Research - International Journal of Medical Research & Health Sciences ( 2020) Volume 9, Issue 7
Efficacy of Midodrine on Hemodynamics
Hessah AlHomam1*, Mariam Abdalla2, Abeer Alturki2, Bashaer Qutbaldeen3, Sarah Aljaawan2, Mohammad Alghafees4 and Hind Almodaimegh2,52College of Pharmacy, King Saud bin Abdulaziz University for Health Sciences/King Abdullah International Medical Research Center ( KAIMR), Ministry of National Guard Health Affairs, Riyadh, Saudi Arabia
3College of Pharmacy,Ibn Sina National College, Jeddah, Saudi Arabia
4College of Medicine, King Saud bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia
5Pharmaceutical Care Department, King Abdulaziz Medical City, Ministry of National Guard Health Affairs, Riyadh, Saudi Arabia
Hessah AlHomam, College of Clinical Pharmacy, King Faisal University, AlAhsa, Saudi Arabia, Tel: 966 800 303 0308, Email: Hessah.mh@hotmail.com
Received: 28-May-2020 Accepted Date: Jul 07, 2020 ; Published: 14-Jul-2020
Abstract
Objectives: To assess the use of Midodrine among patients with orthostatic hypotension and withdrawal vasopressin in King Abdulaziz Medical City (KAMC), demonstrate the effectiveness and safety of Midodrine and detect side effects to provide clear evidence of the efficacy and safety of the drug.
Methods: A retrospective cohort study was done in King Abdulaziz Medical City in Riyadh (Saudi Arabia). The study targeted adult patients who suffered from hypotension between January 2015 and January 2018. The data was extracted using the BESTCare system.
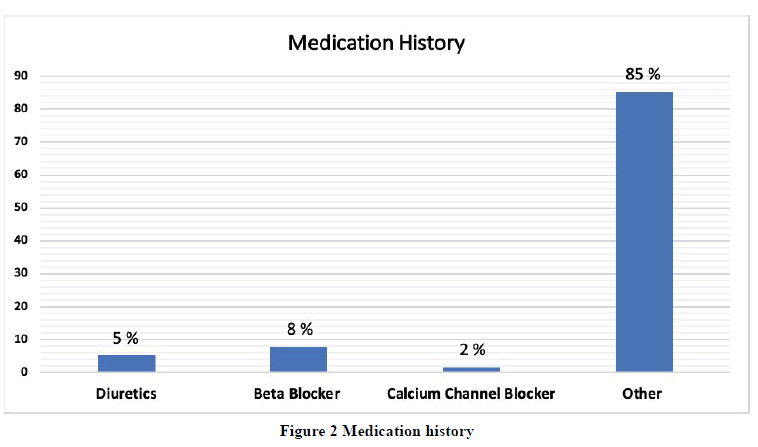
Results: A total of 173 patients were included (55.5% male and 44.5% female). The mean age of the study participants was 67.34 ± 16.0 years. The differences in patients’ parameters before and after midodrine administration were detected and analyzed. The mean difference in hemoglobin (g/l) level was significantly changed before (94.97 ± 21.9) and after (90.84 ± 20.4) the use of Midodrine (p=0.031). However, there were no significant changes in the level of the other parameters before and after the use of Midodrine. The mean dose of Midodrine was 5.3 mg, with mean treatment duration of 41.5 days, and mean hospitalization of 28.7 days. For the medication history, 8% of patients were on betablockers (n=97), 5%were on diuretics (n=64), and 2% were on calcium channel blockers (n=19).
Conclusion: Our data suggest that the administration of Midodrine does not affect patients’ hemodynamics significantly; however, it has a notable effect on decreasing hemoglobin levels
Keywords
Hemodynamics, Midodrine, Efficacy, Orthostatic hypotension
Abbreviations
HR: Heart Rate; SBP: Systolic Blood Pressure; DBP: Diastolic Blood Pressure; MAP: Mean Arterial Pressure; Scr: Serum creatinine; INR: International Normalized Ratio; Hgb: Hemoglobin; RRI: Renal Resistive Index; CO: Cardiac Output; PRA: Plasma Rennin Activity; OH: Orthostatic hypotension; US FDA: United States Food and Drug Administration; USA: United States of America; CI: Confidence Interval; ICU: Intensive Care Unit; BMI: Body Mass Index
Introduction
Midodrine is a vasopressor medication. It is a sympathomimetic drug that acts by stimulating alpha-receptors, which both noradrenaline and adrenaline work on. Midodrine is used to manage hypotension and relieve its associated symptoms, such as dizziness and fatigue, by increasing the blood pressure through constricting the blood vessels [1-4]. It is an orally administrated drug. Following administration, it metabolizes to an active form “Desglymidodrine” which binds to noradrenaline receptors [5].
Midodrine can also be used for other conditions, such as improving hemodynamics like Mean arterial blood pressure (MAP), Renal resistive index (RRI), and Cardiac output (CO) in ascites and cirrhosis [1]. A study was conducted in 2011, aimed to assess the effect of Midodrine on the hemodynamics of patients with cirrhosis. In this study, Midodrine significantly increased the Mean arterial blood pressure (MAP) and decreased the Cardiac output (CO), Plasma rennin activity (PRA), and the Renal resistive index (RRI) in cirrhotic patients with ascites [1]. The results showed that for pretreatment, MAP in group I (93.4 ± 4.7 vs. 90.6 ± 10.1) and group II (84.7 ± 3.19 vs. 84.4 ± 11.9) and CO in group I (6438.2 ± 508.8 vs. 6400 ± 1300) and group II (6833.2 ± 425.14 vs. 6800 ± 1400) values and the PRA result was 2.1 ± 1.12 [1]. Kalambokis, et al. evaluated the effect of administering 10 mg Midodrine for one week in non-azotemic cirrhotic patients with and without ascites [6]. It was associated with a significant increase in the MAP (p<0.05) and systemic vascular resistance (p<0.01) [6]. Also, it was associated with a significant decrease in the CO (p<0.05) and HR (p<0.01) [6].
Although Midodrine tolerability is considered safe in most patients, few side effects were noticed, including piloerection, general paresthesia or pruritus, chills, and urinary retention in a small percentage of people [7]. Midodrine does not affect insulin and uric acid levels nor serum lipid profile [7]. It is contraindicated in people with severe heart diseases, acute kidney diseases, urinary retention, and thyrotoxicosis. Also, it should not be used in people with excessive supine hypertension [8]. Many studies demonstrated that acute oral administration of Midodrine is related to a significant increase in systemic hemodynamics in patients with ascites, renal perfusion, or chronic hypotension [5,9].
Orthostatic hypotension (OH) is a chronic neurodegenerative disorder caused by the dropping of systolic blood pressure of at least 20 mmHg, or diastolic blood pressure of at least 10 mmHg when the patient stands up. This condition can also affect the quality of life. It results in cerebral hypoperfusion symptoms such as dizziness and blurring of vision. It also may result in substantial morbidity and mortality from associated fainting and falls. Orthostatic hypotension usually affects older adults and may increase with age. The percentage can reach up to 16.2% in people above 65 years old [7,10,11].
The goal of therapy in orthostatic hypotension is to improve symptoms and prevent falls. Stoppage of medications, such as (diuretics, α-1 adrenergic antagonists, and tricyclic antidepressants) may cause OH. The use of compression garments and drinking sufficient amounts of water can be used as management strategies for orthostatic hypotension [10]. If the previous treatments did not work, a switch to medical treatment is needed. According to the European Federation of Neurological Societies, fludrocortisone, a synthetic mineralocorticoid analog, considered the first-line treatment for OH. However, it is not approved for OH by US FDA due to adverse effects such as congestive heart failure, while Midodrine, a prodrug for the active metabolite Desglymidodrine alpha-1 agonist, is the only US FDA approved drug to manage OH and its clinical symptoms. It may cause hyperlipidemia and hyperglycemia [7,10].
However, in 2017, a retrospective cohort study conducted in the USA, which evaluated the relative safety of Midodrine and fludrocortisone found that the initiation of Midodrine for patients with OH was associated with a significantly lower incidence of hospitalization compared to fludrocortisone (95% CI, 1.02-1.4) [10].
A placebo-controlled, randomized, multicenter study evaluated the effectiveness of Midodrine in the treatment of OH; the study reported that Midodrine has no related incidence of supine hypertension. It can reduce the recurrence of blood pressure drop after standing up, the severity of falls and syncope, and cause an increase in blood pressure and vascular tone (p=0.0131) [11]. Also, a systematic review evaluated the role of Midodrine in patients with recurrent reflex syncope, and symptomatic orthostatic hypotension showed that Midodrine improved the outcomes in patients with these conditions [12]. On the other hand, a multicenter, randomized, placebo-controlled trial conducted in the USA and Australia assessed the use of Midodrine as adjunctive therapy in reducing the duration of therapy and hospitalization. Midodrine use reduced the OH levels; it increased the standing systolic blood pressure by 22 mmHg (28%, p<0.001 versus placebo) [8]. They suggested that Midodrine improves clinical outcomes in patients with secondary or orthostatic hypotension. The safety and effectiveness of Midodrine among the Saudi population is not studied yet. This study aimed to evaluate the effect of Midodrine use on the hemodynamic parameters of non-cirrhotic Saudi patients.
Methods
Study Design
Observational retrospective cohort study.
Ethics Approval
The study was approved by the Research Ethics Committee of King Abdullah International Medical Research Center.
Study Sites
This study will be conducted at King Abdulaziz Medical City (KAMC), a tertiary academic hospital located in Riyadh, Kingdom of Saudi Arabia. The hospital has expanded over the years with a bed capacity that now has reached 1501. The study targeted adult patients who suffer from hypotension between January 2015 and January 2018 with the exclusion of patients with an accompanying case of liver cirrhosis
Data Collection
Data collection will be done using (Best care) electronic health records. Also, pharmacy records will be reviewed for medication history. Patients who are admitted to cardiac wards will be reviewed using the Apollo system.
Collected Data
• Age
• Gender
• Weight
• BMI
• Physical assessment and laboratory findings (before and after starting the use of midodrine)
• Medical history
• Medication history
• Etiology of OH
• Patient’s setting when use midodrine
• The prescription of Midodrine for hypotension
• Dose of Midodrine
• Length of treatment
• Occurrence of side effects of midodrine
• Severity of side effect
• Occurrence of serious adverse events
• Total length of hospitalization
Data Analysis
The data were entered and complied by using Microsoft Excel 2010 and were analyzed by using the statistical software SPSS 22.0 version (IBM, USA). In the present study, data were analyzed with the use of necessary statistical methods to achieve the objectives of the study. The quantitative data were expressed in Mean and Standard Deviation. The qualitative data were expressed as frequency and percentages. The mean comparison of before and after measurement of the various clinical variables was made by using the paired t-test. A p<0.05 was considered statistically significant.
Results
A total of 173 patients were included in this study. 96 (55.5%) were male and 77 (44.5%) were female. The mean age of the study participants was 67.34 ± 16.0 (20-98) years and weight 70.2 ± 18.4 (Range: 38-150) Kgs (Table 1). Out of the study participants, 58.4% of them were ICU admitted patients, while 15.6% were non-ICU (Table 2).
| Socio-Demographic Variables | No. of Patients | Percentage (%) |
|---|---|---|
| Gender | ||
| Male | 96 | 55.5% |
| Female | 77 | 44.5% |
| Age (in years) (n=172)* | 67.3 ± 16.0 (Range: 20-98) | |
| Weight (in Kgs) (n=169)* | 70.2 ± 18.4 (Range: 38-150) | |
| BMI (n=169)* | 28.8 ± 14.0 (12-150) | |
BMI: Body Mass Index; *Missing value occurred
| Patient Setting (n=128)* | Frequency | Percentage (%) |
|---|---|---|
| ICU | 101 | 58.4% |
| Non-ICU | 27 | 15.6% |
ICU: Intensive Care Unit; *Missing value occurred
The differences in patient’s parameters (HR, SBP, DBP, MAP, Scr, INR, Hgb) before and after the midodrine administration were detected and analyzed (Table 3). The mean difference in hemoglobin level was significantly changed (94.97 g/l ± 21.9 g/l before) (90.84 g/l ± 20.4 g/l after) (p=0.031). However, there were no significant changes in the level of the other parameters before and after the use of midodrine.
| Clinical Variables | No. | Mean | Std. D | t-test | p-value | |
|---|---|---|---|---|---|---|
| Heart Rate (b\m) | Before | 161 | 84.63 | 16.45 | -0.979 | 0.329 |
| After | 161 | 86.29 | 17.98 | |||
| Systolic BP (mmHg) | Before | 166 | 110.2 | 22.47 | 0.357 | 0.721 |
| After | 166 | 109.38 | 23.27 | |||
| Diastolic BP (mmHg) | Before | 166 | 58.92 | 14.98 | 0.271 | 0.786 |
| After | 166 | 58.51 | 14.35 | |||
| MAP (mmHg) | Before | 86 | 70.65 | 13.51 | -1.815 | 0.073 |
| After | 86 | 73.93 | 16.23 | |||
| Creatinine (g\L) | Before | 146 | 238.2 | 202.62 | 1.714 | 0.089 |
| After | 146 | 212.63 | 182.52 | |||
| INR | Before | 106 | 1.68 | 3.56 | 0.118 | 0.906 |
| After | 106 | 1.42 | 0.965 | |||
| Hemoglobin (g\L) | Before | 144 | 94.97 | 21.99 | 2.18 | 0.031* |
| After | 144 | 90.84 | 20.42 | |||
The mean dose of midodrine was 5.3 mg, with mean treatment duration of 41.5 days, and mean hospitalization of 28.7 days (Table 4).
| Clinical Variables | Mean | Std. Dev | Range |
|---|---|---|---|
| Dose* | 5.3 | 2.8 | 2-15 |
| Length of Treatment* | 41. 5 | 79.1 | 3-777 |
| Length of Hospitalization* | 28.7 | 20.1 | 1-92 |
*Missing value occurred
Comorbidities
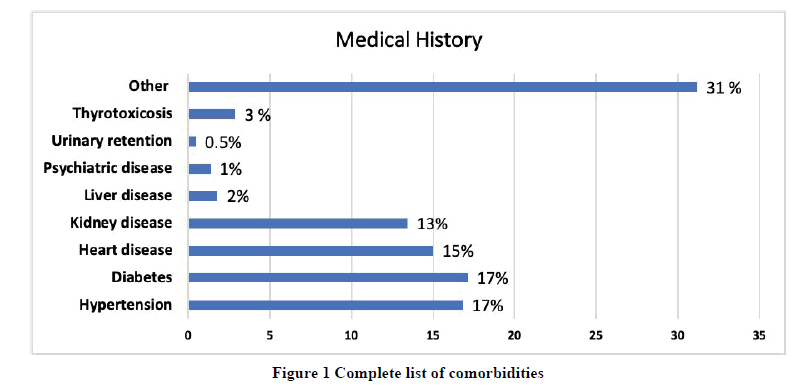
The most prevalent comorbidity identified was Diabetes mellitus, which was found in 17% of the patients (n=113) followed by hypertension (17% [n=111]), Heart diseases (15% [n=99]), Kidney diseases (13% [n=89]),Thyrotoxicosis (3% [n=19]), Liver diseases (2% [n=12]), Psychiatric diseases (1% [n=9]), and Urinary retention (0.5% [n=3]). The complete list of comorbidities can be viewed in Figure 1.
Medication History
When it comes to the medication history of the patients, 8% of the patients were on beta-blockers (n=97), 5% were on diuretics (n=64), and 2% were on calcium channel blockers (n=19) (Figure 2).
Discussion
The mean differences in mean atrial pressure of the study participants before and after the administration of midodrine were not statistically significant. However, in a study conducted in mayo clinic, 2018, the use of midodrine was associated with a significant increase in median MAP within 24 hours after administration of midodrine (p<0.01) [13]. In another study conducted in China, the use of midodrine in hemodialysis patients was associated with a significant increase in the MAP during hemodialysis (79.5 +/- 4.9 to 85.0 +/- 5.1 mmHg, p<0.05) [14].
In our study, the mean difference in hemoglobin level was significantly changed (94.97 ± 21.9 g/l before) (90.84 ± 20.4 g/l after) (p=0.031), while there were no significant changes in the level of the HR, SBP, DBP, Scr, and INR of the study participants. In a systematic review and meta-analysis did by Parsaik, et al. in the USA, the study evaluated the efficacy and safety of midodrine in OH. They found that midodrine administration was significantly associated with a change in the standing SBP (p<0.001). However, the mean change in SBP was 4.9 mmHg (p=0.65) and the mean change in MAP from supine to standing was -1.7 mmHg (p=0.45) [15].
The use of low and high doses of midodrine was associated with the same effect in the hemodynamic parameters. However, the only significant effect of the Midodrine administration was on the hemoglobin level.
Conclusion
Our data suggest that the administration of oral Midodrine does not affect patients’ hemodynamics significantly; however, it has a notable effect on decreasing hemoglobin levels.
Declarations
Acknowledgments
The authors would like to thank King Abdullah International Research Center (KAIMRC) for its support and assistance in conducting this project. Also, the team would like to express their gratitude for the appreciated contribution of Dr. Senthilvel Vasudevan.
Conflicts of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Oda, Abdel Moaty A., et al. "Hemodynamic effects of 3 months of therapy with midodrine in cirrhotic patients with and without ascites." Egyptian Liver Journal, Vol. 1, No. 2, 2011, pp. 61-68.
- Low, Phillip A., and Wolfgang Singer. "Management of neurogenic orthostatic hypotension: An update." The Lancet Neurology, Vol. 7, No. 5, 2008, pp. 451-58.
- Low, Phillip A., et al. "Efficacy of midodrine vs placebo in neurogenic orthostatic hypotension: A randomized, double-blind multicenter study." JAMA, Vol. 277, No. 13, 1997, pp. 1046-51.
- Wright, R. A., et al. "A double-blind, dose-response study of midodrine in neurogenic orthostatic hypotension." Neurology, Vol. 51, No. 1, 1998, pp. 120-24.
- Angeli, Paolo, et al. "Acute effects of the oral administration of midodrine, an α-adrenergic agonist, on renal hemodynamics and renal function in cirrhotic patients with ascites." Hepatology, Vol. 28, No. 4, 1998, pp. 937-43.
- Kalambokis, Georgios, et al. "Effects of a 7-day treatment with midodrine in non-azotemic cirrhotic patients with and without ascites." Journal of Hepatology, Vol. 46, No. 2, 2007, pp. 213-21.
- McClellan, Karen J., Lynda R. Wiseman, and Michelle I. Wilde. "Midodrine." Drugs and Aging, Vol. 12, No. 1, 1998, pp. 75-86.
- Anstey, Matthew H., et al. "Midodrine as adjunctive support for treatment of refractory hypotension in the intensive care unit: A multicenter, randomized, placebo controlled trial (the MIDAS trial)." BMC Anesthesiology, Vol. 17, No. 1, 2017, pp. 1-7.
- Obiedallah, Ahmed A., et al. "Effect of midodrine in patients with liver cirrhosis and refractory ascites." American Journal of Internal Medicine, Vol. 5, No. 1, 2017, pp. 12-17.
- Grijalva, Carlos G., et al. "Fludrocortisone is associated with a higher risk of all‐cause hospitalizations compared with midodrine in patients with orthostatic hypotension." Journal of the American Heart Association, Vol. 6, No. 10, 2017, p. e006848.
- Smith, William, et al. "Clinical benefit of midodrine hydrochloride in symptomatic orthostatic hypotension: A phase 4, double-blind, placebo-controlled, randomized, tilt-table study." Clinical Autonomic Research, Vol. 26, No. 4, 2016, pp. 269-77.
- Izcovich, Ariel, et al. "Midodrine for orthostatic hypotension and recurrent reflex syncope: A systematic review." Neurology, Vol. 83, No. 13, 2014, pp. 1170-77.
- Rizvi, Mahrukh S., et al. "Trends in use of midodrine in the ICU: A single-center retrospective case series." Critical Care Medicine, Vol. 46, No. 7, 2018, pp. e628-33.
- Lin, Yuh-Feng, et al. "Midodrine improves chronic hypotension in hemodialysis patients." The American Journal of the Medical Sciences, Vol. 325, No. 5, 2003, pp. 256-61.
- Parsaik, Ajay K., et al. "Midodrine for orthostatic hypotension: a systematic review and meta-analysis of clinical trials." Journal of General Internal Medicine, Vol. 28, No. 11, 2013, pp. 1496-503.