Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 1
Effectiveness of Myofascial Release Technique with Stretching versus Myofascial Release Technique in Patients with Plantar Fasciitis
Laizu Yeasmin Lipa1, Abhijit Kalita2 and Abhijit Dutta3*2Assistant Professor, Physiotherapy Programme, Assam Down Town University, India
3Associate Dean, Faculty of Paramedical Sciences Assam down town University, Panikhaiti, Guwahati, Assam, India
Abhijit Dutta, Associate Dean, Faculty of Paramedical Sciences Assam down town University, Panikhaiti, Guwahati, Assam, India, Email: abhijitdpt@gmail.com
Received: 02-Dec-2020 Accepted Date: Jan 22, 2021 ; Published: 29-Jan-2021, DOI: o
Abstract
Background: Plantar Fasciitis is a common cause of heel pain which occurs in the second most to weight-bearing and prolong standing occupation, injury, accidental movement in daily life. Degenerative changes can cause acute & chronic inflammation and calcification at the origin of the plantar fascia and bony traction spur formation. It is often characterized by progressive pain with weight-bearing, especially the first few steps in the morning or after periods of inactivity typically present with inferior heel pain often persist for months or even years Objective: The purpose of the study was to determine the effects of MFR technique for patients with plantar fasciitis. Methods and Measures: 30 subjects were participated in the study and randomly divided into 2 groups (n=15). Group-A (control) was treated by MFR with US technique and Group B (experimental) was treated by MFR with Ultrasound (US) with stretching technique. Before and after receiving treatment, the 30 subjects of both groups were assessed by Visual Analog Scale (VAS) and Foot Function Index (FFI) of ankle joint. Results: The results were analyzed statistically by using a paired t-test and independent t-test. In a comparison of both groups, the mean values of VAS (t=4.25) and FFI (t=4.53) are highly significant (p=0.00). It has been stated that MFR with the Stretching technique is more effective in PF management than only MFR technique. Conclusion: The study concluded that the MFR with Stretching is more precise and beneficial than only MFR technique in case of relieving pain & increasing functional ability in terms of VAS and FFI.
Keywords
Plantar fasciitis, Stretching
Abbreviations
Myofascial Release (MFR), Visual Analog Scale (VAS), Foot Function Index (FFI), Ultrasound (US)
Introduction
Plantar Fasciitis (PF) is classified as a syndrome that results from repeated trauma to the plantar fascia at its origin on the calcaneus [1]. The most common theory is repetitive partial tearing and chronic inflammation of the plantar fascia at its insertion on the medial tubercle of the calcaneus [2,3]. Studies report that faulty biomechanics is a major cause of plantar fasciitis. Subjects having either a lower or higher arched foot can experience plantar fasciitis. Patients with lower arches have too much motion, whereas patients with higher arches have too little motion both leading to the pathology of PF [4]. Plantar fasciitis has been experienced by 10% of the population [5]. Approximately 2 million people in the US are treated annually for plantar fasciitis [6-9]. The chief initial complaint is typically a sharp pain in the inner aspect of the heel and arch of the foot or a fatigue-like sensation in the medial arch of the foot after prolonged periods of standing, especially on unyielding cement surfaces [10-13]. The plantar fascia supports the medial longitudinal arch by transmitting forces between the heel and forefoot during the late stance to toe-off phases of gait. Degenerative changes can cause acute and chronic inflammation and calcification at the origin of the plantar fascia and bony traction spur formation [14]. In the presence of aggravating factors, the repetitive movement of walking or running can cause micro-tears in the plantar fascia. The affected site is frequently near the origin of the plantar fascia at the medial tuberosity of the calcaneus [5]. The histologic analysis demonstrates marked thickening and fibrosis of the plantar fascia along with collagen necrosis, chondroid metaplasia, and calcification [15,16]. Although plantar fasciitis has historically been assumed to be primarily an inflammatory process, these findings suggest a principally degenerative mechanism, leading some authors to suggest that “plantar fasciosis” may be a more histologically accurate term [15,17]. PF usually develops due to the coexistence of many etiologic factors. Although the etiology is not clear, identifying the risk factors playing a role in the occurrence of plantar fasciitis is crucial for both the identification of etiology and the successful management of preventable risk factors [18,19].
Myofascial therapy can be defined as “the facilitation of mechanical, neural and psychophysiological adaptive potential as interfaced by the myofascial system” [20]. Fascia is located between the skin and the underlying structure of muscle and bone; it is a seamless web of connective tissue that covers and connects the muscles, organs, and skeletal structures in our body. Muscle and fascia are united forming the myofascial system. The purpose of deep myofascial release is to release restrictions (barriers) within the deeper layers of fascia. This is accomplished by a stretching of the muscular elastic components of the fascia, along with the crosslinks, and changing the viscosity of the ground substance of the fascia [21]. Direct MFR seeks for changes in the myofascial structures by stretching, elongation of the fascia, or mobilizing adhesive tissues. There can be a misconception that the direct method is violent and painful. It is not essentially aggressive and painful, as the practitioner moves slowly through the layers of the fascia until the deep tissues are reached. Indirect myofascial release intends to allow the body’s inherent ability for self-correction returns, thus eliminating pain and restoring the optimum performance of the body. Self-myofascial release is when the individual uses a soft object to provide MFR under their power. Usually, an individual uses a soft roll, or ball (tennis ball, soccer ball) on which to rest one’s body weight, then, by using gravity to induce pressure along the length of the specific muscle or muscle groups, rolls their body on the object, slowly (1-2 seconds an inch), allowing for the fascia to be massaged. Upon any sharp pain, the individual must back up and hold the position, to not force undue stress upon the fascia and muscle. Stretching is defined as the behavior a person adopts to recover, reducing stiffness or soreness, increase or maintains their range of movement. This behavior includes passive and active stretching, which can be in the form of exercise or with the assistance of another person (therapist/trainer). Stretching therefore is how the ROM can be increased, but it is not the only one. There are several ways to achieve ROM improvements depending on the processes associated with the loss of ROM [22]. However, the discomfort level of stretching often has been prescribed as tension remaining below a pain threshold, without considering that an optimal discomfort and tension level may be obtained in a different position that results in the more effective achievement of a new ROM [22,23].
Materials and Methodology
This is an experimental study design, conducted for duration of 12 months, where pre and post study design will be used. A sample of 30 subjects was distributing randomly in two groups Group A-15 subjects (Control Group-MFR with US), Group B-15 subjects (Experimental Group-MFR with US with Stretching). These subjects were referred by the consultant physiotherapist/physician and orthopedic surgeons. All the subjects were required to sign a consent form before participation in the study. A convenient sampling method has been used. To avoid the consequences of drop out of subjects from this study and any further difficulty in carrying the research; a convenient sampling method was taken. The samples included in the study were, prolonged standing patients, both genders were acceptable, subject’s ages of 25-50 years, subjects having sharp pain on the first step in the morning, chronic pain (>90 days) from previously diagnosed plantar fasciitis, no history of surgery to the affected anatomy, no alternative treatment procedures within the last 90 days, chronic plantar fasciitis, both unilateral and bilateral diagnosis, and clinical presentation were included, VAS and FFI grade, subjects would be having pain at the first step in the morning at least 2-5 VAS scale score, willingness to complete treatment and post-treatment regimen as described, patients who have provided written and verbal informed consent. Subjects undergoing prior orthopedic surgery, serial casting in past 6 months; taking oral drugs; having severe limitations in passive range of motion at lower extremities; having any cognitive and perceptual disorders; contracture, any deformity on hip, back, knee, ankle; any metallic implants in the ankle joint; any sensory problem, diabetes neuropathy; having chronic venous insufficiency, patients currently enrolled in any other non-conservative, device, or investigational new drug clinical trial, or who have participated in a clinical study involving the plantar fascia, or any other clinical study involving an investigational product 30 days before enrolment; received previous treatment in the symptomatic limb (not including conservative treatment) were excluded from the study. The study proposal had been accepted by the ethical committee and the samples were collected from Assam Down Town University OPD and Physiotherapy Department, Down Town Hospital.
Outcome Measures
VAS (Visual Analog System) and FFI-R (Foot Function Index-Revised)
Procedure
Subjects suffering from heel pain due to inflammation of fascia, trauma, prolonged standing, excessive weight-bearing, improper exercise, poor quality of the shoe, etc. from Assam downtown College OPD and Downtown Hospital were approached with the proposal of the study. The subjects were screened according to the inclusion and exclusion criteria. Those fulfilling the criteria were explained in detail about the study and written informed consent, in their preferred language, and were obtained from the subjects willing to participate. The subjects were allocated in two different treatment groups, Group-A (Myofascial Release with Ultrasound) and Group-B (Myofascial Release with Ultrasound with Stretching) by random sampling, consisting of 15 subjects in each. For each subject, demographic data was collected.
The demographic data and baseline assessment/pre-intervention data of the outcome measures were taken. Then intervention was given according to the group for six weeks. After completing the therapeutic session of 6 weeks, postintervention/ final data of the outcome measures was taken.
Interventions
GROUP A: Received Myofascial Release technique with Ultrasound, which was done actively and passively.
• Myofascial Release was performed for 20 repetitions.
• Ultrasound for 5 mins using continuous mode with frequency 1 MHz is given four times in a week for 6 weeks.
• A total of 24 treatments in 6weeks
Myofascial Release for Group A
Stage 1: Advanced Technique
Patient position: Supine lying.
Therapist position: Sitting in front of the leg.
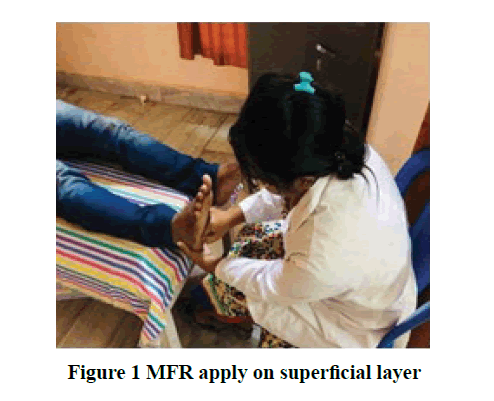
The patient in supine lying and the therapist will sit in front of the patient’s leg (Figure 1). The ankle should dorsiflex during applied MFR. The therapist uses their hand in a concave position and dorsum of the hand. Apply MFR with the dorsal part of the hand and give pressure over the superficial layer by sliding towards the calcaneum from the affected area.
Stage 2: For deep tissue release
Patient position: Prone lying.
Therapist position: Standing on the bedside.
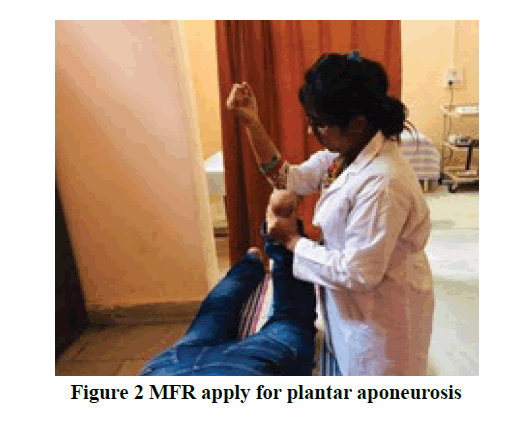
The patient is prone to lying with flexion of the knee and the therapist is in a standing position beside the bed (Figure 2). The ankle is in a normal position. The therapist holds the anterior part of the ankle by their hand and with another forearm applying myofascial and give pressure towards the affected side for plantar aponeurosis.
Stage 3: The Achilles tendon
Patient position: Subject is prone to lying.
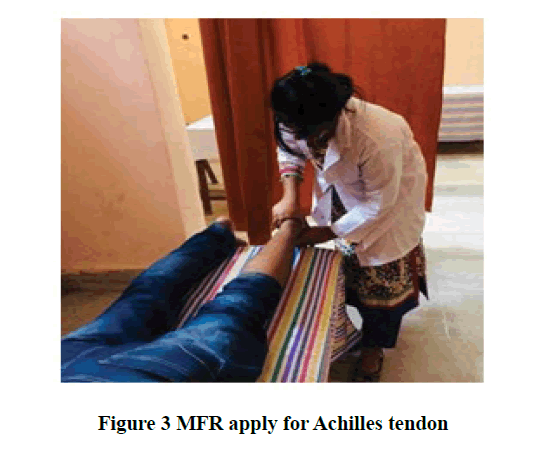
A small roll was placed under the ankle, or the foot is off the edge of the bed so that the foot and the ankle were in forced plantarflexion (Figure 3). The index finger or index finger plus the third finger pad of the distal phalanx of the caudal hand were placed over the place insertion of the Achilles tendon at the calcaneus. The index finger (or index finger plus the third finger) pad of the distal phalanx of the superior hand was laced over the musculotendinous interface of the gastrocnemius muscle with the Achilles tendon, at the superior aspect of the tendon.
Then the tissue was pushed with a 1 lb. force perpendicular into the tibia. Then the superior aspect and inferior aspect of the tendon are compressed together with about 1 lb. force, bringing the two ends of the tendon closed together and the compressive force was maintained.
Stage 4: The Gastrocnemius
Patient position: Prone lying.
The patient is prone to lying and the therapist will stand at the side of the patient’s leg. The therapist uses both hands in cross-hand pattern (Figure 4a and 4b).
Stage 5: MFR with the lacrosse ball
The patient is in a sitting position (Figure 5). The therapist will place a lacrosse ball under the foot. The patient will move the ball anteriorly and posteriorly with the footpad.
GROUP B- received Myofascial Release technique with US with Stretching.
• Myofascial release with Stretching was performed for 2 sets of 10 repetitions, with 10 seconds hold.
• Ultrasound (US) for 5 mins using continuous mode with frequency 1MHz is given four times in a week for 6-weeks.
• A total of 24 treatments in 6 weeks.
Myofascial Release for Group B
Stage 1: Advanced Technique
Stage 1: Advanced Technique
Therapist position: Sitting in front of the leg
The patient in supine lying and the therapist will sit in front of the patient’s leg (Figure 1). The ankle should dorsiflex during applied MFR. The therapist uses their hand in a concave position and dorsum of the hand. Apply MFR with the dorsal part of the hand and give pressure over the superficial layer by sliding towards the calcaneum from the affected area.
Stage 2: For deep tissue release
Patient position: Prone lying.
Therapist position: Standing beside the bed.
The patient is prone to lying with flexion of the knee and the therapist is in a standing position at the bedside (Figure 2). The ankle is in a normal position. The therapist holds the anterior part of the ankle with their hand and with another forearm applying myofascial and gives pressure towards the affected side for plantar aponeurosis.
Stretching for Group-B
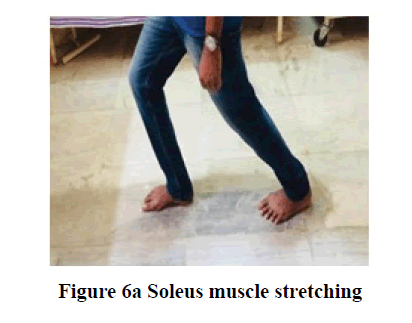
Stage 3: The Soleus
Take a half step forward. Keeping weight evenly distributed on both feet and slowly bends the knees and sinks down toward the ground (Figure 6a). Keeping the heel on the ground and feel a stretch in the back leg, just above the heel. Continue to sink slowly to deepen the stretch. Hold this stretch for about 30 sec and change side. By bending the knee, this stretch targets the Soleus and Achilles tendon, rather than the gastrocnemius (calf) muscle.
Another Technique for the Soleus:
Patient position: Supine
Therapist position: Besides the patient
Procedure: Patient in the supine position and the knee 15° flexed (Figure 6b). One hand of the therapist under the heel holds the calcaneus & another hand over the knee and then gives a stretch.
Stage 4: The Gastrocnemius
Stand about arm’s length from a wall. Lean forward and place both hands on the wall about shoulder-width apart (Figure 7a). Extend one foot (the side to be stretched) behind with the knee bent and heel on the ground. Keep the other foot closer to the wall. Lean into the wall slightly & bend the knee of the heel to be stretched (keeping the heel down) till to feel a stretch in the back of the lower leg (just above the heel) and sink slowly to deepen the stretch. Hold this stretch for about 10 sec and change the sides.
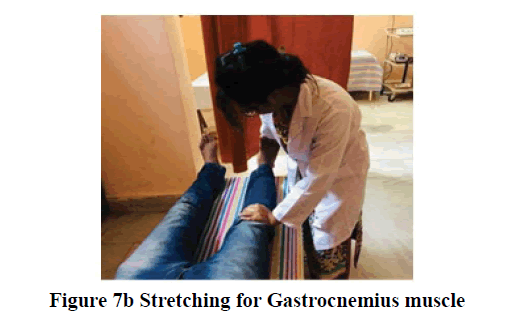
Another Technique for the Gastrocnemius:
Patient position: Supine
Therapist position: Besides the bed.
Procedure: The patient is in the supine position (Figure 7b). One hand of the therapist place under the heel and hold the calcaneus and another hand placed over the knee, then do ankle dorsiflexion and give stretch.
Data Analysis
All analysis was carried out in Microsoft Windows 7. Demographic data of patients include age is descriptively summarized. An alpha level of 0.05 was used to determine statistical significance. A statistical technique used for the analysis of the study was paired t-test and independent sample t-test. A paired t-test was performed to find out the effectiveness of myofascial release with ultrasound with stretching and myofascial release with ultrasound in plantar fasciitis management. On the other hand, an independent sample t-test was carried out to compare both groups i.e. between the control group and the experimental group.
Results
In this study, the mean age of Group-A was 44.47 ± 3.79 and in Group-B was 45.40 ± 3.22 (year) (Table 1 and Figure 8). There is no significant difference in mean age between these two groups.
| Group A | Age (Mean ± SD) | 44.47 ± 3.79 |
| Group B | Age (Mean ± SD) | 45.40 ± 3.22 |
Table 1: Demographic information
Analysis and Interpretation
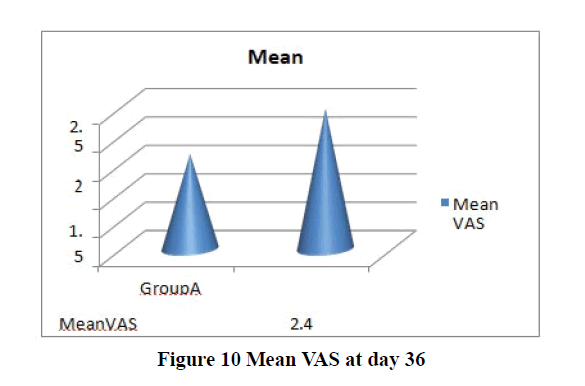
Intra-Group analysis of Group A and Group B of VAS is outlined in the table and figures below (Table 2 and Figure 9,10).
The above Table 2 is constructed to see whether MFR with US with stretching or MFR with US is effective for patients with plantar fasciitis.
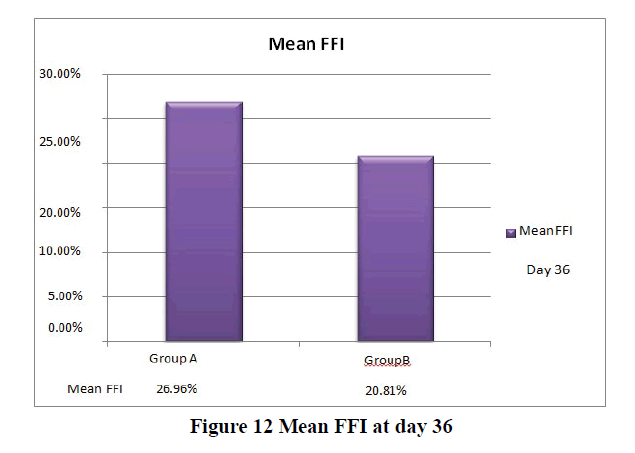
Intra-Group analysis of Group-A and Group-B of FFI is outlined in table and figures (Table 3 and Figure 11,12) below
| Group | VAS | Mean ± SD | N | t | df | p |
| Group A | Before Treatment | 3.47 ± 0.74 | 15 | 7.41 | 14 | 0 |
| After Treatment | 1.67 ± 0.62 | 15 | ||||
| Group B | Before Treatment | 3.47 ± 0.83 | 15 | 11.25 | 14 | 0 |
| After Treatment | 2.47 ± 0.52 | 15 |
Table 2: Group analysis within groups of Group-A and Group-B of VAS
| Group | FFI | Mean ± SD | N | t | df | p |
| Group A | Before Treatment | 43.02% ± 0.023 | 15 | 13.56 | 14 | 0 |
| After Treatment | 26.96% ± 3.97 | 15 | ||||
| Group B | Before Treatment | 43.69% ± 0.026 | 15 | 21.14 | 14 | 0 |
| After Treatment | 20.81% ± 3.17 | 15 |
Table 3: Group analysis within Group-A and Group-B of FFI
The statistical interpretation shows results that pain decrease in both groups but Group-B shows better result than Group-A. In the case of VAS, it was found that in Group-A, t=7.41, which is significant (p=0.00). On another way, in Group-B t=11.25, which is also highly significant (p=0.00). In a comparison of interventions of both groups, Group-B (MFR with US with stretching therapy) is more effective in decreasing pain than Group-A (only MFR with US therapy).
In the case of FFI, there will be increased functional ability with values t=21.14 in Group-B and t=13.56 in Group-A, where both are highly significant (p=0.00). However, the comparison of results concluded that more improvement of functional ability had shown in Group-B than Group-A. Therefore, MFR with US with stretching therapy was found more effective for patients (Group-B) with plantar fasciitis to increase functional ability.
In this study, a paired t-test was performed to see the difference of all outcomes (VAS and FFI) before and after application of interventions, i.e. on 1st day and the 36th day. An Independent t-test was carried out to compare both groups, i.e. between the control group (Group-A) and the experimental group (Group-B). The tests were carried out separately for VAS and FFI.
For VAS, t=4.25 which is highly significant (p=0.00). It has been suggested that VAS decreases more when MFR with US with stretching therapy has been applied.
To see the difference of means of FFI, t=4.53, which is highly significant (p=0.00) implying that FFI decreases more when MFR with US with stretching therapy has been applied compared of the only MFR with US therapy. Interventions of both techniques have the significantly same effect, but the results of the study show MFR with the US with stretching technique is more beneficial in case of relieving pain and increasing functional ability in terms of VAS and FFI in case of ROM.
Discussion
Plantar fasciitis is a disease condition that can be treated with a wide variety of physiotherapy methods alone or sometimes along with some medical intervention. Various methods of physiotherapy exist with the success of their claims without any attempts of comparing the maximal effective methods.
The study aims to determine the effectiveness of myofascial Release with US with Stretching therapy for pain management in patients with PF. For this study interventions in two groups were given, where Group-A was treated only with MFR with US therapy and Group-B treated with MFR with US with stretching therapy. For comparing the effects of the interventions were measured by outcome measuring system of VAS scale and FFI scale and objective measure ROM of ankle dorsiflexion. Both groups showed significant improvement but in the case of Group-A, the number of interventions was higher with a decrease in pain and increasing functional ability and increasing Range of Motion (ROM) compared to Group-B. For this study analysis, paired t-test and independent t-test were carried out. In the present study, both male and female patients from varieties location ages between 25 to 50 years have participated. One of the common causes of plantar fasciitis is prolonged standing & some studies revealed that plantar fasciitis is the second most common in weight-bearing and prolong standing occupation other than the athletic population [24,25]. In this study, there are no significant differences between the ages of both groups.
Using myofascial release with ultrasound with stretching technique showed better results in decreasing pain, improving functional ability, and also increasing ROM of ankle dorsiflexion. After receiving myofascial release with ultrasound with stretching therapy the independent t-value of a particular group was 4.25 in VAS and 4.53 in FFI.
Conclusion
We can conclude that in this study, there is a significant difference in the effectiveness and provided evidence to support the use of physical therapy regimen in the form of myofascial release with ultrasound with stretching therapy over the myofascial release with ultrasound therapy in the management of plantar fasciitis.
Limitations
The results only show the short term effects of the intervention and did not include long term follow up. The study tells us about the effectiveness of both the intervention in long term but was no follow-up for the interventions. Also, the strength of ankle joint musculature was not measured and patients from a limited number of places have been included into this study.
Declerations
Conflicts of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Contribution of Authors
Laizu Yeasmin Lipa: Carried out the research as a part of the curriculum of Masters in Physiotherapy which included review of literature, data collection, methodology, etc.
Abhijit Kalita: Contributed in the study as the guide and guided the candidate in topic selection, finding the researching problem, procedure of the intervention, data analysis, results
Abhijit Dutta: Contributed in the study as co-guide and guided the candidate in literature reviews, procedure, data collection, discussion and in methodology part
Acknowledgement
I express my sincere gratitude to Dr. Abhijit Dutta, Associate Dean, Faculty of Paramedical Sciences Department of Physiotherapy, Assam Downtown University, for his support and encouragement throughout the study. I extend my wholehearted thanks to my guide and teacher, Dr. Abhijit Kalita PT, Assistant Professor, Department of Physiotherapy, dtCAHS, Assam Downtown University, for his valuable guidance, support, encouragement and being a constant source of inspiration throughout the course. Finally, I express my sincere thanks to the patients who participated in the study and to all those individuals who have directly and indirectly helped in this effort of mine.
I would highly recommend individuals to stretch who want to maintain wellness through regular physical activity.
References
- Cornwall, Mark W., and Thomas G. McPoil. "Plantar fasciitis: etiology and treatment." Journal of Orthopaedic and Sports Physical Therapy, Vol. 29, No. 12, 1999, pp. 756-60.
- Henricson, Anders, et al. "The effect of stretching on the range of motion of the ankle joint in badminton players." Journal of Orthopaedic and Sports Physical Therapy, Vol. 5, No. 2, 1983, pp. 74-7.
- DiGiovanni, Benedict F., et al. "Tissue-specific plantar fascia-stretching exercise enhances outcomes in patients with chronic heel pain: a prospective, randomized study." JBJS, Vol. 85, No. 7, 2003, pp. 1270-7.
- Bolgla, Lori A., and Terry R. Malone. "Plantar fasciitis and the windlass mechanism: a biomechanical link to clinical practice." Journal of Athletic Training, Vol. 39, No. 1, 2004, pp. 77.
- Young, Brian, et al. "A combined treatment approach emphasizing impairment-based manual physical therapy for plantar heel pain: a case series." Journal of Orthopaedic and Sports Physical Therapy, Vol. 34, No. 11, 2004, pp. 725-33.
- May, Todd J., et al. "Current treatment of plantar fasciitis." Current Sports Medicine Reports, Vol. 1, No. 5, 2002, pp. 278-84.
- Dyck Jr, David D., and Lori A. Boyajian-O’Neill. "Plantar fasciitis." Clinical Journal of Sport Medicine, Vol. 14, No. 5, 2004, pp. 305-9.
- Cole, Charles, Craig K. Seto, and John D. Gazewood. "Plantar fasciitis: evidence-based review of diagnosis and therapy." American Family Physician, Vol. 72, No. 11, 2005, pp. 2237-42.
- Roxas, Mario. "Plantar fasciitis: diagnosis and therapeutic considerations." Alternative Medicine Review, Vol. 10, No. 2, 2005, pp. 83-93.
- Martin, Joe E., et al. "Mechanical treatment of plantar fasciitis: a prospective study." Journal of the American Podiatric Medical Association, Vol. 91, No. 2, 2001, pp. 55-62.
- Wearing, Scott C., James E. Smeathers, and Stephen R. Urry. "The effect of plantar fasciitis on vertical foot-ground reaction force." Clinical Orthopaedics and Related Research, Vol. 409, 2003, pp. 175-85.
- Travell, Janet G., and David G. Simons. "Myofascial pain and dysfunction: the trigger point manual." Vol. 2, Lippincott Williams & Wilkins, 1983.
- Banks, A. S., et al. "McGkamrys Comprehensive Textbook of Foot and Ankle Surgery. 3rd ed." Philadelphia: Lippincott Williams & Wilkins, 2001.
- Puttaswamaiah, Ravindra, and Prakash Chandran. "Degenerative plantar fasciitis: A review of current concepts." The Foot, Vol. 17, No. 1, 2007, pp. 3-9.
- Schepsis, Anthony A., Robert E. Leach, and J. Gorzyca. "Plantar fasciitis. Etiology, treatment, surgical results, and review of the literature." Clinical Orthopaedics and Related Research, Vol. 266, 1991, pp. 185-96.
- Snider, M. P., W. G. Clancy, and A. A. McBeath. "Plantar fascia release for chronic plantar fasciitis in runners." The American Journal of Sports Medicine, Vol. 11, No. 4, 1983, pp. 215-9.
- Lemont, Harvey, Krista M. Ammirati, and Nsima Usen. "Plantar fasciitis: a degenerative process (fasciosis) without inflammation." Journal of the American Podiatric Medical Association, Vol. 93, No. 3, 2003, pp. 234-7.
- Attar, Suzan M. "Plantar Fasciitis." Saudi Journal of Internal Medicine, Vol. 2, No. 1, 2012, pp. 13-7.
- Buchbinder, Rachelle. "Plantar fasciitis." New England Journal of Medicine, Vol. 350, No. 21, 2004, pp. 2159-66.
- Dewar, Lynne. "The Myofascial Release Manual." Physiotherapy, Vol. 87, No. 6, 2001, pp. 330.
- Barnes, John F., et al. "Pediatric myofascial release." Physical Therapy Forum, 1991.
- Katalinic, Owen M., et al. "Stretch for the treatment and prevention of contractures." Cochrane Database of Systematic Reviews, Vol. 9, 2010.
- McGill, Stuart. "Low back disorders: evidence-based prevention and rehabilitation." Champaign, IL:Human Kinetics, 2007.
- Joshua Dubin, D. C. "Evidence Based Treatment for Plantar Fasciitis." 2007.
- Bartold, Simon J. "The plantar fascia as a source of pain-biomechanics, presentation and treatment." Journal of Bodywork and Movement Therapies, Vol. 8, No. 3, 2004, pp. 214-26.