Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 1
Diffuse Small Bowel Disease, Lupus Enteritis, as First Presentation of Systemic Lupus Erythematosus, Case Report
Abdullah Mohammed Albishi1*, Yahiya Ali Khobrani2, Faris Ayeth Alshahrani2, Yahia I. Assiri3, Nasser Ibraheem Alqahtani1, Khalid Tahir Ibrahim Suliman2 and Mohammed Qasem Alguthrudi22Internal Medicine Department, Armed Forces Hospital Southern Region, Khamis Mushayt, Saudi Arabia
3Radiology Department, College of Medicine, King Khalid University, Abha, Saudi Arabia
Abdullah Mohammed Albishi, Gastroenterology and Endoscopy Department, Armed Forces Hospital Southern Region, Khamis Mushayt, Saudi Arabia, Email: dr.abdullah6975@gmail.com
Received: 25-Nov-2020 Accepted Date: Jan 22, 2021 ; Published: 29-Jan-2021, DOI: O
Abstract
Systemic Lupus Erythematosus (SLE) is a chronic autoimmune inflammatory disease that has wide manifestations that affect many organs in the body. One rare complication of SLE in the Gastrointestinal Tract (GI) is lupus enteritis which is a complex of manifestations including enteric ischemia and intestinal vasculitis, which is characterized by abdominal pain, vomiting, and diarrhea. Hence, we are reporting one case of a middle-aged woman who suffered from abdominal pain for three months without any features suggestive of SLE. She was diagnosed with lupus enteritis which was the first initial presenting symptom for SLE
Keywords
Lupus, Enteritis, Bowel thickness, Abdominal pain, Initial
Introduction
SLE affects the gastrointestinal tract commonly; symptoms are usually related to infections or the medications’ side effects [1]. Lupus enteritis is defined as either vasculitis or small bowel inflammation. The clinical manifestation of lupus enteritis is often nonspecific, with mild to severe abdominal pain, diarrhea, and vomiting [2]. Lupus enteritis is a rare manifestation of SLE that affects 0.2% to 5.8% of these patients. Diagnosis of lupus enteritis clinically can be difficult, especially if no other symptoms suggest SLE [3]. We are reporting one case of a middle-aged woman who suffered from vague abdominal pain for three months without any features suggestive of SLE. She was diagnosed with lupus enteritis which was the first initial presenting symptom of SLE.
Case Report
A 37 years old Saudi female known to have a case of hypothyroidism on thyroxine replacement, was presented to the Emergency Room (ER) with a history of para-umbilical abdominal pain for 3 months which started gradually, intermittent, colic in nature, mainly after a fatty meal, mild to moderate in severity, lasting from minutes up to one hour, improving with fasting. This pain was associated with decreased appetite, nausea, and occasionally vomiting, and a history of two to three times passing loose stool. There was no history of jaundice, hematemesis, dysphagia, diarrhea, constipation, and rectal bleeding, fever, or weight loss.
The patient gave a history of recurrent attacks of epigastric abdominal pain for two years and was diagnosed that time as peptic ulcers secondary to H. pylori and treatment was given. After that, the patient still complained of the same abdominal pain despite the H. pylori eradication so she underwent upper GI endoscopy which showed signs of antral gastritis however, no masses or ulcers were seen.
The patient had a history of total tonsillectomy 18 years ago. There was no history of inherited or acquired diseases among her family; drugs or herbal use.
On Examination
At ER, she was unwell and in pain, fully conscious, oriented, not pale or jaundiced, and no lymphadenopathy.
Her vital signs were BP 116/57 mmHg, temperature 36.4°C, heart rate 71/min, 02 saturation 97% room air.
Chest and cardiovascular systems were normal.
The abdomen was soft, lax with mild para-umbilical tenderness and no guarding, no palpable mass, normal bowel sounds.
Lower limbs: no swelling or edema.
Labs
Blood gases and lactate levels were normal. Stool analysis was also normal. However, the tests for stool Helicobacter pylori were positive. Chest X-ray was usual (Table 1)
Table 1 Various diagnostic tests and their results performed on the patient
| CBC | |
| WBC | 3.4 |
| Hb | 12.1 |
| MCV | 79 |
| MCH | 24 |
| PLT | 294 |
| INR | 1 |
| LFTs | |
| Albumin | 34 |
| ALT | 13 |
| AST | 16 |
| Total bilirubin | 13.1 |
| direct bilirubin | 4.6 |
| Renal profile | |
| Urea | 3.9 |
| Creatinine | 63 |
| Chemistry | |
| Amylase | 79 |
| LDH | 124 |
| TSH | 2,4 |
| Vit D | 41.3 |
| CRP | 5 |
| ESR | 12 |
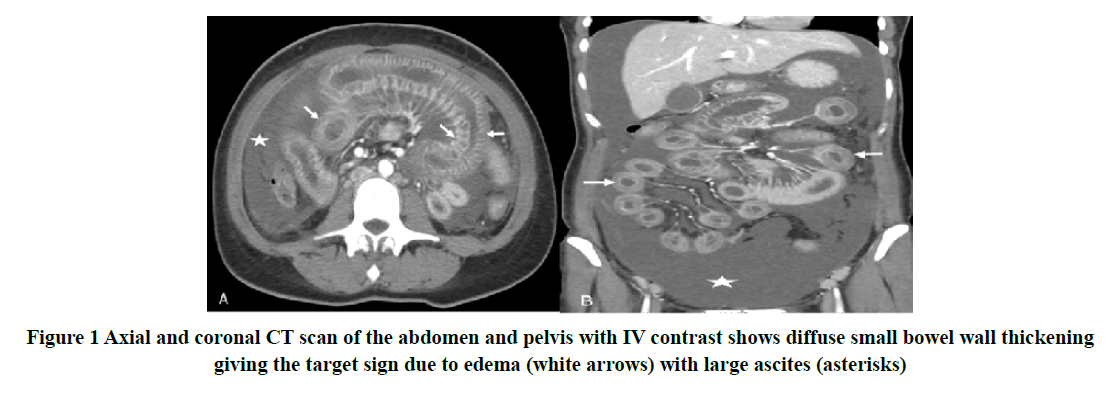
CT scan of the abdomen was done as shown in Figure 1 and reported as diffuse small bowel, with wall thickening giving the target sign due to edema with large ascites.
Upper GI endoscopy was done and showed mild erythematous gastric and duodenal mucosa. Duodenal biopsy histopathology was reported as mild to moderate non-specific chronic duodenitis. No significant villous architectural changes were observed. The patient was negative for intra-epithelial lymphocytosis. Gastric biopsy histopathology was reported as mild to moderate non-specific chronic gastritis. No H. pylori were seen.
Ascitic fluid tapping was done and showed low Serum-Ascites Albumin Gradient (SAAG) ascites. The ascitic fluid analysis showed WBC: 201, no organism was seen in gram stain, MTB (Mycobacterium tuberculosis) PCR was not detected. Cytology of ascitic fluid showed cellular mesothelial cell proliferation, no atypia. The cytological features favor reactive mesothelial cells.
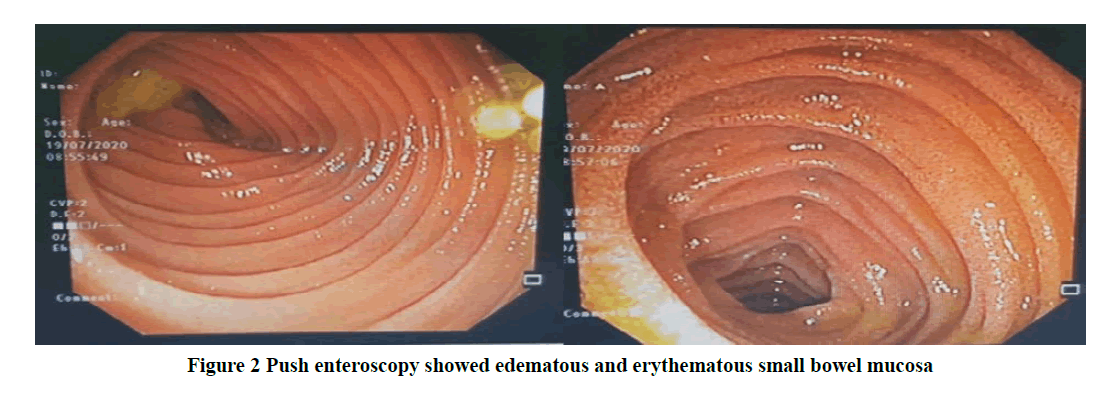
Push enteroscopy was done and showed edematous and erythematous small bowel mucosa as shown in Figure 2.
Small bowel biopsies histopathology showed superficial mucosa with non-specific chronic inflammation with lymphoplasma cells, mixed neutrophils, and a few eosinophils. No granuloma was seen. Small bowel tissue culture showed heavy growth, gastro-intestinal flora was isolated and, the results for MTB (Mycobacterium tuberculosis) PCR were negative.
Clinically, no history of hair loss, eye symptoms, oral ulcers, skin rash, joint pain, and any genital ulcers or urinary symptoms was reported.
Antinuclear Antibody (ANA) positive, dsDNA positive, RF: 8.38 μ/ml, CCP: 0.6 μ/ml, C3: 0.5 g/L, C4: 0.02 g/L.
ANA 1:5120, dsDNA >800 μ/ml, U1SNRNP abs 2 μ/ml, Anti-smith Abs 1 μ/ml, Anti-SSA >200 μ/ml, Anti-SSB 7 μ/ ml
So, the patient was diagnosed with lupus enteritis using Systemic Lupus International Collaboration Clinics Criteria. The patient was educated and instructed regarding her diagnosis and management plan. She started on hydroxychloroquine 200 mg orally twice daily with follow-up in the clinic after one month with new labs.
After one month, she was doing well, with no features suggestive of active lupus (clinically and biochemically).
Discussion
The systematic lupus erythematosus affects about 161000 to 322000 people in the United States. It affects multiple organs in the body, including the gastrointestinal system [3]. In around 50% of SLE patients, anorexia, nausea, and vomiting are the most frequent symptoms seen. These GI symptoms may be due to lupus itself as a result of bowel ischemia or medications side effects, or the coincidence of solely GI manifestations, such as gastritis, pancreatitis, cholecystitis, appendicitis [4]. The differential diagnosis for abdominal pain in systemic lupus erythematosus patient is so wide and can include infection, serositis, pancreatitis, vasculitis, gluten enteropathy, protein-losing enteropathy, intestinal pseudo-obstruction. The lupus enteritis pathology is thought to be complement activation and immune complex deposition, with submucosal edema [5]. Table 2 shows the differential diagnosis of abdominal pain in SLE patients [6].
Table 2 Differential diagnosis of abdominal pain in SLE patient
| Non-SLE related | SLE related |
|---|---|
| Appendicitis | Lupus enteritis |
| Lithiasis cholecystitis | Pancreatitis |
| Peptic Ulcer | Pseudo-obstruction |
| Acute pancreatitis | Acalculous cholecystitis |
| Retroperitoneal hematoma | Mesenteric thrombosis |
| Ovarian pathology | Hepatic thrombosis |
| Diverticulitis | Medication (NSAIDs, MMF, steroids, HCQ) |
| Adhesions, intestinal occlusion | Colon perforation (vasculitis) |
| Infectious enteritis | |
| Pyelonephritis | |
| CMV colitis |
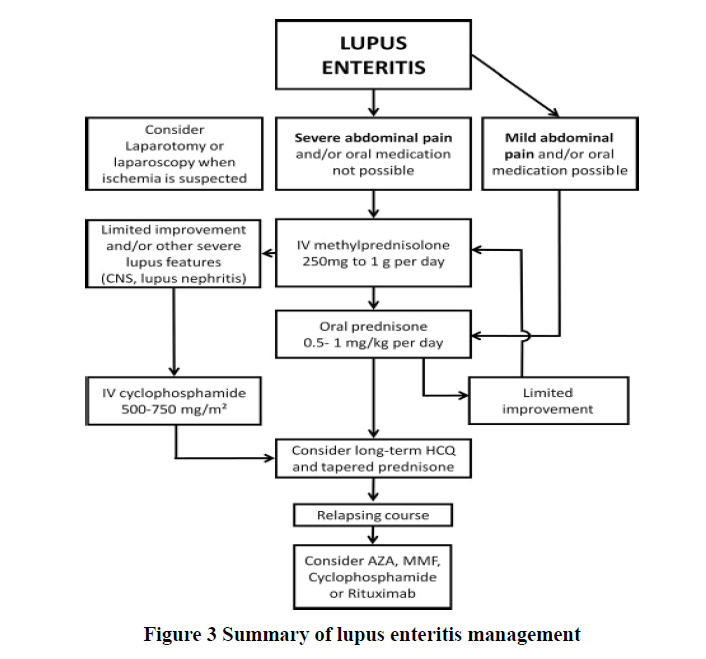
Clinical presentation of lupus enteritis is nonspecific, and usually, the main symptoms include localized or diffuse abdominal pain, vomiting, diarrhea, and fever [7]. It presents with very non-specific signs and symptoms, such as abdominal pain (97%), ascites (78%), nausea (49%), vomiting (42%), diarrhea (32%), and fever (20%) [3]. Lupus enteritis is considered as a form of visceral vasculitis involving mainly the jejunum and ileum, with subsequent submucosal edema [1]. Lupus enteritis leads to three important imaging signs on abdominal CT: (1) bowel wall thickening of greater than 3 mm (target sign) and dilatation of intestinal segments, (2) engorgement of mesenteric vessels (“comb sign”), and (3) increased attenuation of mesenteric fat [5]. Typically, lupus enteritis is steroid-responsive and carries an excellent prognosis and usually, immunosuppressive treatment is reserved for recurrent enteritis or severe SLE cases [2]. Figure 3 shows a summary of important points in the management of lupus enteritis patients [6].
Lupus enteritis is seen in only 13% of patients without a previous SLE diagnosis [3].
The complications of lupus enteritis include mesenteric vasculitides, protein-losing enteropathies, and intestinal pseudo- obstruction. It can be a surgical emergency secondary to perforation and intestinal necrosis [8].
Conclusion
Lupus enteritis is very rare as an initial first presentation of active SLE. Diagnosis requires a combination of clinical symptoms, laboratory testing, and imaging. High index suspicion needs early diagnosis and appropriate treatment otherwise the complication rate will be high sometimes considered as a surgical emergency. Management of lupus enteritis generally depends on the severity and carries a good prognosis.
Declerations
Conflicts of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- Gustafson, David, and Osvaldo Padilla. "Characteristics of Adenocarcinoma of the Gallbladder Following Cholecystectomies in the Hispanic Population." American Journal of Clinical Pathology, Vol. 152, No. Supplement_1, 2019, pp. S64-65.
- Sran, Sisira, et al. "Lupus enteritis as an initial presentation of systemic lupus erythematosus." Case Reports in Gastrointestinal Medicine, Vol. 2014, 2014.
- Lavanchy, Pierrette. "Clinical cases." Psychotherapy and Human Sciences, Vol. 53, No. 2, 2019, pp. 327-30.
- Lin, Hsien-Ping, Yao-Ming Wang, and An-Ping Huo. "Severe, recurrent lupus enteritis as the initial and only presentation of systemic lupus erythematosus in a middle-aged woman." Journal of Microbiology, Immunology and Infection, Vol. 44, No. 2, 2011, pp. 152-55.
- Aiyappan, Senthil Kumar, and Akilesh Suvindran. "Lupus enteritis." The Pan African Medical Journal, Vol. 33, 2019, p. 205.
- Janssens, Peter, et al. "Lupus enteritis: from clinical findings to therapeutic management." Orphanet Journal of Rare Diseases, Vol. 8, No. 1, 2013, pp. 1-10.
- Demiselle, Julien, et al. "An Unusual Cause of Abdominal Pain: Lupus Enteritis." The American Journal of Medicine, Vol. 129, No. 5, 2016, pp. e11-12.
- Ronen, Joshua A., et al. "A Flare-up of Systemic Lupus Erythematosus with Unusual Enteric Predominance." Cureus, Vol. 12, No. 2, 2020, p. e7068.