Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 4
Elevated Levels of CA-125, Estradiol and Cortisol as Prominent Markers to Diagnose Various Stages of Endometriosis in Indian Population
Ashish Ashish1, Kusum Kusum2, Sangeeta Rai3 and Royana Singh1*2Department of Obstetrics and Gynaecology, Institute of Medical Science, Varanasi, India
3Department of Zoology, Institute of Science, Banaras Hindu University, Varanasi, India
Royana Singh, Department of Anatomy, Institute of Medical Science, Banaras Hindu University, Varanasi, India, Email: royanasingh@bhu.ac.in
Received: 25-Mar-2021 Accepted Date: Apr 20, 2021 ; Published: 27-Apr-2021
Abstract
Background: Endometriosis is a chronic inflammatory disease condition that affects an estimated 176 million women worldwide. The disease causes unbearable symptoms of pelvic pain and infertility that limit the quality of reproductive life of affected women. Objective: An attempt has been made to identify certain physiological and/or hormonal factors that may behave as reliable diagnostic markers to assess the various stages of endometriosis. Design: A retrospective population-based study. Material and Methods: Questionnaire-based study was conducted on females of Eastern Uttar Pradesh and Bihar that were suffering from endometriosis. Prevalent patients were characterized in terms of their socio-demographic and clinical characteristics, including validated infertility and chronic disease registries. Results: Progression of the disease was not affected by age and Body Mass Index (BMI) of subjects. The concentration of blood sugar (fasting and PP), and levels of Serum Luteinizing Hormone (LH), Follicle Stimulating Hormone (FSH), T4, and Thyroid Stimulating Hormone (TSH) did not change as the disease progressed from stage 1 to 4. However, levels of serum estradiol, cortisol, prolactin, T3, and CA-125 increased as endometriosis progressed. There also existed close associations between CA-125, estradiol and cortisol, and stages of endometriosis. Conclusion: Elevated levels of CA-125, estradiol, and cortisol may behave as prominent diagnostic markers to assess the progression of the disease and to discriminate between various stages of endometriosis.
Keywords
Endometriosis, Infertility, Pelvic pain, Dysmenorrhea, Dyspareunia
Abbreviations
BMI: Body Mass Index, rASRM: American Society of Reproductive Medicine, PID: Pelvic Inflammatory Disease, LH: Luteinizing Hormone, FSH: Follicle Stimulating Hormone, TSH: Thyroid Stimulating Hormone
Introduction
Endometriosis is a chronic inflammatory disease condition in women, where tissues resembling endometrium, usually stromal or glandular, are located outside the uterine cavity [1,2]. Menorrhagia, dysmenorrhea, dyspareunia, dyschezia, dysuria, pelvic pain, and infertility are the prominent symptoms seen in endometriosis suffering women. Besides, factors like environmental and dietary elements, immune system, viz. cytokines, interleukins, and intrinsic anomalies in the endometrium are also associated with the disease [3,4]. Many previous studies have assessed the risk factors associated with endometriosis [4]. Age, race, alcohol usage, body mass index, cigarette smoking, and menstrual characteristics such as early age menarche, menstrual length, cycle regularity, dysmenorrhea, and menstrual flow intensity are all associated with the incidences of endometriosis [5]. Globally, one in ten women during their reproductive years (between puberty and menopause) are having endometriosis, which is about 176 million women population worldwide suffering from the disease [6,7].
Assessment of the endometriosis rate is difficult in the general female population as the definitive diagnosis requires surgical visualization [8]. Diagnosis of endometriosis is established through laparoscopy visualization at the surgery. Endometrioma and deep endometriosis, however, can be detected using imaging techniques (ultrasonography or MRI) [9]. CA-125 (Cancer Antigen 125 or Carbohydrate Antigen 125) is a protein secreted by the normal human body in small quantities, and its normal value is less than 35 U/mL [7,10]. It is produced from the endometrium and irritation of the peritoneum by infection, surgery, or during endometriosis [7]. CA-125 as a biomarker through serologic testing has been widely used for the detection of endometriosis and monitoring progressive disease [10-12]. CA-125 now has been a well-established biomarker for epithelial cell ovarian carcinoma, derived from coelomic epithelia of the endometrium, fallopian tube, ovary, and peritoneum [8]. In a study CA-125, is raised in endometriosis through stimulation of coelomic epithelia [13]. One of the studies, regarding endometrial cancer, has found that levels of CA15-3, CA125, CEA, and Prolactin were increased in comparison to AUB (Abnormal Uterine Bleeding) patients, showing CA-125 be a better marker with 52.63% sensitivity and 80.00% specificity [14]. One more study, conducted in the Iranian population, on 87 women suspected of endometriosis with pelvic pain, dysmenorrhea, or dyspareunia, has concluded that preoperative serum CA-125 can be an important predictor when surgical management is suspected, especially if the stage of the disease, lesion size, and adhesion score is undertaken [15]. Thus, CA-125 will help one to get a positive response for the correct diagnosis of endometriosis as a preliminary test. It will reduce the delayed diagnosis and will give confidence to patients and clinicians both for further investigations and therapeutic interventions.
Nowadays, endocrine therapies are also providing effective palliation with relatively little toxicity in many hormonesensitive cancers [13]. However, the response to endocrine therapy in the case of endometriosis is yet to be explored.
Despite causing debilitating symptoms of pelvic pain and infertility, and restraining the quality of life of affected women, the causative factors of endometriosis are not widely studied in Indian populations belonging to different ethnic groups. In the present study, an attempt has been made to identify certain physiological and/or hormonal factors that may behave as reliable diagnostic markers to assess the various stages of endometriosis. It is anticipated that the findings of the study may be helpful in the early and cheap diagnosis of the disease. The results may help the medicoprofessionals, scientists, and/or policymakers to modify the existing guidelines related to endometriosis treatment in India.
Materials and Methods
Classification Systems of Endometriosis
Numerous proposed systems to classify various forms of endometriosis exist mainly in the American Society of Reproductive Medicine (rASRM), which is modified and renamed into Revised American Society for Reproductive Medicine classification of endometriosis [10,16]. All of these classifications divide endometriosis into four stages related to the increasing severity of the ovaries lesions, particularly the number of endometrial implants, their depth, and adhesions; Stage I: 1-5 points indicate minimal disease i.e. few superficial implants, Stage II: 6-15 points score indicates mild disease which includes more and deeper implants, Stage III: 16-40 points for moderate disease having many deep implants, small cysts on one or both ovaries and Stage IV: >40 points indicate severe condition with many deep implants, large cysts on one or both ovaries with dense adhesions [11,17,18].
Methodology
The present retrospective study was conducted at the Department of Obstetrics and Gynaecology, Sir Sunderlal Hospital, Institute of Medical Sciences, Banaras Hindu University, Varanasi, India (25°20’N, 83°0’E) from September 2017 to September 2019. The study was questionnaire-based. A random sampling method was done, and details of the lifestyle, habits, and familial history of the patients were recorded. All subjects were of Indian ethnicity from eastern Uttar Pradesh and Bihar, the two states of northern India. Both these states have very high population density, and their population consists of individuals from all ethnic groups and every geographical region of India. The study was approved by Institutional Medical Ethical Committee (No. Dean/2018/EC/936) to resolve ethical issues related to patient recruitment, sample collection, and use of diagnostic methods for examining endometriosis. All subjects were informed about the study and their consents were taken before the start of the study.
Inclusion Criteria: Female patients of 18-50 year age group, and were diagnosed to have endometriosis and BMI less than 32 kg/m2 were included in the study.
Exclusion Criteria: Patients with other causes of chronic pelvic pain, including infectious diseases, Pelvic Inflammatory Disease (PID), adhesions due to previous surgeries or infections were excluded from the study.
Clinical Characteristic: Points noted were the age of subjects, residence, physical and socioeconomic status, type of infertility, duration of infertility, menstrual cycle-age of onset, frequency, and its flow, an association of symptoms like dysmenorrhoea, dyspareunia, chronic pelvic pain, urinary symptoms and their correlation to the stage of endometriosis.
Physical Examination: Findings were analyzed concerning BMI, abdominal/adnexal masses, mobility of uterus, and the presence of adnexal tenderness.
TVS and MRI Finding: Advance technology of imaging methods were suggested for the detection of deep-infiltrating lesions. MRI and computed tomography, including ultrasound were evaluated.
Laparoscopic Findings: Diagnostic laparoscopy, a gold standard tool for direct visualization of the pelvis, which helps in identifying the etiology of the patients’ pain, was advised and evaluated. The laparoscopic staging was done based on the revised AFS scoring system, which categorizes the finding into four stages.
Statistical Analysis
The distributions of data sets obtained in this study were checked for normality using the Kolmogorov-Smirnoff test. Means were separated using Tukey’s test when data were normally distributed and variances were homogeneous (Bartlett’s test for equal variances). All dependent variables, viz. age, Body Mass Index (BMI), CA-125, sugar concentrations (fasting and PP), and hormonal profiling including Luteinizing Hormone (LH), Follicle Stimulating Hormone (FSH), estradiol, cortisol, prolactin, Tri-iodothyronine (T3), Tetra-iodothyronine (T4) and Thyroid Stimulating Hormone (TSH) were subjected to one way ANOVA considering different stages of endometriosis (viz. stages 1, 2, 3 and 4) as independent variables. Dependent variables (i.e. age, BMI, CA-125, sugar concentrations (fasting and PP), LH, FSH, estradiol, cortisol, prolactin, T3, T4, and TSH) were also regressed against different stages (viz. stages 1, 2, 3 and 4) of endometriosis (independent variable), and graphs displaying significant effects (p<0.05) were extrapolated. Also, dependent variables were regressed amongst each other, and graphs showing significant outcomes (p<0.05) were drawn. Moreover, Variance Inflation Factors (VIF, where VIF=1/(1-Ri2)) were calculated to examine the existence of multiple collinearities between the physiological parameters. All statistical analyses were performed using MINITAB 16 (Minitab Inc., State College, Pennsylvania, United States of America).
Results
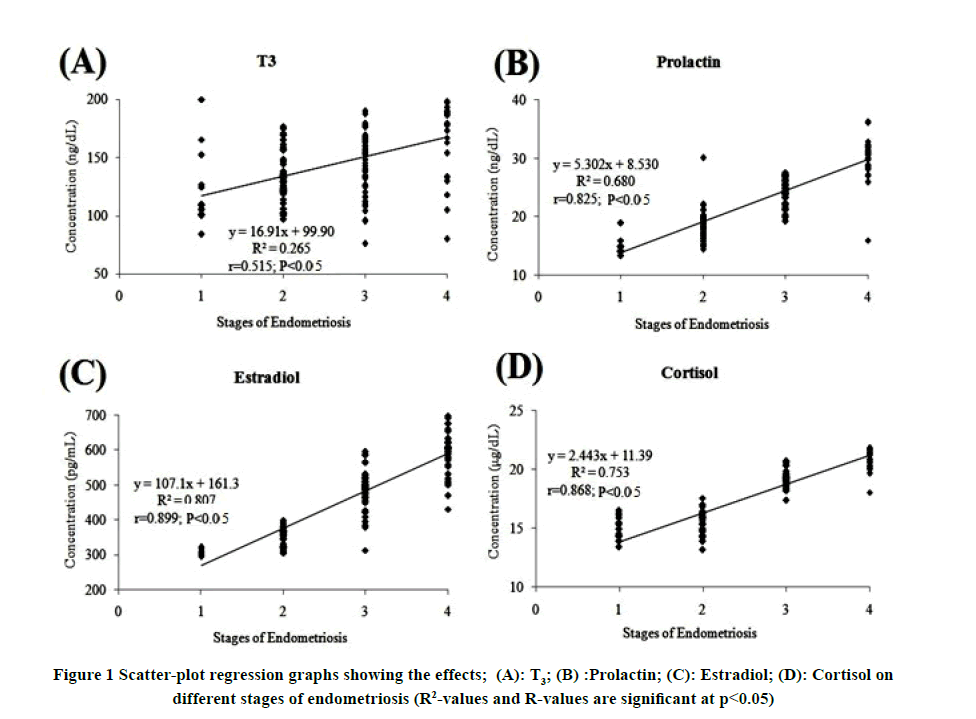
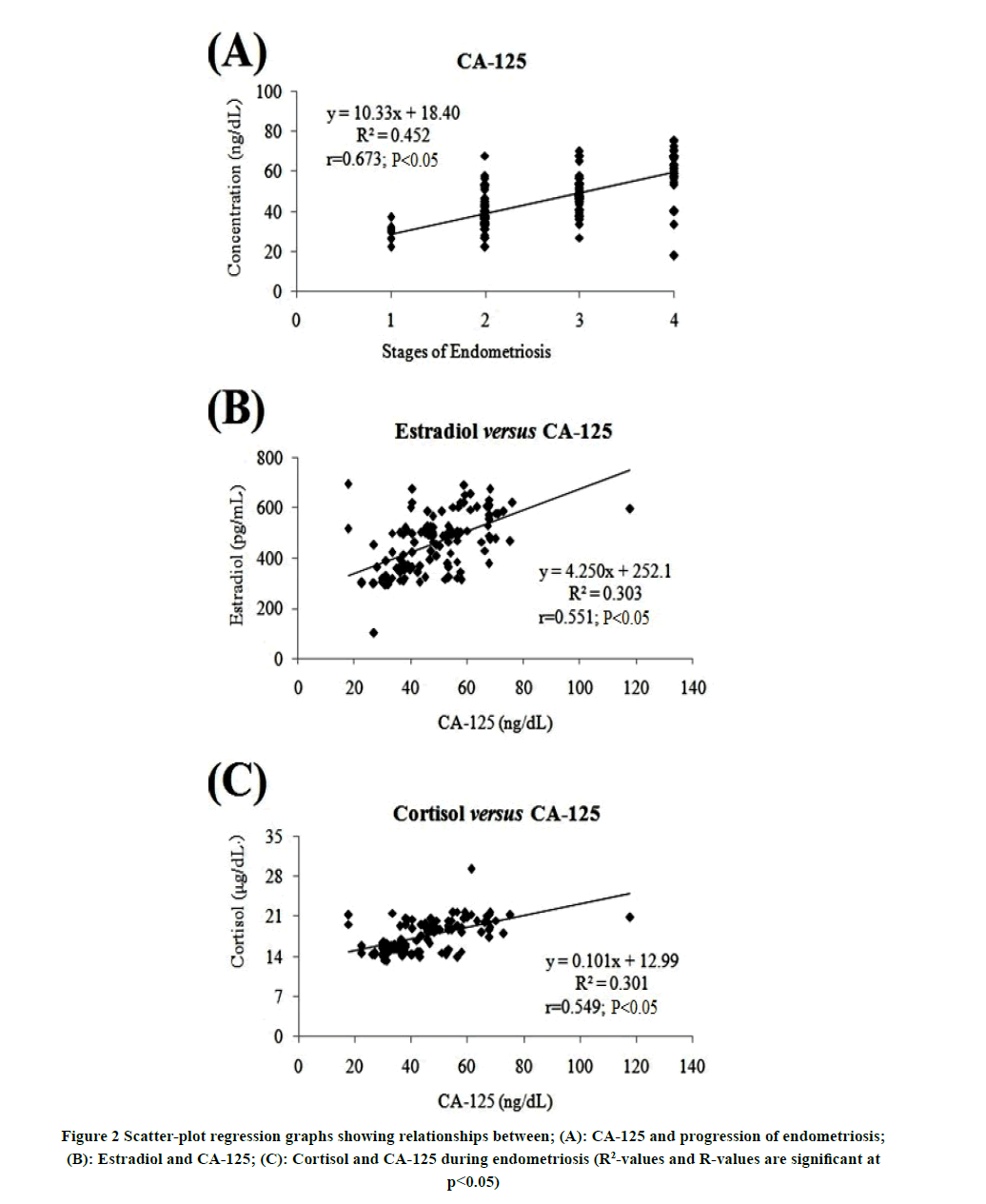
In the present study, no confounding factor was found that could significantly affect the study outcomes. Results revealed significant effects of CA-125, estradiol, cortisol, prolactin, and T3 on different stages (i.e. stages 1, 2, 3, and 4) of endometriosis (Table 1). In contrast, the effects of age, BMI, sugar concentrations (fasting and PP), LH, FSH, T3, and TSH on different stages of endometriosis were insignificant. Regression graphs revealed that with progression in the stages of endometriosis from stage 1 to stage 4, the concentration/levels of CA-125, estradiol, cortisol, prolactin, and T3 increased. However, the association of estradiol and cortisol to different stages of endometriosis was much higher than those of prolactin and T3 (Figure 1, and Figure 2A). This was further visualized from the obtained positive correlation coefficients between estradiol/cortisol and the concentrations of CA-125 as the disease progressed (Figure 2B and Figure 2C). Moreover, the values of variance inflation factors revealed that although CA-125, estradiol, and cortisol varied linearly with different stages of endometriosis, however, there existed moderate association but no multiple collinearities between the physiological parameters, i.e. between CA-125 and estradiol (VIF=1.434), and CA-125 and cortisol (VIF=1.430).
| Variable | Stage 1 | Stage 2 | Stage 3 | Stage 4 | F-value; p-value; df |
|---|---|---|---|---|---|
| (N=19) | (N=80) | (N=75) | (N=47) | ||
| Age | 32.10 ± 8.14 | 32.05 ± 6.91 | 32.53 ± 8.79 | 31.44 ± 8.91 | F=0.62; p=0.605; df=3, 193 |
| BMI (kg/m2) | 22.18 ± 1.39 | 21.54 ± 2.48 | 22.02 ± 2.34 | 21.41 ± 2.28 | F=0.96; p=0.413; df=3, 193 |
| LH | 7.20 ± (4.90-8.90) | 5.10 ± (4.20-7.55) | 5.80 ± (4.63-9.24) | 5.60 ± (3.58-7.90) | F=1.17; p=0.323; df=3, 193 |
| FSH | 14.03 ± 6.88 | 12.82 ± 6.64 | 11.74 ± 6.63 | 13.51 ± 6.86 | F=1.68; p=0.172; df=3, 193 |
| Prolactin | 15.47 ± 7.02 | 18.31 ± 2.28 | 24.37 ± 2.44 | 30.23 ± 3.03 | F=143.73; p<0.0001; df=3, 193 |
| T3 | 122.78 ± 33.20 | 134.07 ± 22.15 | 147.54 ± 25.37 | 166.40 ± 32.66 | F=23.91; p<0.0001; df=3, 193 |
| T4 | 9.09 ± 2.23 | 10.06 ± 2.80 | 9.27 ± 2.42 | 9.59 ± 2.62 | F=01.13; p=0.340; df=3, 192 |
| TSH | 2.90 ± (1.0-3.87) | 2.72 ± (1.51-3.90) | 2.44 ± (1.34-3.90) | 2.60 ± (1.73-4.22) | F=0.90; p=0.441; df=3, 193 |
| CA-125 | 29.95 ± 3.00 | 38.74 ± 8.15 | 49.10 ± 8.76 | 60.24 ± 16.68 | F=52.66; p<0.0001; df=3, 193 |
| Sugar (FA) | 100.96 ± 15.82 | 97.91 ± 15.72 | 98.59 ± 14.61 | 92.53 ± 16.36 | F=1.96; p=0.121; df=3, 212 |
| Sugar (PP) | 143.25 ± 26.47 | 126.21 ± 23.70 | 137.022 ± 27.32 | 122.49 ± 19.87 | F=2.61; p=0.055; df=3, 106 |
| Estradiol | 295.24 ± 47.79 | 352.03 ± 26.93 | 486.03 ± 50.50 | 594.00 ± 60.70 | F=230.07; p<0.0001; df=3, 148 |
| Cortisol | 14.89 ± 0.89 | 15.37 ± 0.94 | 19.22 ± 0.75 | 21.20 ± 1.96 | F=177.77; p<0.0001; df=3, 116 |
Discussion
In the present study, the progression of the disease was not affected by the age and BMI of the female patients. Similarly, the concentration of blood sugar (fasting and PP), and the levels of serum LH, FSH, T4, and TSH did not show any change as the disease progressed from stage 1 to stage 4. However, the levels of serum estradiol, cortisol, prolactin, T3, and the concentration of molecular marker CA-125 increased as endometriosis progressed from stage 1 to stage 4. Higher levels of serum cortisol and prolactin in women suffering from advanced stages of endometriosis may be associated with stress [19]. Dugan A, et al. have also reported that under prolonged stress conditions the level of serum cortisol increases [19]. It is probable that stress may be directly related to the development of endometriosis and its, further, progression to advanced stages [20,21].
Earlier studies have also shown that endometriosis is a progressive estrogen-dependent disease affecting women during their reproductive years [22,23]. Biologically active estrogen, i.e. estradiol intensifies pathological processes like inflammation and growth, and the symptoms associated with endometriosis. The availability of abundant quantities of estradiol for endometriotic tissue may probably be due to several known and unknown mechanisms. One of them is the availability of local aromatase expression [23,24].
Although previous studies have shown that women with endometriosis have no increased risk of thyroid dysfunction; however our study has recorded contradictory findings [25]. We have found increased serum T3 levels with the progressions of endometriosis from stage 1 to stage 4. Similar to our finding, it has been reported that thyroid disorders are associated with severe forms of endometriosis [26]. They found that proteins involved in thyroid metabolism were dysregulated in eutopic and ectopic endometrium of endometriotic patients, leading to resistance of ectopic endometrium T3 action. However, few others found that women suffering from endometriosis had higher rates of hypothyroidism [18].
Cancer Antigen 125 (CA-125) is a biological marker for epithelial cell ovarian cancer. There is an increase in CA 125 in endometriosis through the stimulation of coelomic epithelia. Increased serum CA-125 level in the present study may be associated with ovarian endometriomas. Increased levels of serum CA-125 with a grade of endometriosis, as recorded in our study are also consistent with the findings of many previous studies [13,27,28].
Conclusion
Results of our present study have also revealed more close association between the levels of CA-125, estradiol, cortisol, and the different stages of endometriosis than those between the disease and the levels of prolactin and T3. This close association between CA-125, estradiol, cortisol, and endometriosis is further affirmed by the increasing levels of estradiol or cortisol and increasing concentrations of molecular marker, CA-125 as the disease progressed from stage 1 to stage 4. These findings further reveal that apart from CA-125, the estradiol and cortisol may also behave as prominent diagnostic markers to assess the progression of the disease and to discriminate the different stages of endometriosis. However, more clinical-based research studies are still needed to validate the present findings.
Since no association was found between endometriosis and age, BMI, sugar concentration (fasting and PP), LH, FSH, T4, or TSH levels in the present study; hence, screening of the patients based purely on these parameters and severity of the disease, as recommended by earlier workers, may not be suggested. The present study, therefore, suggests that higher levels of CA-125, estradiol, and cortisol may confirm the progression of the disease and identifying its correct stage. And rather than quantifying numerous physiological parameters, simply assessing the levels of CA-125, estradiol, and cortisol in the patients may not only diagnose and treat the disease early but would also be cost-effective. Moreover, these days, endocrine therapies are providing effective results in hormone-sensitive cancers. Future studies may further assess the response of estradiol or cortisol-based endocrine therapies and endometriosis.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval
A questionnaire-based involving Human Participants study was completed by each patient to record the details of their lifestyle, habits, and familial history. All subjects were of Indian ethnicity from eastern Uttar Pradesh and Bihar, the two states of northern India. This study was approved by the Institutional Medical Ethical Committee (No. Dean/2018/ EC/936), and all participants provided their consent for it.
Author Contributions
Royana Singh and Ashish Ashish have equally participated in the protocol development, collection and analysis of the data, manuscript writing, and final approval. Sangeeta Rai has participated in the study design, data evaluation, drafting, and analysis. Bhupendra Kumar has contributed to data collection, manuscript concept, and design statistical data analysis.
Acknowledgments
We want to extend our sincere gratitude to Multi-Disciplinary Research Units (MRUs) Laboratory, a grant by ICMRDepartment of Health Research.
References
- Klemmt, Petra AB, and Anna Starzinski-Powitz. "Molecular and cellular pathogenesis of endometriosis." Current Women's Health Reviews, Vol. 14, No. 2, 2018, pp. 106-16.
- Riazi, Hedyeh, et al. "Clinical diagnosis of pelvic endometriosis: A scoping review." BMC Women's Health, Vol. 15, No. 1, 2015, pp. 1-12.
- Saceanu, Sidonia Maria, et al. "Endometriosis: When and how we treat." Fertility-Oriented Female Reproductive Surgery, 2017, p. 61.
- Adaji, Enemona Emmanuel, Anand S. Ahankari, and Puja R. Myles. "An investigation to identify potential risk factors associated with common chronic diseases among the older population in India." Indian Journal of Community Medicine: Official Publication of Indian Association of Preventive and Social Medicine, Vol. 42, No. 1, 2017, pp. 46-52.
- Kafaei-Atrian, Mahboobeh, et al. "The relationship between the duration of menstrual bleeding and obesity-related anthropometric indices in students." Journal of Education and Health Promotion, Vol. 8, 2019, p. 81.
- de Almeida Asencio, Fernanda, et al. "Symptomatic endometriosis developing several years after menopause in the absence of increased circulating estrogen concentrations: A systematic review and seven case reports." Gynecological Surgery, Vol. 16, No. 1, 2019, pp. 1-11.
- Zondervan, Krina T. et al. "Endometriosis." Nature Reviews Disease Primers, Vol. 4, No. 1, 2018.
- Jacobs, Ian. "Screening for ovarian cancer by CA-125 measurement." The Lancet, Vol. 331, No. 8590, 1988, p. 889.
- As-Sanie, Sawsan, et al. "Assessing research gaps and unmet needs in endometriosis." American Journal of Obstetrics and Gynecology, Vol. 221, No. 2, 2019, pp. 86-94.
- Canis, Michel, et al. "Revised American Society for Reproductive Medicine classification of Endometriosis: 1996." Fertility and Sterility, Vol. 67, No. 5, 1997, pp. 817-21.
- Medl, Michael, et al. "Serum levels of the tumour‐associated trypsin inhibitor in patients with endometriosis." BJOG: An International Journal of Obstetrics aand Gynaecology, Vol. 104, No. 1, 1997, pp. 78-81.
- Cheng, Ya-Min, Shan-Tair Wang, and Cheng-Yang Chou. "Serum CA-125 in preoperative patients at high risk for endometriosis." Obstetrics and Gynecology, Vol. 99, No. 3, 2002, pp. 375-80.
- Barbieri, Robert L., et al. "Elevated serum concentrations of CA-125 in patients with advanced endometriosis." Fertility and Sterility, Vol. 45, No. 5, 1986, pp. 630-34.
- Kumar, Nithin U., et al. "CA 125 is a better marker to differentiate endometrial cancer and abnormal uterine bleeding." African health Sciences, Vol. 18, No. 4, 2018, pp. 972-78.
- Karimi-Zarchi, Mojgan, et al. "Correlation of CA-125 serum level and clinico-pathological characteristic of patients with endometriosis." International Journal of Reproductive BioMedicine, Vol. 14, No. 11, 2016, pp. 713-18.
- The American Fertility Society. "Classification of Endometriosis." Fertility and Sterility, Vol. 32, No. 6, 1979, pp. 633-34.
- Rock, John A., and ZOLADEX Endometriosis Study Group. "The revised American Fertility Society classification of endometriosis: Reproducibility of scoring." Fertility and Sterility, Vol. 63, No. 5, 1995, pp. 1108-10.
- Parasar, Parveen, Pinar Ozcan, and Kathryn L. Terry. "Endometriosis: Epidemiology, diagnosis and clinical management." Current Obstetrics and Gynecology Reports, Vol. 6, No. 1, 2017, pp. 34-41.
- Dugan, A. L., et al. "Serum levels of prolactin, growth hormone, and cortisol in burn patients: Correlations with severity of burn, serum cytokine levels, and fatality." The Journal of Burn Care and Rehabilitation, Vol. 25, No. 3, 2004, pp. 306-13.
- Cunha-Filho, João Sabino Lahorgue da, et al. "Hyperprolactinemia and luteal insufficiency in infertile patients with mild and minimal endometriosis." Hormone and Metabolic Research, Vol. 33, No. 04, 2001, pp. 216-20.
- Wang, Guoyun, et al. "Rich innervation of deep infiltrating endometriosis." Human Reproduction, Vol. 24, No. 4, 2009, pp. 827-34.
- Bulun, Serdar E. "Endometriosis " Yen and Jaffe’s Reproductive Endocrinology, 2019, pp. 609-42.
- Bulun, Serdar E., et al. "Role of estrogen receptor-β in endometriosis." Seminars in Reproductive Medicine, Vol. 30, No. 1, 2012, pp. 39-45.
- Trukhacheva, Elena, et al. "Estrogen Receptor (ER) β regulates ERα expression in stromal cells derived from ovarian endometriosis." The Journal of Clinical Endocrinology and Metabolism, Vol. 94, No. 2, 2009, pp. 615-22.
- Petta, C. A., et al. "Thyroid autoimmunity and thyroid dysfunction in women with endometriosis." Human Reproduction, Vol. 22, No. 10, 2007, pp. 2693-97.
- Peyneau, Marine, et al. "Role of thyroid dysimmunity and thyroid hormones in endometriosis." Proceedings of the National Academy of Sciences, Vol. 116, No. 24, 2019, pp. 11894-99.
- Weisheng, Bao, et al. "Discovering endometriosis biomarkers with multiplex cytokine arrays." Clinical Proteomics, Vol. 16, No. 1, 2019, pp. 1-9.
- ETIC Endometriosis Treatment Italian Club. "When more is not better: 10 ‘don’ts’ in endometriosis management. An ETIC* position statement." Human Reproduction Open, Vol. 2019, No. 3, 2019, pp. 1-15.