Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 2
Dosimetric Effect on Breast Cancer Patients Treated with Volumetric-Modulated Arc Therapy: Single Institutional Experience
Rania Hashem1, Zaheeda Mulla2*, Nour Ghassal3, Ayman Bokhary1, Fatimah Howladar4, Kholoud Fallatah4, Omar Iskandarani5, Mohammad Attar5 and Reem Ujaimi52Department of Oncology, King Faisal Specialist Hospital and Research Center, Jeddah, KSA
3Department of Bio-medical Physics, King Faisal Specialist Hospital and Research Center, Riyadh, KSA
4Department of Medical School, King Abdul-Aziz University Hospital, Jeddah, KSA
5Department of Radiology, Faculty of Medicine, King Abdul-Aziz University, Jeddah, KSA
Zaheeda Mulla, Department of Oncology, King Faisal Specialist Hospital and Research Center, Jeddah, KSA, Email: mulla.zaheda@gmail.com
Received: 30-Dec-2020 Accepted Date: Feb 11, 2021 ; Published: 18-Feb-2021
Abstract
Objective: To examine the dosimetric effect of Breast Cancer (BC) patients Receiving Radiotherapy (RT) with Volumetric-Modulated Arc Therapy (VMAT). Methodology: This retrospective study enrolled 53 BC women, treated with VMAT between Oct 2013 and Nov 2018. The fractionation was within 40 Gray-50 Gray (Gy) in 15-25 fractions. Dosimetric parameters, Homogeneity Index (HI), Conformity Index (CI), Mean Heart Dose (MHD), and doses to the Ipsilateral Lung (IPL) and Mean Contralateral Breast (MCB) were analyzed. Results: Dosimetric results for 50 Gy/25 Fx showed, D98% (mean ± standard deviation) was 47.5± 0.8 Gy, PTV D2% was 53 ± 0.4 Gy, and D50% was 51 ± 0.3 Gy. The maximum point dose (Dmax), mean ± SD was 110 ± (1.4) and the minimum point dose (Dmin), was 72 ± (9.1). The HI and CI were 0.11 ± 0.02 and 0.1 ± 0.07. The average MHD was 10.6 ± 3.3 Gy, and the MCB dose 4.5 ± 1.4 Gy, IPL V20Gy 31.5 ± 4.7%. For hypofractionated dose, D98% (mean dose ± SD) was 41 ± 1.6 Gy, PTV D2% was 45 ± 01.9 Gy and, D50 was 43 ± 1.8 Gy. The Dmax, mean ± SD was 111 ± (5.0) and the Dmin, mean ± SD was 75 ± (11). The HI and CI were 0.1 ± 0.02, and 0.1 ± 0.34. The average MHD was 10.5 ± 3.55 Gy, MCB 3.7 ± 1.4 G, IPL V20 Gy 31.5 ± 4.7%. Conclusion: VMAT is favorable with complex patient anatomy or when the internal mammary region is included.
Keywords
Breast cancer, Radiotherapy, VMAT, Dosimetry
Introduction
Breast cancer is the most frequently diagnosed malignancy worldwide in women [1]. Adjuvant Radiotherapy (RT) is essential in the management of breast cancer. Currently, the general principle of treating breast cancer after surgery is to irradiate the primary site breast or Chest Wall (CW) with or without the Regional Lymph Nodes (RLNs) in patients with a high risk of locoregional recurrence. RT has benefits in terms of reduced locoregional recurrence and distant metastases and increased overall survival [2-8]. However, this comes with the trade-off of radiating the surrounding Organs at Risk (OAR), such as the heart and lungs, and subsequent induced toxicity and morbidity such as radiation pneumonitis, and cardiotoxicity [9-11].
The recent decades have witnessed many advances in radiation treatment. Volumetric-Modulated Arc Therapy (VMAT) is being increasingly used in the management of breast cancer to optimize the dose distribution to the contoured target(s) while reducing the high doses to OAR, especially to the heart and ipsilateral lung, despite its disadvantage of increasing the OAR volumes that receive low dose radiation [12,13].
Several studies have compared the current treatment methods for breast cancer: three-Dimensional Conformal Ra-diotherapy (3D-CRT), Intensity-Modulated Radiation Therapy (IMRT), and VMAT [14-17]. IMRT and VMAT were found to have superior coverage and uniformity of dose to the target volume than that of 3D-CRT. Both IMRT and VMAT improved dose conformity and sparing of OAR for an optimal therapeutic ratio; however, VMAT reduced the number of Monitor Units (MU) by 30% and the treatment time by 55% [16,18,19].
This study aimed to review the dosimetric data of breast cancer patients treated with adjuvant radiotherapy to the breast/CW and nodal irradiation via VMAT at our institution. The study received ethics approval from the institutional review board.
Materials and Methods
Patients and Simulation
All patients with invasive breast cancer (left and right-sided) with the stage (PT1-T4 N1-N3 M0) were treated with surgery followed by adjuvant radiotherapy at King Abdul Aziz university hospital in Saudi Arabia, between October 2013 and November 2018, both inclusive, were selected in this retrospective study. The Research Ethics Committee of King Abdul Aziz university hospital approved this study.
All patients were simulated in the supine position with their arms over their heads using CT soma tom sensation open, version 2014A, with a CT image slice thickness of 3 mm.
Treatment Planning System (TPS)
VMAT plans were generated and optimized using Monaco treatment planning system version 5.11, with treatment energy of 6 MV, and a single isocenter.
Delineation of target and OARs: At our center, the delineation of the Clinical Target Volume (CTV) and, OARs were contoured based on the RTOG guidelines. As per our institutional protocol, the Planning Target Volume (PTV) was generated by expanding 0.5 cm from the CTV in all directions (the superior-inferior/anterior-posterior/left-right directions). The volumes inside the lung were excluded from the PTV, and the PTV was cropped 3 mm from the skin.
The CTV, PTV, and the heart were delineated by a radiation oncologist, whereas the ipsilateral, contralateral lung, spinal canal, and contralateral breast were contoured by a dosimetrist.
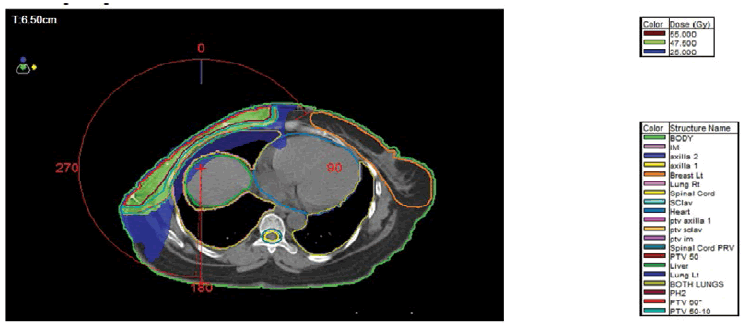
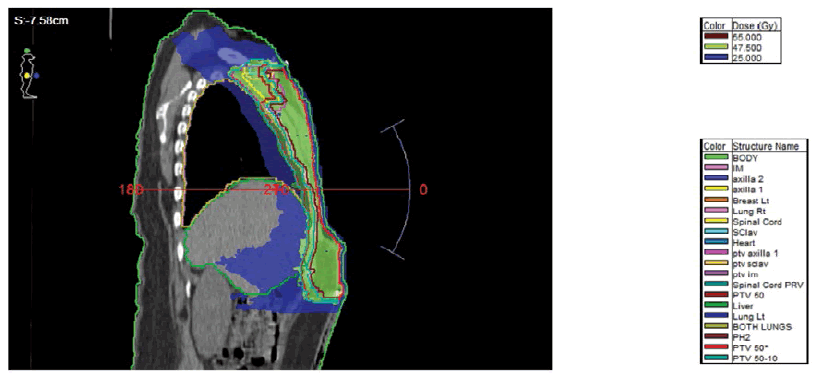
Beam Arrangement: 1 or 2 partial arcs were used depending on the patient contour and geometry. The arc increment was either (15 or 20) degrees. For right breast cancer, the arc started approximately at 60 degrees and finished at 180 degrees, whereas, for left breast cancer, it was approximately from 295 degrees to 180 degrees. The arc length at couch 0 degrees ranged from 240 degrees-250 degrees. Where there was an arc at 90 degrees couch value, the arc started at 30 degrees and stopped at 330 degrees with a length of 60 degrees. The number of control points was between 100 degrees and 180 degrees. See Figures 1 and 2 for the arc direction at 0 degrees and 90 degrees couch direction respectively.
Plan analysis
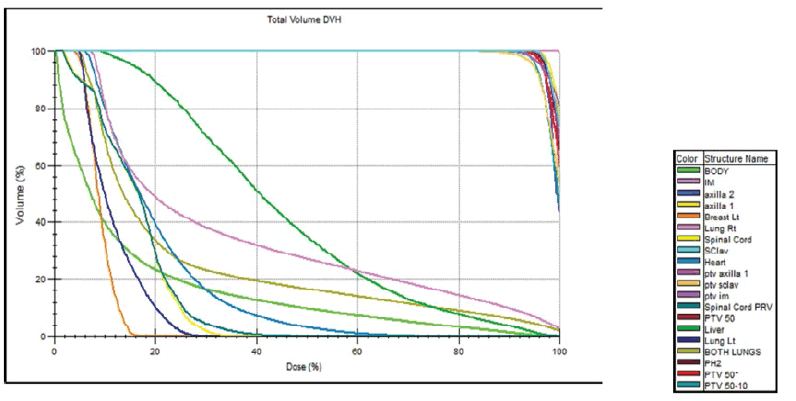
Dose-Volume Histograms (DVHs) of the treatment plans were generated to analyze target coverage and doses administered to the OARs. For plan evaluation, the following parameters were recorded. The maximum point dose (Dmax) and the minimum point dose (Dmin), the volumes of the ipsilateral lung receiving 5 Gy and 20 Gy (V5, V20), as well as the mean ipsilateral lung dose (Dmean), and were evaluated. For the heart V5, V25, and the mean heart dose were examined. For the contralateral breast, the Dmax and Dmean were reported. Furthermore, the plan qualities were evaluated by the Homogeneity Index (HI) and the Conformity Index (CI). The CI of PTV was defined as BV95%/PTV (BV95%=the volume of the body receiving 95% of the prescribed dose, and the dose Homogeneity Index (HI) of PTV was calculated according to ICRU 83 [20,21]. See Figure 3 for the display of the DVH.
VMAT QA (Plan Verification)
The absolute dose was checked using the calculated dose from the TPS at the center of the chamber and was compared with the measured dose in the 2D array (± 3%).
The fluence dose map was evaluated by a unified tool called Gamma Analysis metrics, and consists of 2 units:
Dose difference delta (D) (%).
Space Domain Distance to Agreement (DTA) (mm).
A group of points was chosen and calculated mathematically. The acceptance criteria D and DTA are usually (3%, 3 mm) or (2%, 2 mm) respectively. Finally, the plan verification depended on the number of passing points (>90%). All VMAT treatment plans passed the QA verification process.
Results
Between October 2013 and November 2018, 53 women with breast cancer who received VMAT Radiotherapy at our institution were enrolled in this study. Twenty-nine patients were right-sided, 23 patients were left-sided, while one patient was treated for bilateral breast cancer. The TNM staging of the patients was pT1-4N1-N3M0. The mean age at treatment was 45 years (range: 30-75 years). All were treated in a supine position. Thirty patients with the hypofractionated treatment regimen, 22 patients were treated with standard fractionation and one was treated with 66 Gy/33 fractions.
The prescription dose for the entire treatment volume ranged between 40-50 Gy in 15-25 fractions. Plans were optimized so that a minimum of 95% of the PTV received 100% of the prescribed dose while keeping the volume of the lung receiving 20 Gy (V20) at less than 30%-35% and the V25 of the heart at <10%, and as low mean heart dose as possible. The average treatment duration per fraction was 16 minutes; VMAT plans were optimized for the RapidArc technique in the Monaco treatment planning system. DVHs were analyzed; the dosimetric results are reported as mean value and Standard Deviation (SD) of each parameter for all patients.
Tables 1 and 2 summarize all results presented as mean values and SD for included patients.
| PTV | VMAT |
|---|---|
| V95 mean% (± SD) | 98 ± (1.18) |
| D2% (Gy) (± SD) | 53 ± (0.4) |
| D98% (Gy) (± SD) | 47.5 ± (0.8) |
| Dmax, mean (± SD) | 110 ± (1.4) |
| Dmin, mean (± SD) | 72 ± (9.1) |
| CI | 0.1 ± (0.07) |
| HI | 0. 11 ± (0.02) |
| Ipsilateral lung | |
| Dmean (Gy) (± SD) | 16.9 ± (2.1) |
| V20Gy (%) (± SD) | 31.5 ± (4.7) |
| V5Gy (%) (± SD) | 80 ± (11) |
| Heart | |
| Dmean (Gy) (± SD) | 10.6 ± (3.3) |
| V25Gy (%) (± SD) | 6.8 ± (6.7) |
| V5Gy (%) (± SD) | 78.8 ± (18) |
| Contralateral breast | |
| Dmean (Gy) (± SD) | 4.5 ± (1.4) |
| PTV: Planning Target Volume; D98% and D2%: indicating dose to 98% and 2% (near-maximum dose) | |
| PTV | VMAT Mean + SD |
|---|---|
| V95 mean% (± SD) | 98 ± (0.74) |
| D2% (Gy) (± SD) | 45± (1.9) |
| D98% (Gy) (± SD) | 41 ± (1.68) |
| Dmax, mean | 111 ± (5.0) |
| Dmin, mean | 75 ± (11) |
| CI | 0.1 ± (0.03) |
| HI | 0. 1 ± (0.01) |
| Ipsilateral lung | |
| Dmean (Gy) (± SD) | 15.1 ± (1.6) |
| V20Gy (%) (± SD) | 29.4 ± (4.6) |
| V5Gy (%) (± SD) | 74 ± (11) |
| Heart | |
| Dmean (Gy) (± SD) | 10.5 ± (3.55) |
| V25Gy (%) (± SD) | 7.1 ± (6.2) |
| V5Gy (%) (± SD) | 76 ± (21) |
| Contralateral breast | |
| Dmean (Gy) (± SD) | 3.7 ± (1.4) |
| PTV: Planning Target Volume; D98% and D2%: indicating dose to 98% and 2% (near-maximum dose) | |
On the evaluation of the plans that received a total dose of 50 Gy/25 fractions, the D98% mean dose ± (SD) was 47.5 ± 0.8 Gy, PTV D2% was 53 ± 0.4 Gy, and D50 was 51 ± 0.3 Gy. V95 was (98 ± 1.18)%. Dmax, mean ± SD was 110 ± (1.4) and Dmin, mean ± SD was 72 ± (9.1). The HI and CI were 0.11 ± 0.02 and 0.1 ± 0.07, respectively. On analyzing OAR sparing, the average mean dose to the heart was 10.6 ± 3.3 Gy, whereas V25 and V5Gy were (6.8 ± 6.7)%, and (78.8 ± 18)%, respectively. The dose to the contralateral breast was 4.5 ± 1.4 Gy. The ipsilateral lung V20Gy and V5Gy were (31.5 ± 4.7)% and (80 ± 11)% respectively.
On analysis of the target coverage for a total dose of 42 Gy/16 fractions, the D98% mean dose ± (SD) was 41 ± 1.6 Gy, PTV D2% was 45 ± 01.9 Gy and D50 was 43 ± 1.8 Gy. V95 was found to be 98.7 ± 0.74%. The Dmax, mean ± SD was 111 ± (5.0) and the Dmin, mean ± SD was 75 ± (11). The HI and CI were 0.1 ± 0.02 and 0.1 ± 0.34 respectively. While evaluating OAR, the average mean dose to the heart was 10.5 ± 3.55 Gy, whereas V25 and V5Gy were (7.1 ± 6.2)%, and (76 ± 21)% respectively. The contralateral breast dose was 3.7 ± 1.4 Gy. The ipsilateral lung V20Gy and V5Gy were (31.5 ± 4.7)% and (74 ± 11)% respectively.
Discussion
At our center, like many other centers worldwide, most breast cancer patients are treated with field-based 3D conformal RT. However, because of patient’s anatomical variation (where the patient’s arm is not raised high enough due to morbidity, when the constraint of the heart is high for 3-D conformal, and in some cases where the dose to the ipsilateral lung is not meeting the dose constraints) or when we choose to treat the internal mammary region, coverage can be challenging to achieve without exceeding normal tissue tolerance. In those situations, we choose to use advanced treatment techniques, including VMAT, to achieve better and conformal coverage, with acceptable OAR doses. This study reviewed our experience and compared it with the results of other major centers that have extensive experience in breast cancer radiotherapy.
A study conducted by Johansen, et al. and N. Supakalin concluded that VMAT has superior homogeneity and conformity in terms of PTV; furthermore, the Rapid Arc plan better spared ipsilateral lung and decreased the mean dose to the contralateral breast [18,22]. Popescu, et al. determined that compared with IMRT, VMAT achieved similar PTV coverage with shorter delivery time than IMRT, and lesser MUs [12]. According to Oliver, et al. RapidArc is qualified for producing better plans than IMRT with better dose distribution conformity [23]. The study by Nicolini, et al. concluded that VMAT indicated dosimetric improvements concerning IMRT [24]. Tuomas Virén, et al. showed that the dose coverage (V47.5Gy) was significantly superior with VMAT than with FinF and tIMRT [25]. We have also reported similar results in this study as we achieved excellent PTV coverage, with good conformity and homogeneity.
However, our heart dose was initially a concern. Although there is not a specific standard cardiac dose constraint, the aim is to keep it as low as possible [26]. The toxic effect of radiotherapy on the heart has always been a concern. However, it has recently gained more attention after the study by Darby, et al. in 2013 [11]. They found that every gray of mean heart dose increased the estimated risk of ischemic heart disease by 7.4%, starting soon after radiotherapy. Thus, efforts should be directed to minimize the irradiated cardiac volume [27]. The mean heart dose has not been routinely looked at in our plans, until recently, and the main constraint used has been the V25. We believe our mean heart dose was unacceptably high, and the use of deep inspiration breath-hold technique with or without VMAT would achieve better results [28].
The other concerning number was the V20 of the lung. There is an association between V20 and pulmonary toxicity [29]. The usual maximum acceptable dose in our daily practice is 35%. If anything, one would expect better results with IMRT/VMAT. Six of our patients had V20 in the range of 36%-41%, five of whom were treated in 2013-2014. There was no documented toxicity in those patients with V20>35%, or heart V25>10% who maintained follow-up. Our reported data for OAR is higher than the reported data of the previous studies for VMAT; variability in contouring could be a contributing factor. It is likely, however, that this was the first step in the learning curve [30,31]. In fact, in 2017-2018, the OAR constraints were much improved, with only two patients with V20>35%, or heart V25>10%.
There is a deficiency in the literature about the effect of lower doses (V5) on the heart and lung, which is commonly a concern with IMRT/VMAT; Vishruta, et al. revealed a heart V5 of 48% with VMAT [32]. VMAT alone reduced the lung dose by 20%, but the expense was an increase in V5Gy by almost 20% [31]. Cendales, et al. reported lung V5 of 78% using helical tomotherapy [33]. Our data showed that among patients treated with 50 Gy radiation, the V5Gy of the heart was 78.8 ± 18%, and that of the ipsilateral lung was 80 ± 11%. Among patients treated with 42.4 Gy, the V5Gy of the heart was 76 ± 21% and that of the ipsilateral lung was (74 ± 11)%.
Regarding Dmax and Dmin, the Dmax (110% ± 1.4) in this study, for patients treated with 50 Gy, was slightly higher than the study by Supakalin, et al. (106.99% ± 1.16), although the Dmin (72% ± 9.1), showed a better result than the latter’s (80.69% ± 7.06) [18].
Giving the lower average age of our patient population (45 years), and the potential risk of contralateral breast cancer, the dose to the contralateral breast is an important variable. Our mean dose of 4.5 Gy is comparable to what has been documented in the literature [12,13,18].
This study was the first study in the Middle East, it was meant to be a pure dosimetrist assessment, and however, a comparison with 3D plans would have also added some strength, particularly in those patients with high OAR doses. One would assume the 3D planning would have yielded even higher OAR numbers, particularly concerning high dose levels. However, occasionally, 3D planning might offer a better alternative and notably smaller lower isodose volumes.
No toxicities were recorded among the treated patient. Long-term follow-up is needed to assess late toxicity.
Conclusion
VMAT is a widely used radiotherapy technology and favoured in patients with complex anatomy or when used in higher volumes to include the internal mammary region. Our results revealed that our learning curve improved, and, in 2018 the result turns out to be consistent with previously reported results from the western world. Furthermore, continuous quality assurance assessments and education are essential to maximizing the safe and optimal use of VMAT.
Declarations
Funding
None.
Conflict of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Momenimovahed, Zohre, and Hamid Salehiniya. "Epidemiological characteristics of and risk factors for breast cancer in the world." Breast Cancer: Targets and Therapy, Vol. 11, 2019, pp. 151-64.
- Overgaard, Marie, et al. "Postoperative radiotherapy in high-risk postmenopausal breast-cancer patients given adjuvant tamoxifen: Danish Breast Cancer Cooperative Group DBCG 82c randomised trial." The Lancet, Vol. 353, No. 9165, 1999, pp. 1641-48.
- Early Breast Cancer Trialists' Collaborative Group. "Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: An overview of the randomised trials." The Lancet, Vol. 366, No. 9503, 2005, pp. 2087-2106.
- McGale, P., et al. "Effect of radiotherapy after mastectomy and axillary surgery on 10-year recurrence and 20-year breast cancer mortality: Meta-analysis of individual patient data for 8135 women in 22 randomised trials." Lancet (London, England), Vol. 383, No. 9935, 2014, pp. 2127-35.
- Ragaz, Joseph, et al. "Locoregional radiation therapy in patients with high-risk breast cancer receiving adjuvant chemotherapy: 20-year results of the British Columbia randomized trial." Journal of the National Cancer Institute, Vol. 97, No. 2, 2005, pp. 116-26.
- Nielsen, Hanne M., et al. "Study of failure pattern among high-risk breast cancer patients with or without postmastectomy radiotherapy in addition to adjuvant systemic therapy: Long-term results from the Danish Breast Cancer Cooperative Group DBCG 82 b and c randomized studies." Journal of Clinical Oncology, Vol. 24, No. 15, 2006, pp. 2268-75.
- Üçer, Ali Riza, et al. "Postmastectomy radiotherapy results of operable breast cancer." International Journal of Hematology and Oncology, Vol. 29, No. 4, 2002, pp. 126-33.
- Whelan, Timothy J., et al. "Does locoregional radiation therapy improve survival in breast cancer: A meta-analysis." Journal of Clinical Oncology, Vol. 18, No. 6, 2000, pp.1220-29.
- Darby, Sarah C., et al. "Long-term mortality from heart disease and lung cancer after radiotherapy for early breast cancer: Prospective cohort study of about 300000 women in US SEER cancer registries." The Lancet Oncology, Vol. 6, No. 8, 2005, pp. 557-65.
- Goldman, Ulla Blom, et al. "Reduction of radiation pneumonitis by V20-constraints in breast cancer." Radiation Oncology, Vol. 5, No. 1, 2010, pp. 1-6.
- Darby, Sarah C., et al. "Risk of ischemic heart disease in women after radiotherapy for breast cancer." New England Journal of Medicine, Vol. 368, No. 11, 2013, pp. 987-98.
- Popescu, Carmen C., et al. "Volumetric modulated arc therapy improves dosimetry and reduces treatment time compared to conventional intensity-modulated radiotherapy for locoregional radiotherapy of left-sided breast cancer and internal mammary nodes." International Journal of Radiation Oncology* Biology* Physics, Vol. 76, No. 1, 2010, pp. 287-95.
- Pasler, M., et al. "Node-positive left-sided breast cancer: Does VMAT improve treatment plan quality with respect to IMRT?" Radiation Therapy and Oncology, Vol. 189, No. 5, 2013, pp. 380-86.
- Reardon, Kelli A., et al. "A comparative analysis of 3D conformal deep inspiratory-breath hold and free-breathing intensity-modulated radiation therapy for left-sided breast cancer." Medical Dosimetry, Vol. 38, No. 2, 2013, pp. 190-95.
- Beckham, Wayne A., et al. "Is multibeam IMRT better than standard treatment for patients with left-sided breast cancer?" International Journal of Radiation Oncology* Biology* Physics, Vol. 69, No. 3, 2007, pp. 918-24.
- Haertl, Petra M., et al. "Treatment of left sided breast cancer for a patient with funnel chest: Volumetric-modulated arc therapy vs. 3D-CRT and intensity-modulated radiotherapy." Medical Dosimetry, Vol. 38, No. 1, 2013, pp. 1-4.
- Moon, Sung Ho, et al. "Dosimetric comparison of four different external beam partial breast irradiation techniques: Three-dimensional conformal radiotherapy, intensity-modulated radiotherapy, helical tomotherapy, and proton beam therapy." Radiotherapy and Oncology, Vol. 90, No. 1, 2009, pp. 66-73.
- Supakalin, Narudom, et al. "Comparision of different radiotherapy planning techniques for breast cancer after breast conserving surgery." Asian Pacific Journal of Cancer Prevention: APJCP, Vol. 19, No. 10, 2018, pp. 2929-34.
- Abo-Madyan, Yasser, et al. "Second cancer risk after 3D-CRT, IMRT and VMAT for breast cancer." Radiotherapy and Oncology, Vol. 110, No. 3, 2014, pp. 471-76.
- Feuvret, Loïc, et al. "Conformity index: A review." International Journal of Radiation Oncology* Biology* Physics, Vol. 64, No. 2, 2006, pp. 333-42.
- Hodapp, N. "The ICRU Report 83: Prescribing, recording and reporting photon-beam Intensity-Modulated Radiation Therapy (IMRT)." Radiation Therapy and Oncology: Organ der Deutschen Rontgengesellschaft...[et al], Vol. 188, No. 1, 2012, pp. 97-99.
- Johansen, Safora, Luca Cozzi, and Dag Rune Olsen. "A planning comparison of dose patterns in organs at risk and predicted risk for radiation induced malignancy in the contralateral breast following radiation therapy of primary breast using conventional, IMRT and volumetric modulated arc treatment techniques." Acta Oncologica, Vol. 48, No. 4, 2009, pp. 495-503.
- Oliver, Mike, Will Ansbacher, and Wayne A. Beckham. "Comparing planning time, delivery time and plan quality for IMRT, RapidArc and Tomotherapy." Journal of Applied Clinical Medical Physics, Vol. 10, No. 4, 2009, pp. 117-31.
- Nicolini, Giorgia, et al. "Simultaneous integrated boost radiotherapy for bilateral breast: A treatment planning and dosimetric comparison for volumetric modulated arc and fixed field intensity modulated therapy." Radiation Oncology, Vol. 4, No. 1, 2009, pp. 1-12.
- Virén, Tuomas, et al. "Tangential volumetric modulated arc therapy technique for left-sided breast cancer radiotherapy." Radiation Oncology, Vol. 10, No. 1, 2015, pp. 1-8.
- Jagsi, Reshma, et al. "Evaluation of four techniques using intensity-modulated radiation therapy for comprehensive locoregional irradiation of breast cancer." International Journal of Radiation Oncology* Biology* Physics, Vol. 78, No. 5, 2010, pp. 1594-603.
- Gagliardi, Giovanna, et al. "Radiation dose-volume effects in the heart." International Journal of Radiation Oncology* Biology* Physics, Vol. 76, No. 3, 2010, pp. S77-85.
- Mukesh, Mukesh, et al. "Relationship between irradiated breast volume and late normal tissue complications: A systematic review." Radiotherapy and Oncology, Vol. 104, No. 1, 2012, pp. 1-10.
- Goldman, U. Blom, et al. "Radiation pneumonitis and pulmonary function with lung dose-volume constraints in breast cancer irradiation." Journal of Radiotherapy in Practice, Vol. 13, No. 2, 2014, pp. 211-17.
- Hong, L., et al. "Intensity-modulated tangential beam irradiation of the intact breast." International Journal of Radiation Oncology* Biology* Physics, Vol. 44, No. 5, 1999, pp. 1155-64.
- Jin, Guang-Hua, et al. "A comparative dosimetric study for treating left-sided breast cancer for small breast size using five different radiotherapy techniques: Conventional tangential field, filed-in-filed, tangential-IMRT, multi-beam IMRT and VMAT." Radiation Oncology, Vol. 8, No. 1, 2013, pp. 1-8.
- Dumane, Vishruta A., Nisha Ohri, and Sheryl Green. "Volumetric-modulated arc therapy improved heart and lung sparing for a left-sided chest wall and regional nodal irradiation case." Applied Radiation Oncology, Vol. 6, No. 3, 2017, pp. 28-36.
- Cendales, Ricardo, et al. "Helical tomotherapy in patients with breast cancer and complex treatment volumes." Clinical and Translational Oncology, Vol. 13, No. 4, 2011, pp. 268-74.