesthesia with the standard anesthetic protocols. Two 28-F abdominal drains were placed in the Morrison pouch and pelvis before the closure of the abdomen.
ERAS protocol was based on non-opioid analgesia, early nutrition, and early mobilization of the patients. All patients were discharged with H. pylori kit and were advised to continue oral Rabeprazole (20 mg Q12H) for 3 months. All patients were reviewed on postoperative days 10 and 30 for the presence of any complications or need for readmissions (Table 1).
| Differences between the two groups in the care pathways | ERAS protocols | Standard care |
|---|---|---|
| Pre-operative resuscitation | Intravenous crystalloids, NG tube, Intravenous antibiotics, antacids | Intravenous crystalloids, NG tube, Intravenous antibiotics, antacids |
| Analgesics | Epidural bupivacaine infusion for 24 hrs postoperatively | Opioid analgesia |
| POD0-IV Acetaminophen 1g iv tid POD1-IV Acetaminophen 1g iv tid POD2-oral acetaminophen 500 mg tds (iv dose if NPO) | POD0-IV tramadol 100mg bid POD1-IV tramadol 100mg bid POD2 onwards-IV tramadol and acetaminophen | |
| POD3-oral acetaminophen sos, Breakthrough pain-opioids sos | oral doses once feed resumed Breakthrough pain-opioids sos | |
| Intraoperative care | Grahams Patch Repair under general anesthesia | Grahams Patch Repair under general anesthesia |
| Antibiotics | IV ceftriaxone 1g bid and IV metronidazole 500mg tid×5 days | IV ceftriaxone 1g bid and IV metronidazole 500 mg tid×5 days 2 |
| Mobilization | Ambulate from POD0 (If an epidural catheter is inserted; sitting for 2 h on the day of surgery and ambulating after removal of the epidural catheter 24 h postoperatively) | Ambulate from POD 1 |
| Ambulate from POD0. (If an epidural catheter is inserted; sitting for 2 h on the day of surgery and ambulating after removal of the epidural catheter 24 h postoperatively) | ||
| Withdrawal of tubes and drains | Urinary catheter-when urine output is adequate over the last 24 h (0.5 ml/kg/hr in absence of inotropes/diuretics) | Urinary catheter-when output is adequate for 24 hrs |
| Drains-when the drainage is ≤ 100 ml/day irrespective of resumption of oral feeds | Drains-when unrestricted liquid diet tolerated×24 hrs | |
| NG tube-when the drainage is ≤ 300 ml/day irrespective of the presence or absence of bowel sounds | NG tube-when the drainage is ≤ 50 ml/day with signs of resolution of the ileus | |
| Resumption of oral feeds | NPO till the resolution of ileus | NPO till 5 days |
| Liquid diet after the appearance of bowel sounds | Clear liquids on day 5 and all liquids next 24 hrs | |
| Soft diet as tolerated within the next 24 hrs | Soft diet as tolerated within the next 24 hrs |
Outcome measures
The primary endpoint was the Duration of Stay (DOS) between the two groups. The secondary endpoints included time for removal of a nasogastric tube, drains, and catheter; duration of ileus; time for the first passage of flatus and stool; and time to first walk.
Data Collection and Statistical Analysis Data were collected on a specified proforma prepared by the investigators. Categorical variables such as gender, need for reinsertion of NG tube/extra analgesia, and complications were expressed as proportions. Continuous variables were analyzed using the independent Student t-test or Mann-Whitney U test. Categorical variables were analyzed using the chi-square test or Fisher’s exact test.
Results
Patients from January 2021 through January 2022, of the 120 patients with perforated peptic ulcers who were assessed for eligibility, 60 were in the standard perioperative care group, and 60 were in the ERAS group (Table 2).
| Age (Years) | ERAS | Standard | ||
|---|---|---|---|---|
| No. of patients | Percentage | No. of patients | Percentage | |
| Up to 25 | 10 | 16.70% | 7 | 11.70% |
| 25-35 | 7 | 11.70% | 9 | 15% |
| 35-45 | 12 | 20% | 16 | 26.70% |
| 45-55 | 16 | 26.70% | 11 | 18.30% |
| 55-65 | 9 | 15% | 13 | 21.70% |
| 65-75 | 6 | 10% | 4 | 6.70% |
| Total | 60 | 100% | 60 | 100% |
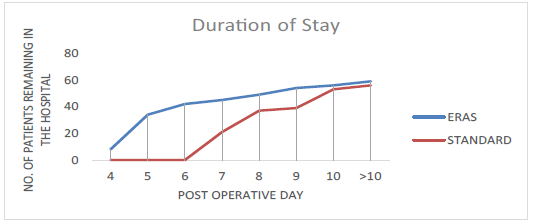
The length of hospital stay was reduced by 2.43 days in the adapted ERAS group when compared with the standard care group (p<0.0001, CI 5.66 to 9.09) (Table 3).
| Sex | ERAS | Standard | ||
|---|---|---|---|---|
| No. of patients | Percentage | No. of patients | Percentage | |
| Male | 50 | 83.3% | 56 | 93.3% |
| Female | 10 | 16.7% | 4 | 6.7% |
| Total | 60 | 100% | 60 | 100% |
60% of patients in the standard care group and 23% of patients in the adapted ERAS group stayed for more than 7 days (Figure 1).
Patients in the ERAS group had a significantly early return of bowel functions in terms of the appearance of first bowel sounds, first flatus, and first stools, and an earlier resumption of oral feeds (Table 4). Twenty patients developed postoperative ileus, eight in the adapted ERAS group and seventeen in the standard care group, who were managed conservatively with nasogastric tube reinsertion, bowel rest, and hydration.
| Outcome variable | ERAS group (n=60) | Standard group (n=60) | Mean difference | p-value | CI |
|---|---|---|---|---|---|
| Mean length of hospitalization (in days) | 6.2 | 8.53 | 2.43 | <0.001 | 5.66-9.09 |
| Mean day of withdrawal of nasogastric tube (days) | 2 | 5 | 3 | <0.001 | 2.0-5.0 |
| Mean time to first flatus (in days) | 1.41 | 2.38 | 0.966 | <0.001 | 1.22-2.51 |
| Mean time to first stool (in days) | 2.65 | 3.78 | 1.13 | <0.001 | 2.37-4.03 |
| Mean time to first fluid diet (in days) | 2.75 | 6.1 | 3.35 | <0.001 | 2.45-6.47 |
| Mean time to first solid diet (in days) | 4.08 | 7.11 | 3.03 | <0.001 | 3.63-7.50 |
| Mean time of removal of urinary catheter (days) | 1.4 | 2.83 | 1.43 | <0.001 | 1.18-3.09 |
The difference in the need for nasogastric tube reinsertion between the two groups however was not significant (8/60 vs. 17/60; p=0.23). The patients in the adapted ERAS groups had the drains and the urinary catheter removed significantly early when compared to the standard care group (Table 4).
Morbidity parameters
There was a significant reduction in the various postoperative morbidity parameters in the ERAS group when compared with the standard care group (Table 5). There was a significant reduction in postoperative morbidities such as superficial surgical site infections (RR 0.35, p=0.02), incidence of PONV (RR 0.28, p<0.0001), and pulmonary complications (RR 0.24, p=0.04) in the ERAS group.
| ERAS group (n=60) | Standard group (n=60) | Relative Risk | p-value | |
|---|---|---|---|---|
| *PONV | 12(20%) | 23(38.3%) | 0.43 | 0.005 |
| *SSI | 15(25%) | 25(41.7%) | 0.6 | 0.05 |
| Pulmonary complications | 14(23.3%) | 31(51.7%) | 0.45 | 0.0027 |
| Urinary tract infections | 12(20%) | 27(45%) | 0.44 | 0.006 |
| Mortality | 1(1.7%) | 4(6.7%) | 0.25 | 0.2088 |
| *PONV Postoperative Nausea And Vomiting, *SSI Surgical Site Infection | ||||
Discussion
In this retrospective trial, there was a significant reduction in hospital stay with no worsening of the postoperative complication rates in patients managed with ERAS protocols when compared to the standard care. Though there are few reports of successful use of modified ERAS protocols in an emergency, these studies were, however, limited by the inclusion of few care elements and fewer patients [5-7].
Gonenc et al. were the first to evaluate the feasibility of ERAS protocols in a prospective RCT on 47 patients who underwent laparoscopic Grahams patch repair [8].
In the present study, the attempt was made to use the maximum possible care elements of preoperative, intraoperative, and postoperative components in patients managed for PPU. In an emergency setting, the limited literature available demonstrates a decreased LOH by utilization of ERAS protocols.
In the present study, the hospital stay was reduced by 2.43 days in the ERAS group in patients managed by open Grahams patch repair.
Failure of adherence or implementation of intraoperative elements might lead to poor outcomes even though a strict protocol is followed during the postoperative period. ERAS protocols for major elective upper gastrointestinal surgery support the safe omission of routine nasogastric decompression [9-14].
Gonenc et al. in their study removed the nasogastric tube immediately after the patient's recovery from anesthesia [5]. In the present study, a significantly shorter duration of ileus and decreased incidence of pulmonary complications in the adapted ERAS group which had a truncated period (mean of 2 days) of NG decompression was found when compared to the standard care.
Gonenc et al. reported a mean of 1.5 days for resumption of orals in the ERAS group [5]. In the present study, liquid and solid feeds were resumed at an average of 2.7 and 4.08 postoperative days, respectively. Likewise, an average of 3.4 days was reported in patients who had urgent colectomy managed with ERAS protocol [6]. In the present study, limited use of drains was preferred as the evidence for the omission of drains in emergent situations is lacking. Moreover, with an adapted protocol, it was possible to attain a shorter time to first flatus, first feeds, and the first walk, thus accelerating patients’ recovery as in the previous reports.
Wisely et al. in their study reported a reduction of 20% in the number of patients with emergency laparotomy requiring catheters beyond 2 days owing to the “diffusion” of ERAS practices from elective procedures [15]. In the present study, the majority of the patients of the adapted ERAS group had the urinary catheter removed within 24 h and none had the catheter for more than 2 days.
Fast-track pathways utilize balanced or multimodal analgesia by combining various analgesics with regional blockade techniques [3,16,17]. Regional blockade in the form of a thoracic epidural catheter is an established component of ERAS protocols as it is associated with shortened ileus owing to the opioid-sparing effect [18].
Gonenc, et al. in their study resorted to NSAIDs for the management of postoperative pain with opioids for breakthrough pain [5]. The need for extra analgesia was not significant in the patients managed with ERAS protocols. However, it was significantly higher in the standard care group when compared with the adapted ERAS group.
The subgroup analysis within the ERAS group, surprisingly, demonstrated the role of epidural analgesia, in hastening bowel functions and shortening the hospital stay in the setting of ERAS in contrast to the reports refuting the same [19].
Wisely et al. in their study comparing all emergency laparotomies in the pre-ERAS and post-ERAS period reported a significant reduction in the complications in the post-ERAS period suggesting its safe role in an emergency. Lohsiriwat reported a non-significant reduction in the overall complication rates in patients of urgent colectomy managed with ERAS protocol when compared with conventional care [7].
In the present study, there was a significant reduction in the rates of superficial SSI, pulmonary complications, UTI, and incidence of PONV in the ERAS group. There was no readmission in the present study. Patients who developed minor complications before discharge continued to stay in the hospital; however, none of the patients who were discharged early in the adapted ERAS group had readmissions within 30 days of discharge.
Conclusion
The patients in the ERAS group had a significantly earlier functional recovery in terms of bowel functions, earlier resumption of oral feeds, and earlier mobilization. Hence, it demonstrates the safety, efficacy, and feasibility of an adapted ERAS protocol in emergent situations. In conclusion, ERAS pathways, in a modified form, are feasible and safe for application in selected patients undergoing Graham’s repair of perforated peptic ulcer without an increase in the rate of complications.
Declarations
Acknowledgments
The authors acknowledge the support of the Department of general surgery, Mysore medical college and research institute, Mysuru towards the conduct of the study.
Authors’ Contributions
All the authors were involved in the acquisition and analysis of the data. Dr. Anandaravi B.N. and Dr. Manjunath R.D. contributed to the conception of the work and revised the manuscript critically for intellectual content. Dr. Vidhya Shree N was the principal investigator and contributed to the acquisition, analysis of data, and preparation of the manuscript.
Funding
None
Conflict of Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Kehlet, Henrik, and Douglas W. Wilmore. "Evidence-based surgical care and the evolution of fast-track surgery." Annals of Surgery, Vol. 248, No. 2, 2008, pp. 189-98.
Google Scholar Crossref - Weimann, A., et al. "ESPEN guidelines on enteral nutrition: surgery including organ transplantation." Clinical Nutrition, Vol. 25, No. 2, 2006, pp. 224-44.
Google Scholar Crossref - Sanchez-Jimenez, R., et al. "ERAS (Enhanced Recovery after Surgery) in colorectal surgery." Colorectal Cancer-Surgery, Diagnostics and Treatment. 2014, pp. 487-03.
Google Scholar - Chung, Kin T., and Vishalkumar G. Shelat. "Perforated peptic ulcer-an update." World Journal of Gastrointestinal Surgery, Vol. 9, No. 1, 2017, pp. 1-12.
Google Scholar Crossref - Gonenc, Murat, et al. "Enhanced postoperative recovery pathways in emergency surgery: a randomized controlled clinical trial." The American Journal of Surgery, Vol. 207, No. 6, 2014, pp. 807-14.
Google Scholar Crossref - Roulin, Didier, et al. "Enhanced recovery pathway for urgent colectomy." World Journal of Surgery, Vol. 38, No. 8, 2014, pp. 2153-59.
Google Scholar Crossref - Lohsiriwat, Varut. "Enhanced recovery after surgery vs conventional care in emergency colorectal surgery." World Journal of Gastroenterology, Vol. 20, No. 38, 2014, p. 13950.
Google Scholar Crossref - Graham, Roscoe R. "The treatment of perforated duodenal ulcers." Surgery, Gynecology and Obstetrics, Vol. 64, 1937, pp. 235-38.
Google Scholar - Clavien, Pierre A., et al. "The Clavien-Dindo classification of surgical complications: five-year experience." Annals of Surgery, Vol. 250, No. 2, 2009, pp. 187-96.
Google Scholar Crossref - Nelson, Richard, Shamecka Edwards, and Bonnie Tse. "Prophylactic nasogastric decompression after abdominal surgery." Cochrane Database of Systematic Reviews, Vol. 3, 2004.
Google Scholar Crossref - Gustafsson, U. O., et al. "Guidelines for perioperative care in elective colonic surgery: Enhanced Recovery After Surgery (ERAS®) Society recommendations." Clinical Nutrition, Vol. 31, No. 6, 2012, pp. 783-800.
Google Scholar Crossref - Mortensen, K., et al. "Consensus guidelines for enhanced recovery after gastrectomy." Journal of British Surgery, Vol. 101, No. 10, 2014, pp.1209-29.
Google Scholar Crossref - Cheatham, Michael L., et al. "A meta-analysis of selective versus routine nasogastric decompression after elective laparotomy." Annals of Surgery, Vol. 221, No. 5, 1995, p. 469.
Google Scholar Crossref - Rao, Wensheng, et al. "The role of nasogastric tube in decompression after elective colon and rectum surgery: a meta-analysis." International Journal of Colorectal Disease, Vol. 26, No. 4, 2011, pp. 423-29.
Google Scholar Crossref - Wisely, Jessica C., and Karen L. Barclay. "Effects of an enhanced recovery after surgery programme on emergency surgical patients." ANZ Journal of Surgery, Vol. 86, No.11, 2016, pp.883-88.
Google Scholar Crossref - Kehlet, Henrik, and Douglas W. Wilmore.."Multimodal strategies to improve surgical outcome. " The American Journal of Surgery, Vol. 183, No. 6, 2002, pp. 630-41.
Google Scholar Crossref - Miller, Timothy E., Tong J. Gan, and Julie KM Thacker. "Enhanced recovery pathways for major abdominal surgery." Anesthesiology News, 2014, pp. 1-8.
Google Scholar - Kehlet, Henrik. "Modification of responses to surgery by neural blockade." Neural Blockade in Clinical Anesthesia and Management of Pain, Vol. 11, 1998 pp. 129-75.
Google Scholar - Hughes, Michael J., et al. "Analgesia after open abdominal surgery in the setting of enhanced recovery surgery: a systematic review and meta-analysis." JAMA Surgery, Vol. 149, No. 12, 2014, pp. 1224-30.
Google Scholar Crossref